OVERVIEW
Introduction
Salsalate is a nonacetylated dimer of salicylic acid that is used in the treatment of chronic arthritis as an analgesic and antipyretic. Salsalate can cause moderate serum aminotransferase elevations when given in high doses in a manner similar to aspirin.
Background
Salsalate (sal' sa late) is a dimer of salicylic acid that has antiinflammatory, analgesic and antipyretic actions similar to aspirin. The antiinflammatory and analgesic effects of salsalate are probably mediated by inhibition of prostaglandin synthesis. Although available for several decades, salsalate is not commonly used. Current indications include treatment of chronic arthritis due to osteoarthritis or rheumatoid arthritis. Salsalate is also used for minor to moderate pain. Salsalate is available as tablets of 500 and 750 mg in multiple generic forms and previously under the brand name of Disalcid. The recommended regimen is 750 to 1500 mg twice daily, based upon response and tolerance. Common side effects are intestinal upset, nausea, headache, somnolence, dizziness, and tinnitus.
Hepatotoxicity
Prospective studies show that a proportion of patients taking salsalate experience at least transient serum aminotransferase elevations particularly when it is given in higher doses. These abnormalities may resolve even with drug continuation or after dose reduction. Marked aminotransferase elevations (>10 fold elevated) occur rarely except with use of higher doses (4 g daily or more) in a manner similar to aspirin. Clinically apparent liver injury with jaundice from salsalate has not been reported and must be very rare. Salsalate is probably capable of inducing Reye syndrome in a susceptible child or adolescent and, like aspirin, should be avoided in those age groups.
Likelihood score: A[HD] (well established cause of liver injury if given in high doses).
Mechanism of Injury
The mechanism of salsalate hepatotoxicity is likely a direct cytotoxic effect of high doses, similar to that of aspirin.
Outcome and Management
Salsalate hepatotoxicity has been marked by aminotransferase elevations without jaundice. Some patients have nonspecific symptoms or gastrointestinal upset. There have been no reported cases of acute hepatitis, acute liver failure or vanishing bile duct syndrome related to salsalate. Aminotransferase elevations during therapy can often be managed by dose adjustment.
Drug Class: Salicylates
Other Drugs in the Class: Aspirin, Diflunisal, Trisalicylate
CASE REPORT
Case 1. Acute enzyme elevations due to high dose salsalate therapy.(1)
A 27 year old man with HIV infection was enrolled in an experimental study of the effects of salsalate on endothelial cell function. He was without symptoms of HIV infection or liver disease, was not receiving antiretroviral therapy and had normal baseline liver tests (Table). He was started on salsalate (750 mg orally twice daily) and monitored closely. After 10 days he developed nausea and abdominal pain and salsalate was stopped. He had no previous history of liver disease, alcohol abuse or drug allergies. He had been taking weekly prophylactic sulfamethoxazole/trimethoprim for several months. Physical examination was unrevealing. Serum enzymes were markedly elevated [ALT 1101 U/L, AST 532 U/L, Alk P 77 U/L, bilirubin normal]. The while blood cell count was normal with 1% eosinophils. The INR was 1.0. He tested positive for anti-HBs and anti-HBc without HBsAg. Tests for hepatitis A and C were negative. He had low levels of serum autoantibodies (ANA 1:40, SMA 1:80), but globulin levels were normal (albumin 4.3 g/L, globulins 2.9 g/dL). His symptoms resolved within days of stopping salsalate and serum enzymes were normal three weeks later.
Key Points
Laboratory Values
Comment
A very convincing case of salsalate induced hepatotoxicity. The onset was within a few days of starting the drug. The patient was mildly symptomatic, but not jaundiced. There were no changes in alkaline phosphatase or bilirubin levels. Recovery was rapid once salsalate was stopped, and there were no other obvious causes of liver injury. The clinical phenotype was acute hepatic necrosis rather than hepatitis. The dose of salsalate was lower than that usually associated with serum aminotransferase elevations, suggesting an element of increased susceptibility to this injury.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Salsalate – Generic, Disalcid® (not available in US)
DRUG CLASS
Antiinflammatory Agents
Product labeling at DailyMed, National Library of Medicine, NIH
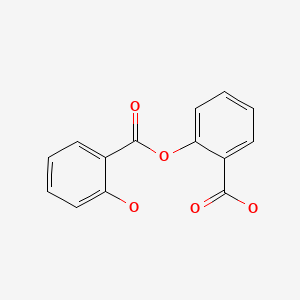
CHEMICAL FORMULA AND STRUCTURE
CITED REFERENCE
- 1.
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056]
ANNOTATED BIBLIOGRAPHY
References updated: 15 August 2020
- Zimmerman HJ. Drugs used to treat rheumatic and musculospastic disease. Chapter 19: The NSAIDS. In Zimmerman, HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott Williams & Williams, 1999, pp. 517-41.(Review of hepatotoxicity of salicylates published in 1999, discusses aspirin but not salsalate specifically).
- Lewis JH, Stine JG. Nonsteroidal anti-inflammatory drugs and leukotriene receptor antagonists. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd Edition. Amsterdam: Elsevier, 2013. pp. 370-402.(Expert review of liver injury caused by NSAIDs mentions that salsalate can cause aminotransferase elevations).
- Grossner T, Smyth EM, Fitzgerald GA. Pharmacology of inflammation, fever, pain, and gout. In, Brunton LL, Hilal-Dandan R, Knollman BC. Goodman & Gilman’s The pharmacological basis of therapeutics, 13th ed. New York: McGraw-Hill, 2018. p. 685-708.(Textbook of pharmacology and therapeutics).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, salsalate was implicated in one patient who developed marked ALT elevations without jaundice [bilirubin 0.9 mg/dL, ALT 1101 U/L, Alk P 77 U/L] 10 days after starting salsalate [1.5 g daily], resolving within 3 weeks of stopping: Case 1).
- Juluri R, Gupta S, Vuppalanchi R. Serum concentration-dependent hepatotoxicity in individuals receiving oral salsalate. Dig Dis Sci. 2009;54:1375–6. [PubMed: 18770032](Prospective study in 11 patients with HIV infection given 1500 mg salsalate twice daily for 8 weeks; 4 patients developed ALT elevations [mean=27 rising to 482 and later to 116 U/L], 2 had symptoms, all resolved rapidly with stopping).
- Goldfine AB, Fonseca V, Jablonski KA, Pyle L, Staten MA, Shoelson SE. TINSAL-T2D (Targeting Inflammation Using Salsalate in Type 2 Diabetes) Study Team. The effects of salsalate on glycemic control in patients with type 2 diabetes: a randomized trial. Ann Intern Med. 2010;152:346–57. [PMC free article: PMC3138470] [PubMed: 20231565](Controlled trial of 14 weeks of 3-4 g of salsalate daily vs placebo in 54 patients with diabetes found decreases in serum HgA1c and glucose, but no change in serum ALT, AST or GGT; dose limiting side effect was tinnitus).
- Hileman CO, Carman TL, Gripshover BM, O'Riordan M, Storer NJ, Harrill DE, White CA, et al. Salsalate is poorly tolerated and fails to improve endothelial function in virologically suppressed HIV-infected adults. AIDS. 2010;24:1958–61. [PubMed: 20613460](Open label study of 13 weeks of salsalate [4 g daily] vs no treatment in 40 patients with HIV infection on antiretroviral therapy found no effect on markers of inflammation and poor tolerance, with minor [<3 times ULN] ALT elevations in 6 [30%]).
- Hawley SA, Fullerton MD, Ross FA, Schertzer JD, Chevtzoff C, Walker KJ, Peggie MW, et al. The ancient drug salicylate directly activates AMP-activated protein kinase. Science. 2012;336:918–22. [PMC free article: PMC3399766] [PubMed: 22517326](Studies in vitro and in vivo showed that salicylate activates AMP-activate protein kinase independent of changes in AMP levels).
- Faghihimani E, Amini M, Adibi A, Naderi Z, Toghiani A, Adibi P. Evaluating the efficacy of salsalate on prediabetic and diabetic patients with fatty liver: A randomized clinical trial. J Res Pharm Pract. 2013;2:40–3. [PMC free article: PMC4076898] [PubMed: 24991603](Among 34 diabetic and 86 prediabetic adults treated with salsalate [1.5 g/day] or placebo for an unreported period of time, serum ALT and AST did not change while results of fasting blood sugar and lipids were not reported).
- Goldfine AB, Fonseca V, Jablonski KA, Chen YD, Tipton L, Staten MA, Shoelson SE. Targeting Inflammation using Salsalate in Type 2 Diabetes Study Team. Salicylate (salsalate) in patients with type 2 diabetes: a randomized trial. Ann Intern Med. 2013;159:1–12. [PMC free article: PMC4128629] [PubMed: 23817699](Among 286 patients with type 2 diabetes treated with salsalate [3.5 g/day] or placebo for 48 weeks, HgA1c levels decreased and fasting glucose levels were lower in salsalate treated subjects, while ALT levels trended to be lower as well).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 28 were due to nonsteroid antiinflammatory agents, one to salsalate but none to choline magnesium trisalicylate).
- Alderete TL, Sattler FR, Richey JM, Allayee H, Mittelman SD, Sheng X, Tucci J, Gyllenhammer LE, Grant EG, Goran MI. Salsalate treatment improves glycemia without altering adipose tissue in nondiabetic obese Hispanics. Obesity (Silver Spring). 2015;23:543–51. [PMC free article: PMC4340767] [PubMed: 25644856](Among 24 obese young Hispanic adults treated with salsalate [4 g/day] or placebo for 4 weeks, fasting glucose and free fatty acids declined without change in liver fat or body weight with salsalate therapy and “liver function tests” did not change in either group).
- Hauser TH, Salastekar N, Schaefer EJ, Desai T, Goldfine HL, Fowler KM, Weber GM, Welty F, Clouse M, Shoelson SE, Goldfine AB., Targeting Inflammation Using Salsalate in Cardiovascular Disease (TINSAL-CVD) Study Team. Effect of Targeting Inflammation With Salsalate: The TINSAL-CVD randomized clinical trial on progression of coronary plaque in overweight and obese patients using statins. JAMA Cardiol. 2016;1:413–23. [PubMed: 27438317](Among 257 patients with stable coronary artery disease treated with salsalate [3.5 g/day] or placebo for 30 months, there were no differences in changes in coronary plaque or calcium scores, but rates of atrial arrhythmias and tinnitus were higher with salsalate; no serious hepatic adverse events and no changes in median ALT or AST levels ).
- Salastekar N, Desai T, Hauser T, Schaefer EJ, Fowler K, Joseph S, Shoelson SE, et al. TINSAL-CVD Study Team. Salsalate improves glycaemia in overweight persons with diabetes risk factors of stable statin-treated cardiovascular disease: A 30-month randomized placebo-controlled trial. Diabetes Obes Metab. 2017;19:1458–62. [PMC free article: PMC5599319] [PubMed: 28295931](Among a subgroup of 192 nondiabetic patients treated with salsalate or placebo for 30 months [TINSAL-CVD; Hauser 2016], there was a sustained decrease in HgA1c and fasting glucose levels with salsalate treatment as well as slight decreases in serum aminotransferase levels and no difference in rates of hepatic adverse events between the two groups [1% in both]).
Publication Details
Publication History
Last Update: August 15, 2020.
Copyright
Publisher
National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda (MD)
NLM Citation
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Salsalate. [Updated 2020 Aug 15].