OVERVIEW
Introduction
Tafenoquine is an aminoquinoline that is used in combination with other antimalarials for the prevention of relapse of Plasmodium vivax malaria and by itself as prophylaxis against all species of malaria. Tafenoquine has been linked to low rates of transient and asymptomatic serum enzyme elevations during therapy but has not been associated with instances of clinically apparent acute liver injury.
Background
Tafenoquine (ta fen' oh kwin) is a synthetic 8-aminoquinoline that acts by binding to the protozoal or parasitic DNA and preventing DNA and RNA production and subsequent protein synthesis; it is active against several of the stages in the development of the plasmodia including liver schizonts, hypnozoites and gametocytes and has most activity against Plasmodium vivax. Tafenoquine was shown to decrease the risk of relapse in patients with Plasmodium vivax malaria who were treated with chloroquine but was less effective than current regimens when used as monotherapy for P. vivax malaria. Tafenoquine has also been shown to be effective as prophylaxis against malaria in travelers to regions with a high risk of malaria transmission. Tafenoquine was approved for use in the United States in 2018 for use in combination with other antimalarials such as chloroquine in prevention of relapse of P. vivax malaria, also referred to as “radical cure”. For this indication, tafenoquine is available as tablets of 150 mg under the brand name Krintafel and the recommended regimen is a single oral dose of 300 mg (2 tablets) given on day 1 or 2 of standard therapy of P. vivax malaria. Later in 2018, tafenoquine was approved for use as prophylaxis against malaria in travelers to high risk areas. For malarial prophylaxis, tafenoquine is available as 100 mg tablets under the brand name Arakoda, and the recommended regimen is a loading dose of 200 mg daily for three days before travel and maintenance dose of 200 mg once weekly to continue until one week after return from travel. Common side effects of tafenoquine include headache, dizziness, anorexia, nausea, pruritus and a decrease in hemoglobin. Testing for G6PD is recommended before using tafenoquine as it can induce hemolysis and methemoglobinemia in patients with G6PD deficiency. Other potentially severe but rare side effects include hypersensitivity reactions and severe psychiatric effects. Specific recommendations on the therapy and prevention of malaria including regularly updated details on diagnosis, drug dosage and safety are available at the CDC website: http://www.cdc.gov/malaria/.
Hepatotoxicity
In prelicensure clinical trials, tafenoquine was linked to a low rate of transient and mild serum aminotransferase elevations during therapy, but not to serum enzyme elevations with jaundice or with clinically apparent acute liver injury. It has had limited widescale use but appears to have a low risk for hepatotoxicity, and its safety profile has been similar to that of primaquine. Tafenoquine can cause hemolysis in patients with G6PD deficiency, which can result in mild indirect hyperbilirubinemia and jaundice, but without significant accompanying evidence of liver injury.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Mechanism of Injury
Hepatic reactions to aminoquinolines used for treatment and prevention of malaria are usually due to hypersensitivity reactions but have been not been reported with tafenoquine. Tafenoquine has minimal hepatic metabolism and has not been found to have clinically significant drug-drug interactions.
Outcome and Management
There is little information on the susceptibility to hepatic injury among the various antimalarial agents, but caution should be used in switching to other aminoquinolines after clinically apparent liver injury to another member of this class.
Drug Class: Antimalarial Agents
PRODUCT INFORMATION
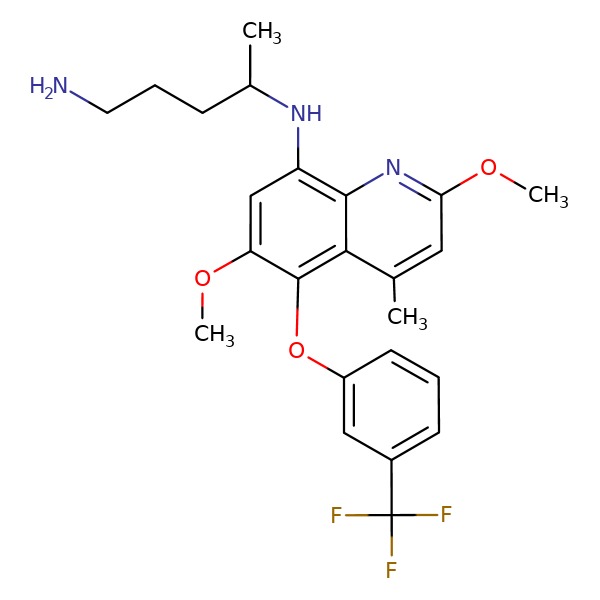
CHEMICAL FORMULA AND STRUCTURE
ANNOTATED BIBLIOGRAPHY
References updated: 10 April 2019
Abbreviations used: P. vivax, Plasmodium vivax; G6PD, glucose-6-phosphate dehydrogenase.
- Zimmerman HJ. Antiprotozoal agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 623-5.(Expert review of hepatotoxicity published in 1999 before the availability of tafenoquine).
- Vinetz JM. Chemotherapy of malaria. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 969-86.(Textbook of pharmacology and therapeutics).
- https://www
.accessdata .fda.gov/scripts/cder/daf/ (FDA Drug Approvals website that has product labels [package inserts], letters of approval and full FDA scientific review of the new drug application for safety and efficacy). - Llanos-Cuentas A, Lacerda MV, Rueangweerayut R, Krudsood S, Gupta SK, Kochar SK, Arthur P, et al. Tafenoquine plus chloroquine for the treatment and relapse prevention of Plasmodium vivax malaria (DETECTIVE): a multicentre, double-blind, randomised, phase 2b dose-selection study. Lancet 2014; 383 (9922): 1049-58. [PubMed: 24360369](Among 329 patients with P. vivax malaria treated with chloroquine combined with tafenoquine [50, 100, 300 or 600 mg] vs chloroquine with primaquine vs chloroquine alone, relapse free efficacy was greater with the higher doses of tafenoquine [89% and 92%] than with lower doses [58% and 54%] or with chloroquine alone [38%], while adverse event rates were similar including ALT elevations [2-7% in tafenoquine vs 2-8% in chloroquine groups].
- Price RN, Nosten F. Single-dose radical cure of Plasmodium vivax: a step closer. Lancet 2014; 383 (9922): 1020-1. [PMC free article: PMC4627505] [PubMed: 24360370](Editorial in response to Llanos-Cuentas [2014]).
- Dow GS, Liu J, Lin G, Hetzell B, Thieling S, McCarthy WF, Tang D, et al. Summary of anti-malarial prophylactic efficacy of tafenoquine from three placebo-controlled studies of residents of malaria-endemic countries. Malar J 2015; 14: 473. [PMC free article: PMC4661991] [PubMed: 26610844](The protective efficacy of tafenoquine vs mefloquine in preventing malaria among Australian soldiers deployed to East Timor in 2000/2001 was estimated to be 100% for both regimens).
- Fukuda MM, Krudsood S, Mohamed K, Green JA, Warrasak S, Noedl H, Euswas A, et al. A randomized, double-blind, active-control trial to evaluate the efficacy and safety of a three-day course of tafenoquine monotherapy for the treatment of Plasmodium vivax malaria. PLoS One 2017; 12: e0187376. [PMC free article: PMC5679603] [PubMed: 29121061](Among 65 patients with P. vivax malaria treated with 3 days of tafenoquine vs chloroquine with primaquine, adverse events linked to tafenoquine included methemoglobinemia in 48% vs 0% and “abnormal hepatic enzymes” in 4% vs 0%, but no patient was symptomatic).
- Novitt-Moreno A, Ransom J, Dow G, Smith B, Read LT, Toovey S. Tafenoquine for malaria prophylaxis in adults: An integrated safety analysis. Travel Med Infect Dis 2017; 17: 19-27. [PubMed: 28495354](Analysis of adverse event rates reported from 5 clinical trials of tafenoquine prophylaxis against malaria; mentions that adverse events occurring more frequently with tafenoquine [n=825] than placebo [n=295] included diarrhea, gastroenteritis, nausea, vomiting, upper respiratory symptoms and back or neck pain; no mention of ALT elevations or hepatotoxicity).
- Rueangweerayut R, Bancone G, Harrell EJ, Beelen AP, Kongpatanakul S, Möhrle JJ, Rousell V, et al. Hemolytic potential of tafenoquine in female volunteers heterozygous for glucose-6-phosphate dehydrogenase (G6PD) deficiency(G6PD Mahidol variant) versus G6PD-normal volunteers. Am J Trop Med Hyg 2017; 97: 702-11. [PMC free article: PMC5590573] [PubMed: 28749773](Dose escalating study of single doses of tafenoquine [100 to 300 mg] in women with mild G6PD deficiency and normal controls found hemoglobin declines with all doses and dose-limiting toxicity at 200 and 300 mg).
- Baird JK. Tafenoquine for travelers' malaria: evidence, rationale and recommendations. J Travel Med 2018; 25 (1): 1-13. [PMC free article: PMC6243017] [PubMed: 30380095](Extensive review of the role of tafenoquine as chemoprophylaxis against malaria).
- Frampton JE. Tafenoquine: first global approval. Drugs 2018; 78: 1517-23. [PubMed: 30229442](Review of the history of development, structure, pharmacology, clinical efficacy and safety of tafenoquine both as treatment of P. vivax malaria [combined with chloroquine] and prophylaxis in travelers against malaria [used alone]; mentions that laboratory abnormalities during treatment can include increased aminotransferase levels).
- Lacerda MVG, Llanos-Cuentas A, Krudsood S, Lon C, Saunders DL, Mohammed R, Yilma D, et al. Single-dose tafenoquine to prevent relapse of plasmodium vivax malaria. N Engl J Med 2019; 380: 215-28. [PMC free article: PMC6657226] [PubMed: 30650322](Among 522 patients with P. vivax infection treated with chloroquine [3 days] with or without tafenoquine [single dose] or primaquine [14 days], relapses were more common with placebo than tafenoquine or primaquine and adverse event rates were similar in all groups, with no differences in "laboratory outcomes").
- Llanos-Cuentas A, Lacerda MVG, Hien TT, Vélez ID, Namaik-Larp C, Chu CS, Villegas MF, et al. Tafenoquine versus primaquine to prevent relapse of plasmodium vivax malaria. N Engl J Med 2019; 380: 229-41. [PMC free article: PMC6657225] [PubMed: 30650326](Among 640 patients with P. vivax infection treated with chloroquine and either tafenoquine [single 300 mg dose] vs primaquine [15 mg once daily for 14 days], relapse free outcome was 67% vs 73% and adverse event rates were similar, ALT elevations occurring in 2% vs 3%, none of which were above 5 times ULN or associated with symptoms and jaundice).
Publication Details
Publication History
Last Update: April 10, 2019.
Copyright
Publisher
National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda (MD)
NLM Citation
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Tafenoquine. [Updated 2019 Apr 10].