NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Plicamycin, which was formerly known as mithramycin, is an antibiotic that is used as an anticancer agent in the therapy of testicular and germ cell cancers. Plicamycin causes acute hepatic injury that arises within days of starting therapy, but is usually transient and asymptomatic and rarely leads to jaundice. Plicamycin has not been approved for use as cancer chemotherapy in the United States, but continues to be used on an investigational basis.
Background
Plicamycin (plye” ka mye’ sin), which was formerly known as mithramycin, is an antineoplastic antibiotic that was first isolated from fermentation extracts of Streptomyces plicatus. It acts by binding to helical double-stranded DNA and blocking RNA synthesis. It has potent antitumor effects in vitro and has been evaluated in several solid tumors in humans. Because of its toxicities (including hepatotoxicities), it has not been approved for use in the United States. Nevertheless, plicamycin has distinctive and sometimes potent activities against germ cell and testicular cancers and continues to be investigated as an experimental therapy in patients with advanced and resistant forms of cancer. Plicamycin is also effective in reducing hypercalcemia associated with malignancy, probably by inhibition of osteoblast function, but its use has been replaced by less toxic approaches such as corticosteroids and bisphosphonates. For the treatment of cancer, plicamycin is administered intravenously in doses of 25 to 50 μg/kg daily for 5 to10 days in 2 to 6 monthly courses. Side effects of plicamycin are common and often dose limiting, including bone marrow suppression, irritability, agitation, gastrointestinal upset, diarrhea, nausea, anorexia, weakness, fever, rash, epistaxis, bruising and hemorrhage.
Hepatotoxicity
Chemotherapy with plicamycin causes serum enzyme elevations in almost all patients who are treated for more than 1 or 2 days and who are monitored during therapy. Serum ALT, AST and LDH values begin to rise within 3 days of the first infusion and peak within 7 to 10 days at levels of 5 to 500 times the upper limit of the normal range (ULN). The elevations, however, are transient and resolve within 1 to 3 weeks and are rarely associated with symptoms or jaundice. Liver biopsies taken during these episodes usually demonstrate centrolobular necrosis and congestion. With repeated courses, elevations continue to occur generally to the same or lesser degree. A single instance of acute liver failure arising within days of therapy that was suggestive of ischemic hepatitis or sinusoidal obstruction syndrome has been reported in a patient treated with full doses of plicamycin for 4 days for nonmalignant hypercalcemia. Otherwise, the serum enzyme elevations, despite being moderate to severe, are transient and benign.
Likelihood score: A[HD] (well known cause of clinically apparent liver injury with high dose intravenous treatment).
Mechanism of Injury
Plicamycin appears to be a direct, intrinsic hepatotoxin as the injury can be produced in animal models and occurs in almost all patients. The injury is likely to be dose related and is not more severe or more rapid in onset with rechallenge. Experimental studies suggest that the hepatotoxicity of plicamycin relates to inhibition of farnesoid X receptor signaling leading to deregulation of bile acid homeostasis.
Outcome and Management
The hepatic injury caused by plicamycin is usually reversible and requires no intervention. The hepatotoxicity of plicamycin has limited its usefulness, and it is considered contraindicated in patients with significant underlying liver disease.
Drug Class: Antineoplastic Agents
Other Drugs in the Subclass, Antibiotics, Cytotoxic: Bleomycin, Dactinomycin, Daunorubicin, Doxorubicin, Epirubicin, Idarubicin, Mitomycin, Mitoxantrone
CASE REPORT
Case 1. Marked serum aminotransferase elevations during intravenous therapy with plicamycin.(1)
A 63 year old man with intrathoracic mesothelioma participating in a phase II clinical trial at the Clinical Center of the National Institutes of Health was started on intravenous plicamycin (25 mcg/kg/day) and developed marked serum aminotransferase elevations within 2 days. He had no history of liver disease, alcohol abuse or known drug allergies and was known to have normal liver tests before starting treatment. He had no symptoms of liver injury and was not receiving other medications. ALT levels peaked at 4832 U/L and AST levels at 4889 U/L a day after stopping therapy and then fell promptly (Table). Tests for hepatitis A, B and C were negative as were routine autoantibodies. Ultrasound of the liver suggested heterogeneity of the liver texture, but showed no other abnormalities, liver masses or evidence of obstruction. A liver biopsy showed centrolobular (zone 3) necrosis and hemorrhage with mild inflammation and no fibrosis or steatosis. After his serum enzymes returned to normal, he was rechallenged with a lower dose of plicamycin (18 mcg/kg/day) and serum aminotransferase levels again rose within a few days, but to a lesser degree (peak ALT 454 U/L). No further therapy with plicamycin was given.
Key Points
| Medication: | Plicamycin |
|---|---|
| Pattern: | Hepatocellular (R=193) |
| Severity: | 1+ (never jaundiced) |
| Latency: | 3 days |
| Recovery: | Complete recovery within 4 weeks |
| Other medications: | None |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Comments |
|---|---|---|---|---|---|
| Pre | Pre | 32 | 85 | 0.3 | Plicamycin started, INR 0.94 |
| 1 day | Pre | 37 | 68 | 0.6 | INR 0.89 |
| 2 days | Pre | 48 | 73 | 0.3 | |
| 3 days | 0 | 714 | 75 | 0.3 | Ultrasound |
| 4 days | 1 day | 4832 | 71 | 0.6 | LDH 5995 U/L, liver biopsy |
| 5 days | 2 days | 3510 | 72 | 0.9 | INR 1.23 |
| 6 days | 3 days | 2144 | 155 | 0.9 | |
| 7 days | 4 days | 1522 | 193 | 0.7 | |
| 1 month | 26 days | 37 | 80 | 0.6 | Plicamycin restarted |
| [3 days] | 142 | 86 | 0.2 | INR 0.99 | |
| [5 days] | 454 | 126 | 0.4 | ||
| Normal Values | <42 | <115 | <1.2 | ||
Comment
The serial test results demonstrated the typical pattern of serum enzyme elevations with plicamycin therapy. The pattern is that of acute hepatic necrosis and is self-limited if therapy is stopped promptly. In this clinical trial, 10 of 12 treated patients developed hepatotoxicity with a pattern similar to the one shown. No patient developed jaundice, and symptoms, when present, were mild and nonspecific (mild nausea and abdominal discomfort).
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Plicamycin – Generic, Mithracin®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Plicamycin | 18378-89-7 | C52-H76-O24 |
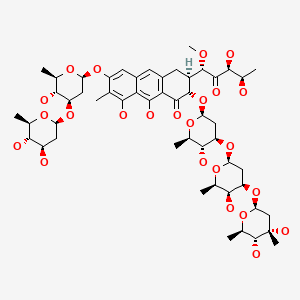
|
CITED REFERENCE
- 1.
- Sissung TM, Huang PA, Hauke RJ, McCrea EM, Peer CJ, Barbier RH, Strope JD, et al. Severe hepatotoxicity of mithramycin therapy caused by altered expression of hepatocellular bile transporters. Mol Pharmacol. 2019;96:158–67. [PMC free article: PMC6608607] [PubMed: 31175181]
ANNOTATED BIBLIOGRAPHY
References updated: 19 February 2020
- Zimmerman HJ. Antibiotics. Hepatotoxic effects of oncotherapeutic and immunosuppressive agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 694-8.(Expert review of hepatotoxicity published in 1999 mentions that mithramycin [plicamycin] is "highly toxic" and that hepatic injury occurs in 25-100% of patients, and is marked by very high elevations in ALT levels).
- DeLeve LD. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 541-68.(Review of hepatotoxicity of cancer chemotherapeutic agents mentions that mithramycin hepatotoxicity is uncommon with dosing used for hypercalcemia, but frequent with daily dosing used in cancer).
- Wellstein A, Giaccone G, Atkins MB, Sausville EA. Cytotoxic agents. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1167-203.(Textbook of pharmacology and therapeutics).
- Kofman S, Medrek TJ, Alexancer RW. Mithramycin in the treatment of embryonal cancer. Cancer. 1964;17:938–48. [PubMed: 14179556](Retrospective analysis of 26 patients with embryonic cell cancers treated with plicamycin found dramatic responses in a few patients, but therapy was limited by toxicities, largely to the bone marrow, no mention of hepatotoxicity).
- Brown JH, Kennedy BJ. Mithramycin in the treatment of disseminated testicular neoplasms. N Engl J Med. 1965;272:111–8. [PubMed: 14224214](Among 12 patients with testicular cancer treated with 2 to 6 courses of plicamycin, 7 had objective regression, all had hepatotoxicity with ALT rising after 3-5 days to as high as 21,000 U/L, then resolving with no jaundice and no deaths from liver disease).
- Morrison RK, Brown DE, Oleson JJ. A toxicologic study of mithramycin. Toxicol Appl Pharmacol. 1967;11:468–81. [PubMed: 4968193](In monkeys and dogs, doses of plicamycin of 0.1 mcg/kg caused marked serum ALT elevations within 5-7 days).
- Ream NW, Perlia CP, Wolter J, Taylor SG 3rd. Mithramycin therapy in disseminated germinal testicular cancer. JAMA. 1968;204:1030–6. [PubMed: 5694748](Among 30 patients with disseminated testicular cancer treated with plicamycin, 9 had an objective response, ALT elevations occurred with each course but returned to normal within 2-3 weeks and no patient developed jaundice; autopsy in 1 patient showed "toxic fatty metamorphosis").
- Ansfield FJ. Clinical studies with mithramycin. Oncology. 1969;23:283–8. [PubMed: 5817464](Among 46 patients with various solid tumors treated with plicamycin [78 courses] in varying doses, moderate-to-severe toxicity occurred in all and 4 patients died; 11 of 22 patients who were monitored had ALT elevations, but all reversed within 1 month).
- Ryan WG, Schwartz TB, Northrop G. Experiences in the treatment of Paget's disease of bone with mithramycin. JAMA. 1970;213:1153–7. [PubMed: 5468261](Among 15 patients with Paget disease of bone treated with plicamycin, serum enzyme elevations occurred, the most sensitive enzyme being isocitric dehydrogenase [ICD], which rose up to 160 times ULN).
- Kennedy BJ. Metabolic and toxic effects of mithramycin during tumor therapy. Am J Med. 1970;49:494–503. [PubMed: 4320120](Among 58 patients with advanced cancers treated with plicamycin, side effects were common including malaise, gastrointestinal upset, fever, headache, irritability, agitation, rash, stomatitis, epistaxis and hemorrhage; ALT or AST elevations occurred in all [up to 8,000 U/L], usually resolving rapidly).
- Kennedy BJ. Mithramycin therapy in advanced testicular neoplasms. Cancer. 1970;26:755–66. [PubMed: 5506598](Among 44 patients with advanced testicular cancer treated with plicamycin, alternate day regimens were more effective and less toxic than standard daily regimens of administration, but all patients had transient LDH elevations during therapy).
- Foley JF, Lemon HM, Miller DM, Kessinger A. The treatment of metastatic testicular tumors. J Urol. 1972;108:439–42. [PubMed: 4115279](Among 11 patients with testicular cancer treated with plicamycin and 7 with dactinomycin, all developed transient serum enzyme elevations).
- Ellas EG, Reynoso G, Mittelman A. Control of hypercalcemia with mithramycin. Ann Surg. 1972;175:431–5. [PMC free article: PMC1355190] [PubMed: 4263259](Among 12 patients with hypercalcemia treated with plicamycin [25 mcg/kg for 1 to 5 days], calcium levels fell in all, AST values rose [77-1250 U/L] in those treated for 3-5 days, but not in those given 1-2 doses only).
- Ryan WG. Mithramycin in Paget's disease of bone. Lancet. 1973;1(7815):1319. [PubMed: 4126107](Among 97 patients with Paget disease treated with plicamycin, all had increases in serum enzymes, but the abnormalities resolved promptly, and no patient had evidence of residual liver damage).
- Fraisse F, Marche C, Gibert C, Coquin Y, Vachon F. Ann Med Interne (Paris). 1980;131:281–4. [Acute hepatic necrosis and hemorrhagic syndrome leading to a fatal outcome during treatment of hypercalcemia with mithramycin (author's transl)] [PubMed: 6449897](26 year old woman treated with plicamycin for nonmalignant hypercalcemia for 4 days [total dose of 5 mg] developed marked increase in ALT [1,600 U/L], coagulopathy, thrombocytopenia, hemorrhage and shock, dying within days of multiorgan failure).
- Green L, Donehower RC. Hepatic toxicity of low doses of mithramycin in hypercalcemia. Cancer Treat Rep. 1984;68:1379–81. [PubMed: 6238672](Among 67 patients with malignant hypercalcemia treated with plicamycin, AST elevations occurred in all, starting within 2 days and resolving within 2-3 weeks; no patient was jaundiced and repeat courses caused similar reactions which were not more severe).
- Hémon Y, Martin C, Auffray JP, Bonneru JJ, Brunet C, Farisse J. Ann Fr Anesth Reanim. 1985;4:301–3. [Acute fatal hepatorenal failure during treatment with mithramycin] French. [PubMed: 3160268](64 year old woman with hypercalcemia developed acute liver failure two days after an infusion of mithramycin and one day after parathyroid surgery).
- Sznol M, Ohnuma T, Holland JF. Hepatic toxicity of drugs used for hematologic neoplasia. Semin Liver Dis. 1987;7:237–56. [PubMed: 3317861](Overview of hepatotoxicity of antineoplastic agents, mentions that mithramycin displays dose related hepatotoxicity in animals and in humans marked by aminotransferase and lactic dehydrogenase elevations).
- Davidson TG. Conventional treatment of hypercalcemia of malignancy. Am J Health Syst Pharm. 2001;58 Suppl 3:S8–15. [PubMed: 11757206](Review of therapy of malignant hypercalcemia mentions that plicamycin can be effective, but has a variable and unpredictable duration of response and is usually reserved for cases in which other therapies have failed).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, several cases were attributed to antineoplastic agents [such as mercaptopurine, cyclophosphamide, docetaxel, temozolomide, bortezomib and imatinib], but none to mithramycin).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, including 2 attributed to antineoplastic agents, 1 to melphalan and 1 to gemtuzumab, but none to mithramycin).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Among 176 reports of drug induced liver injury from Latin America published between 1996 and 2012, ten were attributed to antineoplastic agents, but none to plicamycin).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 49 cases were attributed to antineoplastic agents, but none to plicamycin).
- Sissung TM, Huang PA, Hauke RJ, McCrea EM, Peer CJ, Barbier RH, Strope JD, et al. Severe hepatotoxicity of mithramycin therapy caused by altered expression of hepatocellular bile transporters. Mol Pharmacol. 2019;96:158–67. [PMC free article: PMC6608607] [PubMed: 31175181](12 patients with various malignancies were treated with 20 cycles of intravenous plicamycin of whom 10 developed ALT elevations that were above 5 times ULN in 8; molecular analyses suggested that the plicamycin hepatotoxicity was mediated by inhibition of FXR signaling: Case 1).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Long-term follow-up of stage III testicular carcinoma treated with mithramycin (plicamycin).[Med Pediatr Oncol. 1995]Long-term follow-up of stage III testicular carcinoma treated with mithramycin (plicamycin).Kennedy BJ, Torkelson JL. Med Pediatr Oncol. 1995 May; 24(5):327-8.
- The anticancer antibiotic mithramycin-A inhibits TRPV1 expression in dorsal root ganglion neurons.[Neurosci Lett. 2014]The anticancer antibiotic mithramycin-A inhibits TRPV1 expression in dorsal root ganglion neurons.Zavala K, Lee J, Chong J, Sharma M, Eilers H, Schumacher MA. Neurosci Lett. 2014 Aug 22; 578:211-6. Epub 2014 Jan 25.
- Mithramycin inhibits human epithelial carcinoma cell proliferation and migration involving downregulation of Eps8 expression.[Chem Biol Interact. 2010]Mithramycin inhibits human epithelial carcinoma cell proliferation and migration involving downregulation of Eps8 expression.Yang TP, Chiou HL, Maa MC, Wang CJ. Chem Biol Interact. 2010 Jan 5; 183(1):181-6.
- Review Expanding the Chemical Diversity of the Antitumoral Compound Mithramycin by Combinatorial Biosynthesis and Biocatalysis: The Quest for Mithralogs with Improved Therapeutic Window.[Planta Med. 2015]Review Expanding the Chemical Diversity of the Antitumoral Compound Mithramycin by Combinatorial Biosynthesis and Biocatalysis: The Quest for Mithralogs with Improved Therapeutic Window.Méndez C, González-Sabín J, Morís F, Salas JA. Planta Med. 2015 Oct; 81(15):1326-38. Epub 2015 Sep 21.
- Review Mithramycin, an agent for developing new therapeutic drugs for neurodegenerative diseases.[J Pharmacol Sci. 2013]Review Mithramycin, an agent for developing new therapeutic drugs for neurodegenerative diseases.Osada N, Kosuge Y, Ishige K, Ito Y. J Pharmacol Sci. 2013; 122(4):251-6. Epub 2013 Jul 30.
- Plicamycin - LiverToxPlicamycin - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...