NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Tacrine is an oral acetylcholinesterase inhibitor previously used for therapy of Alzheimer disease. Tacrine therapy is associated with a very high rate of serum aminotransferase elevations during therapy and has been linked to several instances of clinically apparent, acute liver injury.
Background
Tacrine (tak' reen) was the first acetylcholinesterase inhibitor introduced into clinical use for management of Alzheimer disease. Tacrine acts by inhibiting the metabolism of acetylcholine and thus prolonging its activity and raising levels in the cerebral cortex. Therapy with tacrine improves mental functioning in patients with mild-to-moderate dementia of Alzheimer disease. Tacrine was approved for use in the United States in 1993 as therapy of mild-to-moderate dementia of the Alzheimer type. Tacrine was marketed in capsules of 10, 20, 30 and 40 mg under the brand name Cognex with the typical dose being 20 to 40 mg four times daily. Tacrine has dose limiting side effects including diarrhea, nausea, vomiting, abdominal discomfort, dizziness, headache, anxiety, blurred vision, dry mouth and insomnia, symptoms typical of cholinergic stimulation. Because of continuing concerns over safety and availability of other acetylcholinesterase inhibitors, tacrine was withdrawn from use in 2013.
Hepatotoxicity
Strikingly, therapy with tacrine was associated with serum aminotransferase elevations in almost half of patients. These elevations usually arose within 6 to 8 weeks of starting therapy and rapidly resolved when therapy was stopped. Elevations above 3 times the upper limit of the normal range (ULN) occurred in 25%, above 10 times ULN in 6% and above 20 times ULN in 2% of patients. Accompanying elevations in alkaline phosphatase and bilirubin were rare, and the ALT abnormalities were usually asymptomatic and resolved rapidly when therapy was stopped or with dose reduction. Monitoring of serum aminotransferase levels during tacrine therapy was recommended, with dose modification for ALT elevations above 3 times the ULN and discontinuation if levels rose above 5 times the ULN. In prelicensure studies, no instances of clinically apparent acute liver injury with jaundice were reported. Subsequently, however, several cases of acute hepatocellular injury with jaundice attributed to tacrine were reported, generally arising within 2 to 8 weeks of starting therapy and usually resolving rapidly with discontinuation. Eosinophilia often accompanied the hepatic injury due to tacrine, but rash and fever were uncommon as were autoantibodies. Rechallenge often led to recurrence of the hepatic injury with a somewhat shorter latency but similar or milder course. In many patients, the serum aminotransferase elevations resolved even without drug discontinuation or dose modification. Nevertheless, fatal cases of liver injury attributed to tacrine were reported to the sponsor. Routine monitoring of serum aminotransferase levels for the first six months of therapy was recommended. However, the availability of other oral anticholinesterase inhibitors that are given only once or twice daily, do not require ALT monitoring and only rarely cause liver enzyme elevations has led to the withdrawal of tacrine from clinical use in the United States.
Likelihood score: A (well established cause of liver injury, although usually marked by serum aminotransferase elevations without symptoms or jaundice).
Mechanism of Injury
Tacrine undergoes first pass metabolism by the liver and is extensively metabolized by the cytochrome P450 system. The hepatotoxicity of tacrine is probably related to production of a toxic intermediate, but the precise mechanism of injury is not known. Intestinal bacteria (the “microbiome”) may play a role in tacrine hepatotoxicity in that impaired glucuronidation caused by changes in intestinal bacterial flora is associated with aminotransferase elevations in rodents exposed to tacrine.
Outcome and Management
The hepatotoxicity of tacrine is usually marked by transient and asymptomatic, moderate-to-severe elevations in serum aminotransferase levels that resolve rapidly with discontinuation. More severe instances of hepatotoxicity with symptoms and jaundice have been reported but are rare. Tacrine has not been linked to cases of chronic hepatitis or vanishing bile duct syndrome, at least in the published literature. The safety of switching to another acetylcholinesterase inhibitor after tacrine hepatotoxicity has not been shown, but there is little reason to suspect that cross sensitivity exists.
References regarding the safety and potential hepatotoxicity of the drugs used for Alzheimer disease are provided below for tacrine and again for all agents after the overview section of Alzheimer Disease Agents.
Drug Class: Alzheimer Disease Agents
CASE REPORT
Case 1. Acute hepatocellular injury with jaundice during tacrine therapy.(1)
A 76 year old woman developed fever and jaundice 20 days after starting tacrine in a therapeutic trial of this drug for Alzheimer disease. She had no previous history of liver disease, drug reactions, alcohol abuse or risk factors for viral hepatitis. She was taking no other medications. The dose of tacrine had been increased from 25 to 100 mg during the first 5 days of therapy, but was then reduced to 75 mg because of headaches. When jaundice was noted, tacrine was discontinued promptly and two days later she was admitted for evaluation. On examination, she was afebrile and anicteric. Blood tests showed a total serum bilirubin of 4.1 mg/dL with marked elevations in ALT (~1700 U/L) and minimal increases in alkaline phosphatase levels (~130 U/L). Liver tests had been normal before tacrine was started and were still normal on day 12 of therapy (Table). The prothrombin index was slightly decreased (70%) and eosinophil counts were normal. Tests for hepatitis A and B were negative as were autoantibodies. Ultrasound of the abdomen showed a normal liver and biliary tract. A liver biopsy showed centrilobular necrosis and mild inflammatory infiltrates with no cholestasis and no fibrosis. Serum ALT levels peaked one day after admission and fell rapidly thereafter, becoming normal within the next 5 weeks.
Key Points
| Medication: | Tacrine (75 mg daily) |
|---|---|
| Pattern: | Hepatocellular (R=42) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | 3 weeks |
| Recovery: | 5 weeks |
| Other medications: | None |
Laboratory Values
| Time After Starting | Time After Stopping | ALT* (U/L) | Alk P* (U/L) | Bilirubin* (mg/dL) | Other |
|---|---|---|---|---|---|
| -1 day | Pre | 30 | 105 | 0.7 | |
| 12 days | 0 | 35 | 100 | 0.7 | |
| 20 days | 0 | 1700 | 130 | 4.1 | Fever and jaundice |
| 22 days | 0 | 2200 | 135 | 1.2 | Tacrine stopped |
| 4 weeks | 5 days | 799 | 195 | 0.5 | Liver biopsy |
| 5 weeks | 2 weeks | 80 | 110 | 0.6 | |
| 8 weeks | 5 weeks | 30 | 95 | 0.5 | Fully recovered |
| Normal Values | <40 | <130 | <1.2 | ||
- *
Values estimated from Figure 1.
Comment
Tacrine is well known to be associated with serum aminotransferase elevations which usually arise within 3 to 8 weeks of starting therapy. These elevations can be marked (>20 times ULN), but are typically self-limited and asymptomatic. This patient was unusual only because she developed jaundice and symptoms. The rapid resolution of injury upon stopping tacrine is typical. Despite the frequency of this abnormality, tacrine hepatotoxicity is usually mild and self limited. No cases of fatal tacrine induced liver injury have been reported in the literature, although such cases have evidently been reported to the sponsor.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Tacrine – Cognex®
DRUG CLASS
Alzheimer Disease Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Tacrine | 321-64-2 | C13-H14-N2 |
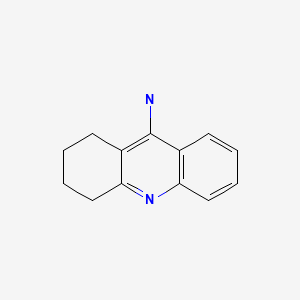
|
CITED REFERENCE
- 1.
- Hammel P, Larrey D, Bernuau J, Kalafat M, Fréneaux E, Babany G, Degott C, et al. Acute hepatitis after tetrahydroaminoacridine administration for Alzheimer's disease. J Clin Gastroenterol. 1990;12:329–31. [PubMed: 2362104]
ANNOTATED BIBLIOGRAPHY
References updated: 15 January 2020
- Zimmerman HJ. Miscellaneous drugs and diagnostic chemicals. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 709-42.(Expert review of hepatotoxicity published in 1999; tacrine, the first cholinesterase inhibitor approved for use in Alzheimer disease, was associated with a very high rate of serum ALT elevations [~50%], but rarely caused clinically apparent liver injury; the other Alzheimer disease agents are not discussed).
- Larrey D, Ripault MP. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 518.(Review of hepatotoxicity of psychotropic agents ; drugs for Alzheimer disease are not specifically discussed).
- Roberson ED. Alzheimer's disease. Treatment of central nervous system degenerative disorders. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 333-5.(Textbook of pharmacology and therapeutics).
- Chatellier G, Lacomblez L. Tacrine (tetrahydroaminoacridine; THA) and lecithin in senile dementia of the Alzheimer type: a multicentre trial. Groupe Françs d'Etude de la Tetrahydroaminoacridine. BMJ. 1990;300:495–9. [PMC free article: PMC1662308] [PubMed: 2107926](In a randomized controlled crossover trial of tacrine in 67 patients with Alzheimer disease, 9 patients [13%] developed significant ALT or AST elevations, usually arising after 2-8 weeks of therapy, ALT 85-2115 U/L, one patient developed jaundice which resolved within 3-4 weeks of stopping).
- Ames DJ, Bhathal PS, Davies BM, Fraser JR, Gibson PR, Roberts S. Heterogeneity of adverse hepatic reactions to tetrahydroaminoacridine. Aust N Z J Med. 1990;20:193–5. [PubMed: 2344330](5 of 14 patients [36%] taking tacrine for Alzheimer disease developed abnormal liver tests [ALT 106-422 U/L, GTT 20-71 U/L, bilirubins normal], one was symptomatic; liver biopsies showed focal necrosis, fat and one patient with granulomas; all resolved with stopping the drug or lowering the dose).
- Hammel P, Larrey D, Bernuau J, Kalafat M, Fréaux E, Babany G, Degott C, et al. Acute hepatitis after tetrahydroaminoacridine administration for Alzheimer's disease. J Clin Gastroenterol. 1990;12:329–31. [PubMed: 2362104](A 76 year old woman with Alzheimer disease developed fever and jaundice 20 days after starting tacrine [bilirubin 5.0 mg/dL, ALT ~1800 U/L, Alk P 125 U/L, prothrombin index 40%], with rapid resolution on stopping, all liver tests falling to normal within 6 weeks).
- O'Brien JT, Eagger S, Levy R. Effects of tetrahydroaminoacridine on liver function in patients with Alzheimer's disease. Age Ageing. 1991;20:129–31. [PubMed: 2053502](Prospective analysis of liver tests in 30 patients with Alzheimer disease treated with tacrine; 50% developed AST elevations within 17-38 days, 8 had clinical symptoms but none had jaundice, all resolved within 3-23 days after stopping or dose reduction; 6 were restarted and 5 tolerated therapy long term).
- Farlow M, Gracon SI, Hershey LA, Lewis KW, Sadowsky CH, Dolan-Ureno J. A controlled trial of tacrine in Alzheimer's disease. The Tacrine Study Group. JAMA. 1992;268:2523–9. [PubMed: 1404819](Among 468 patients with Alzheimer disease treated with tacrine or placebo, ALT elevations [>3 times ULN] occurred in 25% of tacrine treated, but in none of placebo treated patients; all elevations were reversible and asymptomatic, usually arising in the first 8 weeks of treatment and resolving within 7-71 days of stopping).
- Knapp MJ, Knopman DS, Solomon PR, Pendlebury WW, Davis CS, Gracon SI. A 30-week randomized controlled trial of high-dose tacrine in patients with Alzheimer's disease. The Tacrine Study Group. JAMA. 1994;271:985–91. [PubMed: 8139083](In a randomized controlled trial of tacrine vs placebo in 653 patients with Alzheimer disease, some degree of ALT elevation occurred in 54% and elevations >3 times ULN in 28% of tacrine treated patients, but no patient had jaundice and most were asymptomatic, all resolved on stopping tacrine).
- Watkins PB, Zimmerman HJ, Knapp MJ, Gracon SI, Lewis KW. Hepatotoxic effects of tacrine administration in patients with Alzheimer's disease. JAMA. 1994;271:992–8. [PubMed: 8139084](In depth analysis of liver test abnormalities occurring in 2446 patients on tacrine in multi-center trials; ALT elevations occurred in 49%, were >3 times ULN in 25%, >10 times ULN 6%, and >20 times ULN in 2%, usually arising within 6-8 weeks of starting, with no symptoms or minimal nausea and fatigue even when ALT >10 times ULN, eosinophilia in 23-44% but no rash, more rapid but less severe recurrence on rechallenge, nevertheless 88% could continue tacrine; more common in women than men).
- Gracon SI, Knapp MJ, Berghoff WG, Pierce M, DeJong R, Lobbestael SJ, Symons J, et al. Safety of tacrine: clinical trials, treatment IND, and postmarketing experience. Alzheimer Dis Assoc Disord. 1998;12:93–101. [PubMed: 9651138](Review of safety including hepatotoxicity of tacrine based upon registration trials and postmarketing adverse event reporting; ALT levels rise to >3 times the ULN in at least 25% of patients but are usually asymptomatic and not associated with jaundice).
- Barbare JC, Imbert A, Benkirane A. [Recent developments concerning drug- induced liver toxicity]. Presse Med 2001; 30: 673-6. French. PMID: 11360729. [PubMed: 11360729](Review of importance of central reporting of drug induced liver injury, providing examples of recently described hepatotoxic reactions, including 3 recent cases of hepatocellular injury due to riluzole).
- Farlow MR, Cummings JL. Effective pharmacologic management of Alzheimer's disease. Am J Med. 2007;120:388–97. [PubMed: 17466645](Review of safety and efficacy of medications for Alzheimer disease; no discussion of hepatotoxicity).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008; none were attributed to a drug used to treat Alzheimer disease).
- Mayeux R. Early Alzheimer's disease. N Engl J Med. 2010;362:2194–201. [PubMed: 20558370](Case discussion and review of current understanding of Alzheimer disease including role of therapy; common side effects of cholinesterase inhibitors include nausea, vomiting, anorexia, diarrhea, dizziness, muscle cramps, insomnia and vivid dreams; memantine can cause constipation, dizziness, headache and body pains; no mention of hepatotoxicity).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none were attributed to drugs used to treat Alzheimer disease).
- Tricco AC, Soobiah C, Berliner S, Ho JM, Ng CH, Ashoor HM, Chen MH, Hemmelgarn B, Straus SE. Efficacy and safety of cognitive enhancers for patients with mild cognitive impairment: a systematic review and meta-analysis. CMAJ. 2013 Nov 5;185(16):1393–401. [PMC free article: PMC3826344] [PubMed: 24043661](Systematic review of 8 clinical trials and 3 reports on the safety and efficacy of Alzheimer drugs mentions that side effects of nausea, diarrhea, vomiting and headaches were usually more frequent with the active drugs compared to placebo; no mention of ALT elevations or clinically apparent liver injury).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none of the cases were attributed to a drug used to treat Alzheimer disease).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Among 176 reports of drug induced liver injury from Latin America published between 1996 and 2012, none were attributed to a drug for Alzheimer disease).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, none were due to a drug for Alzheimer disease).
- Kröger E, Mouls M, Wilchesky M, Berkers M, Carmichael PH, van Marum R, Souverein P, et al. Adverse drug reactions reported with cholinesterase inhibitors: an analysis of 16 years of individual case safety reports from VigiBase. Ann Pharmacother. 2015;49:1197–206. [PubMed: 26324356](Analysis of spontaneous adverse event reports made between 2006 and 2013 to a WHO drug monitoring database identified 16,995 serious adverse events in patients receiving cholinesterase inhibitors, 121 of which were hepatobiliary, including 47 for donepezil, 53 rivastigmine and 21 galantamine; no details provided).
- Mohammad D, Chan P, Bradley J, Lanctôt K, Herrmann N. Acetylcholinesterase inhibitors for treating dementia symptoms - a safety evaluation. Expert Opin Drug Saf. 2017;16:1009–19. [PubMed: 28678552](Review of safety of donepezil, galantamine and rivastigmine in Alzheimer disease concludes that adverse events are “generally mild”, mostly gastrointestinal, comparable among the different agents, but usually greater with higher doses and less with transdermal formulations).
- Yip LY, Aw CC, Lee SH, Hong YS, Ku HC, Xu WH, Chan JMX, et al. The liver-gut microbiota axis modulates hepatotoxicity of tacrine in the rat. Hepatology. 2018;67:282–95. [PubMed: 28646502](In Lister hooded rats, tacrine administration resulted in variable increases in ALT and AST with higher levels correlating with higher systemic exposure, which could be modified by changing the intestinal bacterial flora [microbiome], which was likely the result of bacterial deglucuronidation of tacrine during enterohepatic recycling).
- Dou KX, Tan MS, Tan CC, Cao XP, Hou XH, Guo QH, Tan L, et al. Comparative safety and effectiveness of cholinesterase inhibitors and memantine for Alzheimer's disease: a network meta-analysis of 41 randomized controlled trials. Alzheimers Res Ther. 2018;10:126. [PMC free article: PMC6309083] [PubMed: 30591071](Meta-analysis of 41 published randomized controlled trials of drugs for Alzheimer disease concluded that all had beneficial effects on cognition and function but not on neuropsychiatric symptoms, and all had adverse effects but memantine showed “the best profile of acceptability”; no mention of ALT elevations or hepatotoxicity).
- Khoury R, Rajamanickam J, Grossberg GT. An update on the safety of current therapies for Alzheimer's disease: focus on rivastigmine. Ther Adv Drug Saf. 2018;9:171–8. [PMC free article: PMC5810854] [PubMed: 29492246](Review of the safety of Alzheimer disease agents discusses gastrointestinal adverse events, cardiac side effects, skin reactions [to transdermal formulations] and neuropsychiatric effects, but not hepatic adverse events).
- Bhattacharjee S, Patanwala AE, Lo-Ciganic WH, Malone DC, Lee JK, Knapp SM, Warholak T, Burke WJ. Alzheimer's disease medication and risk of all-cause mortality and all-cause hospitalization: A retrospective cohort study. PMID: Alzheimers Dement (N Y). 2019;5:294–302. [PMC free article: PMC6626065] [PubMed: 31338414](Among more than 20,000 Medicare beneficiaries receiving Alzheimer disease drugs, overall survival was better for those on donepezil than memantine or rivastigmine; no mention of serious hepatic adverse events or liver related deaths).
- Carney G, Bassett K, Wright JM, Maclure M, McGuire N, Dormuth CR. Comparison of cholinesterase inhibitor safety in real-world practice. Alzheimers Dement (NY). 2019;5:732–9. [PMC free article: PMC6944712] [PubMed: 31921965](Among 29,047 Canadian patients with Alzheimer disease who initiated anticholinesterase therapy between 2007 and 2016, all cause mortality and serious cardiovascular event rates were lower in those receiving galantamine than those on donepezil; no mention of hepatic adverse events or liver related deaths).
- Matsunaga S, Fujishiro H, Takechi H. Efficacy and safety of cholinesterase inhibitors for mild cognitive impairment: a systematic review and meta-analysis. J Alzheimers Dis. 2019;71:513–23. [PubMed: 31424411](Systematic review of 14 randomized controlled trials of anticholinesterase drugs in Alzheimer disease concluded that the agents had slight efficacy in ameliorating symptoms but a moderate rate of discontinuation because of adverse events such as abnormal dreams, dizziness, headache, insomnia, diarrhea, muscle cramps, nausea and weight loss; no mention of discontinuations because of ALT elevations or hepatotoxicity).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Safety of tacrine: clinical trials, treatment IND, and postmarketing experience.[Alzheimer Dis Assoc Disord. 1998]Safety of tacrine: clinical trials, treatment IND, and postmarketing experience.Gracon SI, Knapp MJ, Berghoff WG, Pierce M, DeJong R, Lobbestael SJ, Symons J, Dombey SL, Luscombe FA, Kraemer D. Alzheimer Dis Assoc Disord. 1998 Jun; 12(2):93-101.
- Review Alzheimer Disease Agents.[LiverTox: Clinical and Researc...]Review Alzheimer Disease Agents.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Tacrine, an oral acetylcholinesterase inhibitor, induced hepatic oxidative damage, which was blocked by liquiritigenin through GSK3-beta inhibition.[Biol Pharm Bull. 2015]Tacrine, an oral acetylcholinesterase inhibitor, induced hepatic oxidative damage, which was blocked by liquiritigenin through GSK3-beta inhibition.Park SM, Ki SH, Han NR, Cho IJ, Ku SK, Kim SC, Zhao RJ, Kim YW. Biol Pharm Bull. 2015; 38(2):184-92.
- Hepatotoxic effects of tacrine administration in patients with Alzheimer's disease.[JAMA. 1994]Hepatotoxic effects of tacrine administration in patients with Alzheimer's disease.Watkins PB, Zimmerman HJ, Knapp MJ, Gracon SI, Lewis KW. JAMA. 1994 Apr 6; 271(13):992-8.
- Review Tacrine: a pharmacological approach to Alzheimer's disease.[J Psychosoc Nurs Ment Health S...]Review Tacrine: a pharmacological approach to Alzheimer's disease.Keltner NL. J Psychosoc Nurs Ment Health Serv. 1994 Mar; 32(3):37-9.
- Tacrine - LiverToxTacrine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...