NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.
OVERVIEW
Introduction
Cyclobenzaprine is a centrally acting muscle relaxant closely related to the tricyclic antidepressants. Despite its similarity to tricyclic antidepressants, there is little evidence that cyclobenzaprine causes liver injury.
Background
Cyclobenzaprine (sye" kloe ben' za preen) is a tricyclic antidepressant derivative that relaxes skeletal muscle by an unknown mechanism of action. Cyclobenzaprine is also a central nervous system depressant, and its efficacy may be related to its sedative effects. Cyclobenzaprine is used for the treatment of painful muscle spasms from acute muscle conditions. The recommended dosage in adults is 5 to 10 mg three times daily for 3 to 4 weeks. Cyclobenzaprine is available in tablets of 5 and 10 mg in multiple generic forms and under the trade names of Flexeril, Flexamid and Amrix. Extended release capsules of 15 and 30 mg are also available. Cyclobenzaprine was approved for use in the United States in 1977 and it remains widely used with more than 10 million prescriptions filled yearly. It is usually administered for limited periods of time. Common side effects include sleepiness, dry mouth, dizziness and headache.
Hepatotoxicity
The product insert for cyclobenzaprine mentions that abnormal liver function, hepatitis, jaundice, and cholestasis occur in <1% of patients. Details about these cases are not available and no convincing case reports of cyclobenzaprine hepatotoxicity have been published.
Likelihood score: E* (Unproven but suspected cause of clinically apparent liver injury).
Mechanism of Injury
Because cyclobenzaprine is a tricyclic antidepressant derivative, it is unclear why it is not associated with hepatotoxicity similar to that attributed to the tricyclic antidepressants. Cyclobenzaprine is metabolized by the liver and has an enterohepatic circulation and half-life of several days.
Outcome and Management
The minor ALT elevations associated with chronic cyclobenzaprine use are usually asymptomatic and transient. Any elevation of greater than 10 times the upper limit of normal or persistence of abnormalities greater than 5 times the upper limit of normal should lead to discontinuation. Rechallenge is not recommended unless the agent is felt to be highly needed. There is no reason to suspect cross sensitivity to hepatic injury among the various muscle relaxant drugs.
Drug Class: Muscle Relaxants
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Cyclobenzaprine – Generic, Flexeril®
DRUG CLASS
Autonomic Agents: Muscle Relaxants, Central
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Cyclobenzaprine | 303-53-7 | C20-H21-N |
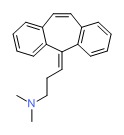 |
ANNOTATED BIBLIOGRAPHY
References updated: 30 January 2017
- Zimmerman HJ. Muscle spasmolytics. In, Hepatotoxicity: The Adverse Effects of Drugs and Other Chemicals on the Liver. 2nd Ed. Philadelphia: Lippincott, 1999. p. 544-45.(Expert review of hepatotoxicity published in 1999 discusses dantrolene, chlorzoxazone and baclofen but does not mention cyclobenzapine).
- Hibbs RE, Zambon AC. Agents acting at the neuromuscular junction and autonomic ganglia. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman’s The pharmacological basis of therapeutics, 12th ed. New York: McGraw-Hill, 2011. p. 255-76.(Textbook of pharmacology and therapeutics).
- Katz WA, Dube J. Cyclobenzaprine in the treatment of acute muscle spasm: review of a decade of clinical experience. Clin Ther 1988; 10: 216-28. [PubMed: 3078905](Thorough review of pre- and postmarketing studies of efficacy and safety of cyclobenzaprine; "Routine laboratory measurements...obtained at the start and end of each study showed no alterations indicative of organ toxicity").
- Winchell GA, King JD, Chavez-Eng CM, Constanzer ML, Korn SH. Cyclobenzaprine pharmacokinetics, including the effects of age, gender, and hepatic insufficiency. J Clin Pharmacol 2002; 42: 61-9. [PubMed: 11808825](Four studies from sponsor showing linear pharmacokinetics, slight accumulation, greater accumulation in liver disease, but no serious adverse events or liver toxicity).
- Spiller HA, Cutino L. Fatal cyclobenzaprine overdose with postmortem values. J Forensic Sci 2003; 48: 883-4. [PubMed: 12877312](Two patients with intentional cyclobenzaprine overdose died of respiratory arrest; one had chronic hepatitis C).
- Chou R, Peterson K, Helfand M. Comparative efficacy and safety of skeletal muscle relaxants for spasticity and musculoskeletal conditions: a systematic review. J Pain Symptom Manage 2004; 28: 140-75. [PubMed: 15276195](Thorough review of the pharmacology, efficacy and side effects of the muscle relaxants).
- Toth PP, Urtis J. Commonly used muscle relaxant therapies for acute low back pain: a review of carisoprodol, cyclobenzaprine hydrochloride, and metaxalone. Clin Ther 2004; 26: 1355-67. [PubMed: 15530999](A review of safety and efficacy of muscle relaxants including cyclobenzaprine states that its common side effects include somnolence, dry mouth, fatigue, and headache; no mention of liver injury or ALT elevations).
- Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug-induced liver injury in the United States. Liver Transpl 2004; 10: 1018-23. (Among. [PubMed: 15390328]~50,000 liver transplants done in the United States between 1990 and 2002, 270 [0.5%] were done for drug induced acute liver failure, but none were attributed to a specific muscle relaxant).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-1352.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 5 [0.7%] were attributed to muscle relaxants, but none specifically to cyclobenzaprine).