OVERVIEW
Introduction
Minocycline is a tetracycline antibiotic with excellent absorption and tissue penetration that is used for several bacterial infections as well as treatment of acne. Minocycline can cause both an acute hepatitis-like syndrome occurring within 1 to 3 months of starting therapy or a more insidious chronic hepatitis with autoimmune features typically after long term treatment.
Background
Minocycline (min" oh sye' kleen) is a semisynthetic derivative of tetracycline that has excellent oral absorption and wide tissue penetration. Like other tetracyclines, minocycline is believed to act by binding to bacterial ribosomes and inhibiting protein synthesis. Minocycline has a broad spectrum of activity against both gram positive and gram negative organisms. Minocycline was approved for use in the United States in 1971 and it continues in wide use with several million prescriptions being filled yearly. Current indications are for therapy of susceptible infections, including gonorrhea, syphilis, non-gonococcal urethritis, Chlamydial infections, cholera, leprosy, and the meningococcal carrier state. Perhaps the major use of minocycline is chronic use for treatment of acne and suppression of staphylococcal bacterial flora that contribute to it. Minocycline is available in multiple generic forms as capsules or tablets of 50, 75 or 100 mg. For acute infections, minocycline is recommended in doses of 100 mg every 12 hours for 5 to 15 days, often after an initial loading dose of 200 mg. For therapy of acne, doses of 50 mg once to three times daily are recommended. Minocycline is also available in extended release formulations for daily dosing and as a solution or powder for intravenous use. Commercial names of minocycline include Minocin, Dynacin, Myrac, and Apo-, Novo- and PMS-Minocycline. Common side effects include nausea, diarrhea, gastrointestinal upset, headache, dizziness, visual blurring, skin rash and hypersensitivity reactions.
Hepatotoxicity
Minocycline therapy is associated with two forms of clinically apparent liver injury, an acute hepatitis-like syndrome that arises within 1 to 3 months of starting therapy and a chronic hepatitis-like syndrome typically with autoimmune features that occurs with long term therapy, sometimes after several years of use. There is some overlap between these two presentations of minocycline hepatotoxicity, both are associated with a hepatocellular pattern of serum enzyme elevations and both can be associated with autoantibodies and immunological features.
Minocycline has been linked to cases of an acute hepatitis with jaundice that typically arises within a few weeks or months of starting therapy. The enzyme elevations are typically hepatocellular and resemble acute viral hepatitis. Immunoallergic features are common and may be prominent with fever, rash and eosinophilia and some cases with facial edema, lymphoadenopathy and lymphocytosis that may resemble acute mononucleosis. The liver injury is usually self limited with complete resolution within 1 to 2 months of stopping. Some patients have autoimmune markers and these also improve upon stopping minocycline.
Minocycline has also been linked to cases of chronic hepatitis with or without jaundice that typically arise during long term therapy, sometimes after years of use. The most common presentation is with an autoimmune hepatitis-like syndrome that can be severe and even fatal, particularly if minocycline is not stopped promptly. Patients can present acutely with jaundice and fatigue or chronically with insidious onset of fatigue, joint aches and jaundice, usually after 6 months to many years of therapy. A hepatocellular pattern of enzyme elevations is typical with ALT levels ranging from 3- to 20-fold elevated depending upon the severity and duration of the injury. Autoantibodies are usually present, typically antinuclear antibody (ANA) at titers of >1:160. In some cases, ANA may initially be negative, arising later as the disease progresses or starts to improve. Immunoglobulins are also usually elevated and liver biopsy demonstrates changes typical of autoimmune hepatitis with active interface hepatitis, spotty eosinophilic necrosis and portal infiltrates rich in lymphocytes and plasma cells. Fibrosis is uncommon, but can occur, particularly if the disease is prolonged and minocycline continued in the face of hepatic injury. The condition will resolve spontaneously if minocycline is withdrawn, but corticosteroids are often used. In long term follow up after stopping minocycline, chronic injury is rare, if it occurs at all and generally all symptoms and laboratory test abnormalities resolve within 6 to 12 months of stopping, although patients may continue to have low titers of ANA.
Other immunologically mediated syndromes associated with minocycline use include a serum sickness like syndrome (generally within 3 to 12 weeks of starting), a lupus-like syndrome and hemolytic anemia (the latter two with chronic therapy). Liver injury can accompany these other autoimmune conditions, but is generally anicteric, mild and rapidly reversible. The pattern of serum enzyme elevations is typically hepatocellular and autoantibodies are common.
Likelihood score: A (well known cause of clinically apparent liver injury).
Mechanism of Injury
The cause of the liver injury associated with minocycline use is probably immunological, mediated by autoimmune reactions against liver cells or minocycline adducts present in the liver. Patients with minocycline induced liver injury have been reported to have an increased frequency of the rare HLA alelle B*35:02, but most cases lack this allele and clinical features are not different in those with or without the HLA association.
Outcome and Management
The acute liver injury attributed to minocycline is usually self-limited in course, although fatal examples have been reported. In addition, the autoimmune hepatitis like syndrome caused by minocycline can be severe, and fatal outcomes have been described. Most cases, however, resolve slowly with withdrawal of the agent. Corticosteroids are often used to treat minocycline induced liver injury, largely because it resembles spontaneous autoimmune hepatitis and responds rapidly to immunosuppressive therapy. The effectiveness of corticosteroids in speeding or insuring recovery from minocycline induced autoimmune hepatitis has not been proven, but anecdotal cases suggest a fairly dramatic effect. If corticosteroids are used, the dose should be rapidly reduced and the medication should be discontinued within 3 to 6 months. Furthermore, patients should be followed carefully after withdrawal of corticosteriods. Recurrence of hepatitis after withdrawal should suggest that the autoimmune hepatitis was unrelated to the minocycline or that the minocycline brought out the autoimmune diathesis that is self-sustaining. Autoimmune hepatitis not caused by medications usually requires long term if not life long immunosuppressive therapy. There is no information about possible cross sensitivity to hepatic injury among the various tetracyclines. Interestingly, doxycycline which resembles minocycline structurally, has been associated with a short latency acute cholestatic or mixed hepatitis with immunoallergic features, but has not been associated definitively with the longer latency autoimmune hepatitis-like syndrome.
Drug Class: Antiinfective Agents, Tetracyclines
CASE REPORTS
Case 1. Chronic hepatitis with autoimmune features caused by minocycline.
[Modified from a case in the database of the Drug-Induced Liver Injury Network]
A 20 year old woman had been taking minocycline for acne for one and a half years when she developed joint pains in the hands, wrists, hips and ankles. She stopped minocycline and began to feel better, but was found to have markedly elevated serum enzymes on routine evaluation of the joint symptoms a few weeks later. She denied significant past medical history and had no risk factors for viral hepatitis. She took no other medications except oral contraceptives and did not drink alcohol regularly. Initially, serum ALT and AST were 15- to 20-fold elevated, but alkaline phosphatase and serum bilirubin were normal. Tests for hepatitis A, B, and C and for infectious mononucleosis were negative. Autoantibody testing showed a positive antinuclear antibody (1:160), but negative tests for smooth muscle and liver-kidney microsomal antibodies. Serum globulins were elevated as was IgG (1960 mg/dL, normal <1520). Ceruloplasmin was low normal. An ultrasound of the abdomen showed normal gallbladder and no enlargement of bile ducts. A liver biopsy showed changes suggestive of autoimmune hepatitis with marked interface hepatitis, portal inflammation with lymphocytes and plasma cells, but no fibrosis. She was started on prednisone and laboratory test abnormalities improved rapidly.
Key Points
Laboratory Values
Comment
The major symptoms were arthralgias, suggesting that the reaction to minocycline therapy was a lupus-like syndrome. These symptoms, however, abated and the patient was found to have a fairly significant anicteric hepatitis which was slow to resolve. Ultimately, a liver biopsy was done that suggested autoimmune hepatitis. Thereupon, prednisone was started with prompt improvement in serum aminotransferase levels. The dose of prednisone was gradually decreased and stopped within 6 months. She had no further symptoms, but serum ALT levels were mildly abnormal.
Case 2. Severe acute hepatitis with autoimmune features caused by minocycline.
[Modified from a case in the database of the Drug-Induced Liver Injury Network]
A 21 year old man was started on minocycline for acne and two months later developed fatigue, dark urine and weight loss and stopped therapy. A week later, he was admitted to the hospital because of jaundice. He denied a previous history of liver disease or risk factors for viral hepatitis. He drank alcohol rarely. Serum bilirubin was elevated as were serum aminotransferase levels. Tests for hepatitis A, B, and C and for infectious mononucleosis were negative. Autoantibody testing showed a positive antinuclear antibody (1:1280), but negative tests for smooth muscle and liver-kidney microsomal antibodies. A liver biopsy was done which showed changes suggestive of autoimmune hepatitis with marked activity. He was started on prednisone and rapidly improved. Therapy was gradually reduced and then discontinued several months later, without relapse of symptoms or recurrence of laboratory abnormalities.
Key Points
Laboratory Values
Comment
Minocycline can cause either an acute or a chronic hepatitis, but both are characterized by a hepatocellular pattern of serum enzyme elevations, the presence of autoantibodies and a liver biopsy showing changes typical of autoimmune hepatitis. Spontaneous recovery with stopping minocycline is the rule, but recovery can be prolonged, and prednisone therapy may speed the process. Whether prednisone actually improves ultimate outcome has not been proven. Nevertheless, both drug induced and spontaneous autoimmune hepatitis can be severe and even fatal, and prednisone therapy may provide rapid relief. Most important, however, is to limit the dose and duration of therapy, carefully monitoring patients after stopping for evidence of recurrence.
PRODUCT INFORMATION
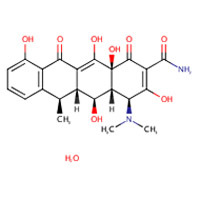
CHEMICAL FORMULAS AND STRUCTURES
ANNOTATED BIBLIOGRAPHY
References updated: 23 January 2019
- Zimmerman HJ. Tetracyclines. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999. p. 599-602.(Expert review of tetracycline and liver injury published in 1999; the tetracyclines cause two forms of drug induced liver injury, microvesicular fat and liver failure occurring after 4-10 days with high does of parenteral tetracyclines and an idiosyncratic liver injury that occurs with the oral agents, doxycycline causing a cholestatic and minocycline a hepatocellular injury which may be associated with autoimmune features).
- Moseley RH. Tetracyclines. Hepatotoxicity of antimicrobials and antifungal agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, p. 468.(Expert review of tetracycline induced liver injury mentions that the hepatotoxicity of intravenous tetracycline is of historic interest only as it is no longer given parenterally; both doxycycline and minocycline have been associated with idiosyncratic liver injury).
- MacDougall C, Chambers HF. Tetracyclines and glycylcyclines. Protein synthesis inhibitors and miscellaneous antibacterial agents. In, Brunton LL, Chabner KA, Knollman KC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1521-6.(Textbook of pharmacology and therapeutics).
- Schultz JC, Adamson JS Jr, Workman WW, Norman TD. Fatal liver disease after intravenous administration of tetracycline in high dosage. N Engl J Med 1963; 269: 999-1004. [PubMed: 14059734](Initial dramatic report of acute fatty liver due to iv tetracycline; a rapidly fatal multisystem disease appeared in 6 pregnant women in their last trimester or early postpartum period after 3 to 5 days of relatively high doses of iv tetracycline; all developed jaundice [bilirubin 4.9-12.5 mg/dL] with mild AST [72-170 U/L] and Alk P [9-17 King Armstrong U/L] elevations, prolongation of protime, acidosis and renal dysfunction. Autopsy showed foamy hepatocytes, fat by oil red O stain and minimal hepatocyte necrosis).
- Dowling HF, Lepper MH. Hepatic reactions to tetracycline. JAMA 1964; 188: 307-9. [PubMed: 14114004](Review of literature on acute fatty liver due to tetracycline and recommendations on its use: avoiding doses >2 g/day and cautious use in women in last trimester of pregnancy).
- Horwitz ST, Marymont JH Jr. Fatal liver disease during pregnancy associated with tetracycline therapy. Report of a case. Obstet Gynecol 1964; 23: 826-9. [PubMed: 14168241](After complicated Caesarian and emergency hysterectomy with shock and bleeding, 41 year old woman received tetracycline given iv for 4 days, then orally to day 8; on day 10 she developed fever, acidosis and ileus, dying on day 16 with multiorgan failure and jaundice; autopsy showed fatty liver).
- Norman TD, Schultz JC, Hoke RD. Fatal liver disease following the administration of tetracycline. South Med J 1964; 57: 1038-42. [PubMed: 14179316](Further analysis of 6 cases of acute fatty liver after tetracycline in pregnant women with histological changes).
- Whalley PJ, Adams RH, Combes B. Tetracycline toxicity in pregnancy. Liver and pancreatic dysfunction. JAMA 1964; 189: 357-62. [PubMed: 14160508](Five cases of acute fatty liver with azotemia and pancreatitis after 4-17 days of iv or oral therapy 1-2 g/day: bilirubin 1.2-18.8 mg/dL; AST 34-780 U/L; Alk P 8.6-22 BU/L; 1 case fatal. The anicteric case had pancreatitis and was attributed to oral drug, but had fat on liver biopsy).
- Brewer T. Tetracycline hepatotoxicity. Br Med J 1965; 1: 995. [PMC free article: PMC2165688] [PubMed: 14260641](Letter questioning role of tetracycline in acute fatty liver).
- Finn WF, Horwitz ST. Maternal death due to fatty metamorphosis of liver following tetracycline therapy. N Y State J Med 1965; 65: 662-7. [PubMed: 14251580](After Caesarian section, followed by hysterectomy and pneumonia, 41 year old woman received iv tetracycline for 4 days, followed by oral and then iv drug again, developing shock and jaundice; autopsy showed fatty liver without necrosis).
- Ichida F, Watanabe K, Ishiwara S, Inoue K, Tanabe Y. [A case of cholestatic jaundice due to tetracycline-triacetyloleandomycin] Nippon Naika Gakkai Zasshi 1965; 54:142-7. Japanese. [PubMed: 5294320]
- Kunelis CT, Peters JL, Edmondson HA. Fatty liver of pregnancy and its relationship to tetracycline therapy. Am J Med 1965; 38: 359-77. [PubMed: 14266828](Classical clinical and histologic description of syndrome in 12 pregnant women, ages 19-31, given tetracycline for 3 to 12 days [total dose 1.5 to 14 g] after 16-39 weeks of pregnancy [bilirubin 12-19.8 mg/dL, ALT 24-210 U/L, AST 36-760 U/L, lactic acid high in 3/3 patients], 67% fatal, often accompanied by multiorgan failure, pancreatitis and shock).
- Tapp E, Carroll R. Tetracycline accumulation in toxic liver damage. J Pathol Bacteriol 1965; 89: 715-21. [PubMed: 14320315](Animal studies showing accumulation of tetracycline in damaged hepatocytes, particularly with high levels of calcium).
- Winterling AN, Goldman RL. Hepatic and renal lesions in a case of tetracycline toxicity during long-term estrogen therapy after orchiectomy. Calif Med 1965; 102: 314-6. [PMC free article: PMC1515729] [PubMed: 14291456](66 year old man post-orchiectomy for prostate cancer developed sudden onset of fever, lactic acidosis and mild jaundice [bilirubin 2.9 mg/dL] after 8 days of iv tetracycline [17 g], subsequently died after emergency laparotomy; autopsy showed fatty liver).
- Wruble LD, Ladman AJ, Britt LG, Cummins AJ. Hepatotoxicity produced by tetracycline overdosage. JAMA 1965; 192: 6-8. [PubMed: 14262279](56 year old woman with cecal volulus developed jaundice [bilirubin 7.8 mg/dL, AST 98 U/L, Alk P normal] 2 days after receiving 8 g of tetracycline, subsequently progressing to liver failure and death; autopsy showed fatty liver).
- Wruble LD, Cummins AJ. Tetracycline and fatty liver. Am J Dig Dis 1965; 10: 742-4. [PubMed: 14316764](Editorial on tetracycline induced acute fatty liver with discussion of mechanisms focusing on mitochondrial injury).
- Tetracyclines and the liver in pregnancy. Lancet 1966; 1: 357-8. [PubMed: 4159865](Editorial on the history of acute fatty liver of pregnancy, first described by Sheehan in 1940 and later linked to high dose iv tetracycline in pregnancy, but also in nonpregnant women and in men).
- Davis JS, Kaufman RH. Tetracycline toxicity. A clinicopathologic study with special reference to liver damage and its relationship to pregnancy. Am J Obstet Gynecol 1966; 95: 523-9. [PubMed: 5939019](6 cases of acute fatty liver, 1 man and 5 women [4 pregnant] given intravenous tetracycline for 9-10 days [3-6 g] [bilirubin 3-12.5 mg/dL, ALT 34-310 U/L], all acidotic and all died, autopsy showing fatty liver).
- Schiffer MA. Fatty liver associated with administration of tetracycline in pregnant and nonpregnant women. Am J Obstet Gynecol 1966; 96: 326-32. [PubMed: 5919490](Six cases of acute fatty liver from tetracycline, 2 in pregnancy at 34- and 40 weeks; 4 in nonpregnant women, but clinical course not described).
- Aach R, Kissane J eds. Clinicopathologic conference. A seventeen-year-old girl with fatty liver of pregnancy following tetracycline therapy. Am J Med 1967; 43: 274-83. [PubMed: 6034958](Clinicopathologic conference describing 17 year old pregnant woman who developed suspected pyelonephritis, was treated with im and oral tetracycline and 8 days later developed multiorgan failure, lactic acidosis and died despite induced delivery of a stillborn child).
- Peters RL, Edmondson HA, Mikkelsen WP, Tatter D. Tetracycline-induced fatty liver in nonpregnant patients. A report of six cases. Am J Surg 1967; 113: 622-32. [PubMed: 6021433](Classical description of clinical and histologic features of tetracycline induced acute fatty liver in nonpregnant patients; 6 nonpregnant women, ages 18-62, given iv tetracycline for 3-13 days [9-26 g] presenting with jaundice and lethargy; peak AST 52-960 U/L; bilirubin 2.7-7.4 mg/dL, often with complex and critical course, pancreatitis and renal failure, acidosis; fatty liver on autopsy).
- Damjanov I, Arnold R, Faour M. Tetracycline toxicity in a nonpregnant woman. JAMA 1968; 204: 934. [PubMed: 5694615](20 year old woman given iv tetracycline for 8 days after second of two gall bladder operations developed sudden onset of renal and hepatic failure [bilirubin 4.2 mg/dL, ALT 620 U/L], autopsy showed fatty liver and acute tubular necrosis).
- Robinson MJ, Rywlin AM. Tetracycline-associated fatty liver in the male. Report of an autopsied case. Am J Dig Dis 1970; 15: 857-62. [PubMed: 5459744](72 year old man given 10 days of iv tetracycline [30 g total] developed worsening liver injury followed by hepatic and renal failure and severe acidosis [bilirubin 6.8 mg/dL, AST 1550 KU/L, Alk P 15 KA U/L]; autopsy showed fatty liver, fatty vacuolization of renal tubular cells and pancreatitis).
- Breen KJ, Perkins KW, Mistilis SP, Shearman R. Idiopathic acute fatty liver of pregnancy. Gut 1970; 11: 822-5. [PMC free article: PMC1553146] [PubMed: 5485832](23 year old woman who survived acute fatty liver of pregnancy; onset day after spontaneous labor and stillborn delivery [bilirubin 7.9 mg/dL, Alk P 70 King Armstrong U/L, AST 67 U/L, prothrombin index 50%], liver biopsy showed fatty liver, improved with dextrose administration).
- Combes B, Whalley PJ, Adams RH. Tetracycline and the liver. Prog Liver Dis 1972; 4: 589-96. [PubMed: 4569011](Review of hepatotoxicity of tetracycline, including studies of pathogenesis).
- Wenk RE, Gebhardt FC, Bhagavan BS, Lustgarten JA, McCarthy EF. Tetracycline-associated fatty liver of pregnancy, including possible pregnancy risk after chronic dermatologic use of tetracycline. J Reprod Med 1981; 26: 135-41. [PubMed: 7230149](Two cases of acute fatty liver over a 15 year period and 60,000 deliveries; one woman received tetracycline for 3 days, the second had no history of its use, but had tetracycline detected in bony tissue suggestive of chronic use).
- Böcker R, Estler CJ, Müller S, Pfandzelter C, Spachmüller B. Comparative evaluation of the effects of tetracycline, rolitetracycline and doxycycline on some blood parameters related to liver function. Arzneimittelforschung 1982; 32: 237-41. [PubMed: 7200783](Minocycline caused a dose dependent rise in AST and increase in triglycerides, but no hepatic histological changes in mice; similar findings were previously reported with tetracycline).
- Burette A, Finet C, Prigogine T, De Roy G, Deltenre M. Acute hepatic injury associated with minocycline. Arch Intern Med 1984; 144: 1491-2. [PubMed: 6732411](57 year old woman developed jaundice after 4 days of iv minocycline for aspiration pneumonia: [bilirubin ~3.5 mg/dL, ALT 1050 U/L, Alk P 680 U/L, and high amylase], biopsy showed fatty liver with minimal inflammation).
- Schrumpf E, Nordgard K. Unusual cholestatic hepatotoxicity of doxycycline in a young male? Scand J Gastroenterol 1986; 21 (Suppl 120): 68. Not in PubMed.(Abstract: Patient developed severe and prolonged cholestatic hepatitis after 2 weeks of oral doxycycline [bilirubin 9.8 rising to 69.5 mg/L, ALT 53 to 132 U/L, Alk P 283 to 775 U/L] and severe itching; ultimate recovery after 6 months).
- Davies MG, Kersey PJ. Acute hepatitis and exfoliative dermatitis associated with minocycline. BMJ 1989; 298: 1523-4. [PMC free article: PMC1836697] [PubMed: 2527068](16 year old boy and 17 year old girl dveveloped severe hepatitis after 4 weeks of minocycline, both with severe skin rash [toxic epidermal necrolysis], fever, jaundice, lymphadenopathy and leukemoid reactions; one fatal, but history of travel to Africa and exposure to antimalarials).
- Adams LE, Hess EV. Drug-related lupus. Incidence, mechanisms and clinical implications. Drug Saf 1991; 6: 431-49. [PubMed: 1793523](Review of drug related lupus-like syndrome, linked to more than 60 agents including isoniazid, hydralazine, chlorpromazine, methyldopa and procainamide. Usually presents with arthralgias and fever and ANA positivity, usually occurring with long term use of the medication).
- Böcker R, Estler CJ, Ludewig-Sandig D. Evaluation of the hepatotoxic potential of minocycline. Antimicrob Agents Chemother 1991; 35: 1434-6. [PMC free article: PMC245185] [PubMed: 1929305](High dose studies in rats showed rises in AST and hepatic triglycerides, but no changes in liver histology).
- Lienart F, Morissens M, Jacobs P, Ducobu J. Doxycycline and hepatotoxicity. Acta Clin Belg 1992; 47: 205-8. [PubMed: 1332350](42 year old woman with severe cardiomyopathy developed encephalopathy and enzyme elevations with jaundice after 5 days of oral doxycycline [bilirubin 1.2 mg/dL, ALT 139 U/L, Alk P 373 U/L, ammonia 99 mcg/dL], resolving rapidly on stopping; likely due to heart failure and ischemia rather than drug induced liver injury).
- Min DI, Burke PA, Lewis WD, Jenkins RL. Acute hepatic failure associated with oral minocycline: a case report. Pharmacotherapy 1992; 12: 68-71. [PubMed: 1532250](39 year old woman developed fatigue and nausea after 4 weeks of minocycline and vitamin A [50,000 U bid] followed by high fever, lymphadenopathy and jaundice progressing to acute liver failure [bilirubin rising from 0.9 to 23.5 mg/dL, ALT 120 to 1625 U/L, Alk P 892 U/L], ultimately resolving spontaneously after stopping).
- Boudreaux JP, Hayes DH, Mizrahi S, Hussey J, Regenstein F, Balart L. Fulminant hepatic failure, hepatorenal syndrome, and necrotizing pancreatitis after minocycline hepatotoxicity. Transplant Proc 1993; 25: 1873. [PubMed: 8470208](17 year old girl developed acute liver failure while taking minocycline, but no information given on dose, latency or laboratory abnormalities).
- Carson JL, Strom BL, Duff A, et al. Acute liver disease associated with erythromycins, sulfonamides, and tetracyclines. Ann Intern Med 1993; 119 (7 Pt 1): 576-83. [PubMed: 8363168](Case control study using Medicaid billing results between 1980-87 found 107 cases of hospitalization for unexplained hepatitis, odds ratios for erythromycin 5.2; sulfonamides 11.4; tetracyclines 5.2; total of 5 cases exposed to tetracycline, doxycycline or minocycline).
- Hunt CM, Washington K. Tetracycline-induced bile duct paucity and prolonged cholestasis. Gastroenterology 1994; 107: 1844-7. [PubMed: 7958700](Two cases of severe and prolonged cholestatic hepatitis and bile duct paucity after oral tetracyclines; 37 year old woman developed jaundice 2 days after 3 day course of doxycycline with prolonged cholestasis [peak bilirubin 30 mg/dL], but ultimate recovery; 63 year old woman developed jaundice 6 weeks after a 2 week course of tetracycline [bilirubin 11.8 mg/dL, ALT 245 U/L], with prolonged jaundice [peak bilirubin 29.5 mg/dL) and persistence of enzyme elevations for >3 years [Alk P 631 U/L, ALT 97 U/L]).
- Kaufmann D, Pichler W, Beer JH. Severe episode of high fever with rash, lymphadenopathy, neutropenia, and eosinophilia after minocycline therapy for acne. Arch Intern Med 1994; 154: 1983-4. [PubMed: 8074603](35 year old woman developed fever, rash and eosinophilia 3 weeks after starting minocycline for acne with normal ALT, AST and bilirubin and resolution in ~10 days of stopping, indicating a serum sickness-like syndrome without hepatitis).
- Friis H, Andreasen PB. Drug-induced hepatic injury: an analysis of 1100 cases reported to the Danish Committee on Adverse Drug Reactions between 1978 and 1987. J Intern Med 1992; 232: 133-8. [PubMed: 1506809](Adverse drug reaction reports between 1978 and 1987 in Denmark; no tetracycline is mentioned as a cause).
- Gordon PM, White MI, Herriot R, Martin JC, Reid DM. Minocycline-associated lupus erythematosus. Brit J Dermatol 1995; 132: 120-1. [PubMed: 7756122](15 year old girl developed arthraglias and lupus-like syndrome after 2 years minocycline therapy of acne; liver tests were normal, ANA 1:640, resolved with stopping).
- Castex F, Canva-Delcambre V, Maunoury V, Talbodec N, Wolchies E, Paris JC. [Acute hepatitis induced by minocycline] Gastroenterol Clin Biol 1995; 19: 640-1. French. [PubMed: 7590035](30 year old woman developed jaundice 8 days after starting minocycline [bilirubin 2.0 mg/dL, ALT 23 times ULN, Alk P normal, ANA negative], with resolution of liver test abnormalities within 1 month of stopping).
- Gough A, Chapman S, Wagstaff K, Emery P, Elias E. Minocycline induced autoimmune hepatitis and systemic lupus erythematosus-like syndrome. BMJ 1996; 312: 169-72. [PMC free article: PMC2349841] [PubMed: 8563540](Brief report of 4 cases of jaundice developing during long term minocycline therapy and review of 16 cases reported to British Committee on Safety of Medicines; no specific laboratory results provided).
- Pillans PI. Drug associated hepatic reactions in New Zealand: 21 years’ experience. N Z Med J 1996; 109: 315-9. [PubMed: 8816722](Adverse drug reaction reports identified 943 liver injuries over 21 years in New Zealand; triacetyloleandomycin accounted for 21 cases [2.1%] and minocycline for at least 4).
- Goulden V, Glass D, Cunliffe WJ. Safety of long-term high-dose minocycline in the treatment of acne. Brit J Dermatol 1996; 134: 693-5. [PubMed: 8733373](Prospective study of safety of 100-200 mg minocycline given daily for average of 10 months, 200 of 700 patients who had liver tests done, there were“no significant abnormalities”).
- Knowles SR, Shapiro L, Shear NH. Serious adverse reactions induced by minocycline. Report of 13 patients and review of the literature. Arch Dermatol 1996; 132: 934-9. [PubMed: 8712844](15 cases with adverse reactions to minocycline; one with Stevens-Johnson syndrome and acute liver failure arising within 29 days of starting minocycline, necessitating liver transplantation).
- Malcolm A, Heap TR, Eckstein RP, Lunzer MR. Minocycline-induced liver injury. Am J Gastroenterol 1996; 91: 1641-3. [PubMed: 8759678](3 men and 3 women, ages 15-48, treated with minocycline for 4 weeks to 2 years developed liver injury [peak ALT 257 to 3824 U/L, 3 ANA positive, 3 with jaundice, most had mild eosinophilia], liver biopsy showed chronic hepatitis in 2, all recovered completely, two with corticosteroid therapy).
- Tham SN, Kwok YK, Chan HL. Cross-reactivity in fixed drug eruptions to tetracyclines. Arch Dermatol 1996; 132: 1134-5. [PubMed: 8795565](Among 9 Chinese patients with a fixed drug eruption due to tetracycline, all had recurrence on doxycycline and 3 on minocycline; no mention of liver involvement).
- MacNeil M, Haase DA, Tremaine R, Marrie TJ. Fever, lymphadenopathy, eosinophilia, lymphocytosis, hepatitis, and dermatitis: a severe adverse reaction to minocycline. J Am Acad Dermatol 1997; 36 (2 Pt 2): 347-50. [PubMed: 9039216](17 year old girl developed fever, lymphadenopathy, severe rash and mild hepatitis 3 weeks after starting minocycline for acne [bilirubin 2.3 mg/dL, ALT 134 U/L, Alk P 309 U/L, ANA negative] required corticosteroid therapy, but ultimately resolved).
- Herzog D, Hajoui O, Russo P, Alvarez F. Study of immune reactivity of minocycline-induced chronic active hepatitis. Dig Dis Sci 1997; 42: 1100-3. [PubMed: 9149070](16 year old girl developed arthralgias and anicteric hepatitis after 18 months of therapy with minocycline for acne [bilirubin evidently normal, ALT 392 U/L, Alk P normal, ANA 1:1280], resolved upon stopping; found serum antibodies to 90 kD and 50 kD fractions of HepG2 cells, possibly P-450 proteins).
- Björnsson E, Lindberg J, Olsson R. Liver reactions to oral low-dose tetracyclines. Scand J Gastroenterol 1997; 32: 390-5. Review. [PubMed: 9140164](32 year old man developed abdominal pain, dark urine and rash within 24 hours of starting doxycycline which he had received in the past [bilirubin 4.3- 8.1 mg/dL, ALT 3.5 times ULN, Alk P 1.1 times ULN], resolving within 3 months of stopping; thorough review of all published and SADRAC reported cases of oral tetracycline associated liver injury found 15 cases, only 6 rated as likely, none with tetracycline, 5 doxycycline, 1 lymecycline).
- Bruguera M, Padrós J. [Acute hepatitis associated with treatment with minocycline] Med Clin (Barc). 1997; 108: 596. [PubMed: 9280793](18 year old woman found to have enzyme elevations without symptoms or jaundice 1 month after starting minocycline [bilirubin normal, ALT 283, Alk P normal, ANA negative], resolving within 2-3 months of stopping).
- Crosson J, Stillman MT. Minocycline-related lupus erythematosus with associated liver disease. J Am Acad Dermatol 1997; 36 (5 Pt 2): 867-8. [PubMed: 9146570](22 year old woman developed arthralgias 2 years after starting minocycline therapy for acne [bilirubin 0.9 mgdL, ALT 292 U/L, Alk P 64 U/L, ANA 1:80], symptoms resolving rapidly upon stopping, but recurring abruptly after a single tablet, and serum ALT remained elevated for another 2 months before resolving).
- Golstein PE, Deviere J, Cremer M. Acute hepatitis and drug-related lupus induced by minocycline treatment. Am J Gastroenterol 1997; 92: 143-6. [PubMed: 8995955](19 year old man developed fatigue, weight loss, arthralgias and liver test abnormalities after 20 months of therapy with minocycline for acne [bilirubin normal, ALT 374 U/L, Alk P normal, ANA 1:640, IgG 2280 mg/dL], resolving upon stopping, but ANA persisted in high titer [1:1280 9 months later]).
- Hoefnagel JJ, van Leeuwen RL, Mattie H, Bastiaens MT. [Side effects of minocycline in the treatment of acne vulgaris] Ned Tijdschr Geneeskd 1997; 141: 1424-7. Dutch. [PubMed: 9542866](Editorial on association of minocycline with lupus, autoimmune hepatitis, vasculitis and serum sickness-like syndromes).
- Shapiro LE, Knowles SR, Shear NH. Comparative safety of tetracycline, minocycline, and doxycycline. Arch Dermatol 1997; 133: 1224-30. [PubMed: 9382560](Review of toxicity of tetracyclines from literature and a Canadian database; minocycline had the highest rates of adverse events, but all were relatively safe: no lupus-like syndrome associated with doxycycline or tetracycline).
- Angulo JM, Sigal LH, Espinoza LR. Coexistent minocycline-induced systemic lupus erythematosus and autoimmune hepatitis. Semin Arthritis Rheum 1998; 28: 187-92. [PubMed: 9872479](22 year old woman with arthralgias and jaundice after 1 year of minocycline therapy for acne [bilirubin 3.2 mg/dL, ALT 916 U/L, Alk P 204 U/L, ANA 1:640], resolving upon stopping, but arthralgias required prednisone for 18 months).
- Bhat G, Jordan J Jr, Sokalski S, Bajaj V, Marshall R, Berkelhammer C. Minocycline-induced hepatitis with autoimmune features and neutropenia. J Clin Gastroenterol 1998; 27: 74-5. [PubMed: 9706776](18 year old man developed hepatitis after 2 years of intermittent therapy with minocycline [bilirubin 4.8 mg/dL, ALT 1270 U/L, Alk P 117 U/L, ANA 1:1280], rapid response to prednisone and no relapse when stopped).
- Matteson EL, Johnson BW, Maher JD. Arthralgias, myalgias, and autoimmune hepatitis with minocycline therapy. J Rheumatol 1998; 25: 1653-4. [PubMed: 9712119](20 year old man developed fever and arthralgias after taking minocycline for 5 years for acne [no mention of bilirubin or jaundice, ALT 307 U/L, ANA 1:5280], full recovery 4 weeks after stopping).
- Pavese P, Sarrot-Reynauld F, Bonadona A, Massot C. [Immunoallergic reaction with hepatitis induced by minocycline] Ann Med Interne (Paris) 1998; 149: 521-3. French. [PubMed: 10021906](19 year old woman developed lupus-like syndrome and hepatitis after 2 years of minocycline therapy, resolving within 2 months of stopping).
- Teitelbaum JE, Perez-Atayde AR, Cohen M, Bousvaros A, Jonas MM. Minocycline-related autoimmune hepatitis: case series and literature review. Arch Pediatr Adolesc Med 1998; 152: 1132-6. [PubMed: 9811293](3 case reports of chronic autoimmune-like hepatitis in 15-16 year olds, arising 1-1.5 years after starting minocycline for acne [bilirubin normal to 26 mg/dL, ALT 363, 988 and 904 U/L, Alk P normal, all with ANA and high IgG], resolving in 2 to 9 months, 2 treated with prednisone; literature review).
- Angulo JM, Sigal LH, Espinoza LR. Minocycline induced lupus and autoimmune hepatitis. J Rheumatol 1999; 26: 1420-1. [PubMed: 10381074](22 year old woman had sudden onset of arthralgias and then jaundice after a year of minocycline for acne [bilirubin 3.2 mg/dL, ALT 916 U/L, Alk P 204 U/L, ANA 1:2560], biopsy showing chronic hepatitis, resolving rapidly upon stopping, but arthralgias required long term prednisone).
- Dadamessi I, Leduc I, Duché A, et al. [Autoimmune hepatitis and lupus syndrome associated with minocycline] Rev Med Interne 1999; 20: 930-3. French. [PubMed: 10573731](25 year old woman had two episodes of ALT elevations [peak 266 and 256 U/L, ANA 1:140 and 1:320] arising during minocycline therapy [first asymptomatic, second with arthralgias], resolving each time with discontinuation).
- Elkayam O, Yaron M, Caspi D. Minocycline-induced autoimmune syndromes: an overview. Semin Arthritis Rheum 1999; 28: 392-7. [PubMed: 10406406](Systematic review of literature on autoimmune syndromes from minocycline, 4 patterns: serum sickness, lupus-like syndrome, autoimmune hepatitis and vasculitis; usually presenting after 1-20 years, ANA common but so is pANCA, features may overlap, hepatitis most common: 66 cases reported).
- Westermann GW, Böhm M, Bonsmann G, Rahn KH, Kisters K. Chronic intoxication by doxycycline use for more than 12 years. J Intern Med 1999; 246: 591-2. [PubMed: 10620103](38 year old man took large doses of doxycycline chronically and developed repeated bouts of mild jaundice [bilirubin 3.4-5.0 mg/dL, ALT 44-118 U/L, Alk P 466 U/L] and weakness, skin discoloration and heart block, resolving upon stopping).
- Sturkenboom MC, Meier CR, Jick H, Stricker BH. Minocycline and lupuslike syndrome in acne patients. Arch Intern Med 1999; 159: 493-7. [PubMed: 10074958](Case control study in 27,688 acne patients in UK database, risk of lupus increased 8.5 fold in minocycline treated patients, not with other tetracyclines, typically long term therapy; liver involvement not mentioned; more common in women, absolute risk low).
- Colmegna I, Perandones CE, Chaves JG. Minocycline induced lupus and autoimmune hepatitis. J Rheumatol 2000; 27: 1567-8. [PubMed: 10852297](22 year old woman developed fever and polyarthralgias after 40 days of 9th course of minocycline for acne [bilirubin 4.9 mg/dL, ALT 1300 U/L and ESR 100], resolving rapidly but with prolonged rheumatological complaints requiring prednisone long term: ANA negative).
- Goldstein NS, Bayati N, Silverman AL, Gordon SC. Minocycline as a cause of drug-induced autoimmune hepatitis. Report of four cases and comparison with autoimmune hepatitis. Am J Clin Pathol 2000; 114: 591-8. [PubMed: 11026106](Four cases of minocycline hepatitis and comparison to 10 spontaneous autoimmune hepatitis cases showed no distinguishing features except resolution with stopping drug; 16-52 year old women developed liver injury 4 months to 12 years after starting minocycline [bilirubin 0.4, 1.2, 6.5 and 7.3 mg/dL, ALT 137, 343, 700, and 1288 U/L, Alk P 49, 83, 138 and 253 U/L, all ANA positive], histology showed fibrosis in 2, all responded to prednisone with resolution persisting after stopping corticosteroids).
- Lawrenson RA, Seaman HE, Sundström A, Williams TJ, Farmer RD. Liver damage associated with minocycline use in acne: a systematic review of the published literature and pharmacovigilance data. Drug Saf 2000; 23: 333-49. [PubMed: 11051220](Systematic review of cases of liver injury from minocycline in patients with acne defining two patterns – acute and chronic with different latencies, associated findings and potential outcomes).
- Pohle T, Menzel J, Domschke W. Minocycline and fulminant hepatic failure necessitating liver transplantation. Am J Gastroenterol 2000; 95: 560-1. [PubMed: 10685779](20 year old woman given minocycline for 3 years for acne developed autoimmune hepatitis, but did not stop minocycline and progressed to hepatic failure and need for transplant 2 months later [bilirubin 11.7 rising to 25.4 mg/dL, ALT 199 U/L, GGT 34 U/L, ANA positive, IgG 2220 mg/dL]).
- Tomer G, Shneider BL. Minocycline-induced hepatitis. J Pediatr Gastroenterol Nutr 2000; 30: 105-6. [PubMed: 10630451](Editorial on minocycline and liver injury in children).
- Bachmeyer C, Cadranel JF. Minocycline-induced lupus and autoimmune hepatitis: family autoimmune disorders as possible risk factors. Dermatology 2002; 205: 185-6. [PubMed: 12218241](15 year old girl treated for 3 years with minocycline for acne developed polyarthritis, but no jaundice [bilirubin normal, ALT 4 times ULN, Alk P normal, anti-DNA positive, ANA 1:1280], resolving slowly upon stopping with all tests normal at 6 months, except ANA which was still 1:320 12 months later).
- Abe M, Furukawa S, Takayama S, Michitaka K, Minami H, Yamamoto, Horiike N, et al. Drug-induced hepatitis with autoimmune features during minocycline therapy. Intern Med 2003; 42: 48-52. [PubMed: 12583618](25 year old Japanese woman developed jaundice after 1 year of minocycline therapy for acne [bilirubin 23.7 mg/dL, ALT 2074 U/L, Alk P 138 U/L, IgG 2110 mg/dL, ANA 1:160], resolving with 3 month course of prednisone, no relapse with stopping).
- Real Martínez Y, Medina S. [Acute hepatitis and minocycline] Rev Esp Enferm Dig 2003; 95: 741-2. Spanish. [PubMed: 14588070](14 year old boy developed jaundice after 5 months of minocycline therapy for acne [bilirubin 5.1 mg/dL, ALT 2376 U/L, GGT 83 U/L, IgG 1734 mg/dL, ANA negative, SMA 1:320], treated with corticosteroids for 5 months and no relapse when stopped).
- Selimoglu MA, Ertekin V. Autoimmune hepatitis triggered by Brucella infection or doxycycline or both. Int J Clin Pract 2003; 57: 639-41. [PubMed: 14529072](11 year old girl was found to have abnormal liver tests 3 weeks after finishing a 6 week course of doxycycline for acute brucellosis [bilirubin 1.2 mg/dL, ALT 222 U/L, Alk P 561 U/L, ANA negative, HLA B8 DRB1*03], a liver biopsy showing inflammation, necrosis and bridging fibrosis, improving on prednisone therapy, relapsing on stopping and ultimately requiring long term azathioprine therapy).
- Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug-induced liver injury in the United States. Liver Transpl 2004; 10: 1018-23. [PubMed: 15390328](Among ~50,000 liver transplants done in the US between 1990 and 2002, 270 [0.5%] were done for drug induced acute liver failure, none of which were attributed to minocycline, doxycycline or tetracycline).
- Björnsson E, Jerlstad P, Bergqvist A, Olsson R. Fulminant drug-induced hepatic failure leading to death or liver transplantation in Sweden. Scand J Gastroenterol 2005; 40: 1095-1101. [PubMed: 16165719](Among 103 cases of fulminant drug induced liver injury reported to a Swedish registry between 1966 and 2002, one case was attributed to doxycycline, but no other tetracycline mentioned).
- Andrade RJ, Lucena MI, Fernández MC, Pelaez G, Pachkoria K, Garcia-Ruiz E, Garcia-Munoz B, et al. Drug-induced liver injury: an analysis of 461 incidences submitted to the Spanish Registry over a 10-year period. Gastroenterology 2005; 129: 512-21. [PubMed: 16083708](Reports to a Spanish network found 461 cases of drug induced liver disease; no tetracycline was listed among the top 20 agents implicated [at least 5 cases]).
- Smith K, Leyden JJ. Safety of doxycycline and minocycline: a systematic review. Clin Ther 2005; 27: 1329-42. [PubMed: 16291409](Systematic review of overall safety of doxycycline and minocycline stressing overall low rate of adverse events [13-72 per million prescriptions]; little mention of liver toxicity).
- Galan MV, Potts JA, Silverman AL, Gordon SC. The burden of acute nonfulminant drug-induced hepatitis in a United States tertiary referral center. J Clin Gastroenterol 2005; 39: 64-7. [PubMed: 15599214](Ten year experience of 96 patients with acute liver injury, 64 were due to viral hepatitis and 32 to drugs; minocycline accounted for 4 cases and ranked second in frequency [7 from amiodarone and 4 from amoxicillin/clavulanate]).
- Chamberlain MC, Schwarzenberg SJ, Akin EU, Kurth MH. Minocycline-induced autoimmune hepatitis with subsequent cirrhosis. J Pediatr Gastroenterol Nutr 2006; 42: 232-5. [PubMed: 16456421](15 year old boy developed signs of cirrhosis after 1 year of minocycline therapy [bilirubin 2.5 mg/dL, ALT 67-83 U/L, Alk P normal, ANA 1:40, anti-DNA positive], treated with 6-mercaptopurine and prednisone with only partial response and found to have cirrhosis on follow up liver biopsy).
- Björnsson E, Olsson R. Suspected drug-induced liver fatalities reported to the WHO database. Dig Liver Dis 2006; 38: 33-8. [PubMed: 16054882](Survey of drug induced liver fatalities reported to WHO database between 1968-2003 revealed 4690 reports – 89% from the US; the list of most 21 most commonly implicated drugs did not include a tetracycline).
- Basude D, Dhawan A. Re: Minocycline-induced autoimmune hepatitis with subsequent cirrhosis. J Pediatr Gastroenterol Nutr 2007; 44: 389; author reply 389-90. [PubMed: 17325565](Letter in response to Chamberlain [2006] arguing that the child likely had a preexisting cryptogenic cirrhosis not related to minocycline therapy).
- Margolis DJ, Hoffstad O, Bilker W. Association or lack of association between tetracycline class antibiotics used for acne vulgaris and lupus erythematosus. Br J Dermatol 2007; 157: 540-6. [PubMed: 17596147](Analysis of UK database on 97,694 subjects with acne, 25% received minocycline, 16% doxycycline and 45% other tetracyclines. Hazard ratio for lupus-like syndrome was 3.11 for minocycline; no increased risk or association with doxycycline or other tetracyclines).
- Egiguren L, Minondo L, Zapata E, Castiella A. [Patient with autoimmune hepatitis and idiopathic thrombocytopenic purpura after minocycline therapy] Gastroenterol Hepatol 2007; 30: 565-6. Spanish. [PubMed: 17980139](15 year old girl developed jaundice 1 month after starting minocycline therapy for acne [bilirubin 4.4 mg/dL, ALT 1232 U/L, Alk P 555 U/L, ANA 1:1280], developing idiopathic thrombocytopenic purpura when treated with prednisone; no follow up available).
- Losanoff JE, Holder-Murray JM, Ahmed EB, Cochrane AB, Testa G, Millis JM. Minocycline toxicity requiring liver transplant. Dig Dis Sci 2007; 52: 3242-4. [PubMed: 17404879](33 year old woman developed jaundice 7 weeks after starting minocycline for acne [bilirubin 9.9 mg/dL, ALT 882 U/L, Alk P 191 U/L, ANA positivity], with subsequent worsening despite stopping drug, ultimately requiring liver transplantation; graft showed massive necrosis).
- Heaton PC, Fenwick SR, Brewer DE. Association between tetracycline or doxycycline and hepatotoxicity: a population based case-control study. J Clin Pharm Ther 2007; 32: 483-7. [PubMed: 17875115](Analysis of 2 years of Medicaid claims in California found 3377 cases of “hepatotoxicity”; 20 had received tetracycline <45 days before onset; only 4 controls had: adjusted odds ratio 3.7; not elevated for doxycycline; this despite safety record of oral tetracyclines and known hepatotoxicity of doxycycline).
- Ford TJ, Dillon JF. Minocycline hepatitis. Eur J Gastroenterol Hepatol 2008; 20: 796-9. [PubMed: 18617786](20 year old developed fatigue and jaundice 1 year after starting minocycline for acne [bilirubin 5.0 mg/dL, AST 1095 U/L, Alk P 178 U/L, ANA 1: 2560], resolving within 1-2 months of stopping accompanied by fall in ANA titers to normal).
- Meropol SB, Chan KA, Chen Z, Finkelstein JA, Hennessy S, Lautenbach E, Platt R, et al. Adverse events associated with prolonged antibiotic use. Pharmacoepidemiol Drug Saf 2008 17: 423-32. [PMC free article: PMC4269235] [PubMed: 18215001](Analysis of 3 large UK and US databases on medication use and clinical outcomes covering ~6 million patients for adverse events related to >1 month of either amoxicillin [0-1.2/100,000], ciprofloxacin [0-5.7/100,000] and doxycycline [0-0.9/100,000 person days], but no mention of liver toxicities).
- Carrascosa MF, Lucena MI, Andrade RJ, Caviedes JRS, et al. Fatal acute hepatitis after sequential treatment with levofloxacin, doxycycline, and naproxen in a patient presenting with acute Mycoplasma pneumoniae infection. Clin Ther 2009; 31: 1014-19. [PubMed: 19539102](63 year old man developed acute liver injury 1 week after starting a 3 day course of levofloxacin and 5 days after starting doxycycline [bilirubin 4.0 rising to >35 mg/dL, ALT 1577 U/L, Alk P 189 U/L], with subsequent progressive liver failure and death; biopsy showed massive necrosis).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, minocycline accounted for 3 cases, doxycycline for 3 cases and tetracycline was listed as a secondary possible cause for one).
- Chavant F, Lafay-Chebassier C, Beauchant M, Perault-Pochat MC. [Doxycycline induced hepatitis]. Gastroenterol Clin Biol 2008; 32: 825-7. French. [PubMed: 18823729](37 year old man developed fatigue 6 weeks after starting doxycycline [bilirubin 2.8 mg/dL, ALT 2322 U/L, Alk P 184 U/L, ANA 1:100], resolving within 6 weeks of stopping).
- Robles DT, Leonard JL, Compton N, Waghmare A, McDonough KA, George E, Wolgamot G, Fleckman P. Severe drug hypersensitivity reaction in a young woman treated with doxycycline. Dermatology 2008; 217: 23-6. [PubMed: 18332631](20 year old woman developed severe rash and fever 3 weeks after starting doxycycline for acne [bilirubin 2.5 mg/dL, ALT 133 U/L, Alk P 205 U/L, eosinophils 980/µL], requiring intubation and corticosteroid therapy and 3 week hospitalization, ultimately resolving).
- Maubec E, Wolkenstein P, Loriot MA, Wechsler J, Mulot C, Beaune P, Revuz J, Roujeau JC. Minocycline-induced DRESS: evidence for accumulation of the culprit drug. Dermatology 2008; 216: 200-4. [PubMed: 18182810](Review of 9 patients with DRESS syndrome due to minocycline; 8 women and 1 man, ages 15-45, onset after 16 to 60 days, 8 with liver “dysfunction”, resolving after 1 to 8 months, but two died, not of liver disease).
- Ramakrishna J, Johnson AR, Banner BF. Long-term minocycline use for acne in healthy adolescents can cause severe autoimmune hepatitis. J Clin Gastroenterol 2009; 43: 787-90. [PubMed: 19262406](3 cases of minocycline hepatotoxicity; 16 year olds with onset of jaundice 2, 13 and 24 months after starting minocycline for acne [bilirubin 19.6, 9.1 and 9.5 mg/dL, ALT 1282, 2306 and 2056 U/L, ANA 1:160-1:640], liver biopsies showing hepatitis and fibrosis; all treated with corticosteroids, 2 requiring prolonged therapy).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol 2010; 70: 721-8. [PMC free article: PMC2997312] [PubMed: 21039766](Worldwide pharmacovigilance database containing 9036 hepatic adverse drug reactions in children includes 117 cases attributed to minocycline, but no other tetracycline listed in the top 40 causes).
- Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol 2010; 105: 2396-404. [PubMed: 20648003](313 cases of drug induced liver injury were seen over a 12 year period at a large hospital in Bangalore, India; none were due to tetracyclines).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury and 25 to antituberculosis agents, including 15 to isoniazid alone [ranking first], 6 to isoniazid combined with other agents, 3 to rifampin and pyrazinamide, and 1 to dapsone).
- Björnsson E, Talwalkar J, Treeprasertsuk S, Kamath PS, Takahashi N, Sanderson S, Neuhauser M, Lindor K. Drug-induced autoimmune hepatitis: clinical characteristics and prognosis. Hepatology 2010; 51: 2040-8. [PubMed: 20512992](Among 261 cases of autoimmune hepatitis seen at the Mayo Clinic between 1997 and 2007, 24 were attributed to drugs, 11 to minocylcine, 11 to nitrofurantoin and 2 to others; all responded to corticosteroid therapy and all who were withdrawn did not relapse).
- Casella G, Villanacci V, Di Bella C, Drera E, Baldini V, Bassotti G. Acute hepatitis caused by minocycline. Rev Esp Enferm Dig 2010; 102: 668. [PubMed: 21142391](80 year old woman was found to have enzyme elevations after a year of minocycline therapy [bilirubin 2.2 mg/dL, ALT 721 U/L, GGT 107 U/L, ANA 1:320, INR 1.2], responding to corticosteroid therapy, and enzymes remained normal after their discontinuation).
- Mailhol C, Tremeau-Martinage C, Paul C, Godel A, Lamant L, Giordano-Labadie F. [Severe drug hypersensitivity reaction (DRESS syndrome) to doxycycline]. Ann Dermatol Venereol 2010; 137: 40-3. French. [PubMed: 20110067](59 year old woman developed fever, rash and facial edema 3 weeks after starting doxycycline for malaria prophylaxis [bilirubin normal, ALT 278 U/L, eosinophils 15%, atypical lymphocytosis], resolving on discontinuation).
- Leitner JM, Graninger W, Thalhammer F. Hepatotoxicity of antibacterials: Pathomechanisms and clinical. Infection 2010; 38: 3-11. [PubMed: 20107858](Review of hepatotoxicity of antibiotics; mentions that hepatotoxicity from oral tetracycline is rare ~1.5 cases per million prescriptions, whereas minocycline has been associated with either an immediate reaction with eosinophilia, dermatitis and enzyme elevations or a delayed autoimmune hepatitis-like syndrome).
- Glenn C, Feldman SR. Letter: Tetracycline-induced hepatotoxicity. Dermatol Online J 2011; 17: 14. [PubMed: 22233750](49 year old woman developed fatigue, edema, low albumin and raised alkaline phosphatase levels [bilirubin and ALT normal] 6 months after starting oral tetracycline for rosacea, albumin and alkaline phosphatase levels returning to normal upon stopping, later tolerating doxycycline).
- Czaja AJ. Drug-induced autoimmune-like hepatitis. Dig Dis Sci 2011; 56: 958-76. (Review of drug induced autoimmune hepatitis-like syndromes, most commonly caused by nitrofurantoin and minocycline, but also with hydralazine, methyldopa and more rarely with statins, fibrates, NSAIDs, various herbals and tumor necrosis factor antagonists). [PubMed: 21327704]
- Aldenhoven M, van Enk JG, Avis WA. [Minocycline-induced autoimmune hepatitis]. Ned Tijdschr Geneeskd 2013; 157: A5465. Dutch. [PubMed: 23328022](Abstract: 14 year old girl developed liver injury with positive ANA after long term use of minocycline, resolving after stopping the drug without corticosteroid therapy).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none were attributed to a tetracycline).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol 2014; 13: 231-9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, 37 of which were attributed to an antibiotic, but none to a tetracycline).
- deLemos AS, Foureau DM, Jacobs C, Ahrens W, Russo MW, Bonkovsky HL. Drug-induced liver injury with autoimmune features. Semin Liver Dis 2014; 34: 194-204. [PubMed: 24879983](Review of drug induced autoimmune hepatitis with examples due to methyldopa, hydralazine, minocycline and nitrofurantoin).
- Douros A, Bronder E, Andersohn F, Klimpel A, Thomae M, Sarganas G, Kreutz R, et al. Drug-induced liver injury: results from the hospital-based Berlin Case-Control Surveillance Study. Br J Clin Pharmacol 2015; 79: 988-99. [PMC free article: PMC4456131] [PubMed: 25444550](Among 76 inpatients with hepatitis of uniknown cause enrolled in a prospective case-cohort surveillance study between 2002 and 2011, one was attributed to doxycycline, but no other tetracycline was implicated).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 323 [36%] were attributed to antibiotics including 28 [3%] to minocycline and 4 [0.4%] to doxycycline).
- Urban TJ, Nicoletti P, Chalasani N, Serrano J, Stolz A, Daly AK, Aithal GP, et al; Drug-Induced Liver Injury Network (DILIN); Pharmacogenetics of Drug-Induced Liver Injury group (DILIGEN); International Serious Adverse Events Consortium (iSAEC). Minocycline hepatotoxicity: clinical characterization and identification of HLA-B∗35:02 as a risk factor. J Hepatol 2017; 67: 137-44. [PMC free article: PMC5634615] [PubMed: 28323125](The uncommon HLA allele B*35:02 was found in 4 of 25 [16%] of patients with minocycline hepatotoxicity vs 0.6% in a population control group; those with and without this allele did not different in clinical features or outcome).
- de Boer YS, Kosinski AS, Urban TJ, Zhao Z, Long N, Chalasani N, Kleiner DE, Hoofnagle JH; Drug-Induced Liver Injury Network. Features of autoimmune hepatitis in patients with drug-induced liver injury. Clin Gastroenterol Hepatol 2017; 15: 103-12. [PMC free article: PMC5370577] [PubMed: 27311619](Among 88 cases of drug induced liver injury, auotimmune features were found in 83% of nitrofurantoin, 74% of minocycline, 60% of methyldopa and 43% of hydralazine associated cases. ANA and SMA titers and IgG levels tended to fall with recovery, and cases with autoimmune features were similar clinically to those without except for a tendency for a longer latency to onset in those with autoantibodies).
- Harmon EG, McConnie R, Kesavan A. Minocycline-induced autoimmune hepatitis: a rare but important cause of drug-induced autoimmune hepatitis. Pediatr Gastroenterol Hepatol Nutr 2018; 21: 347-50. [PMC free article: PMC6182477] [PubMed: 30345250](17 year old male developed jaundice 5 months after starting minocycline [100 mg daily] for acne [bilirubin 10.2 rising to 21.8 mg/dL, ALT 2229 U/L, Alk P not given, ANA negative], biopsy showing autoimmune-like features leading to a 12 week course of prednisone and ultimate recovery).
- Shankar S, Oliver MR. Primum non nocere: minocycline-induced liver injury in a teenager. J Paediatr Child Health 2018; 54: 1031-3. [PubMed: 29962030](15 year old girl developed fever, rash, lymphadenopathy and abdominal pain 4 weeks after starting minocycline [100 mg daily] for acne [bilirubin normal, ALT 688 U/L, GGT 281 U/L, eosinophils 500/mcL], treated with corticosteroids and had fully recovered when seen 6 months later).
- Shah J, Shahidullah A, Liu Y. Drug-induced autoimmune hepatitis in a patient treated with minocycline: a rare adverse effect. Case Rep Gastroenterol 2018; 12: 447-52. [PMC free article: PMC6120419] [PubMed: 30186098](31 year old woman developed nausea and abdominal pain 3 months after starting minocycline for acne [bilirubin 1.8 mg/dL, ALT 1138 U/L, Alk P 160 U/L, INR 1.9, ANA 1:160, IgG 3176 mg/dL], with a rapid response to prednisolone [given for 4 weeks] and ultimate complete recovery).
Publication Details
Publication History
Last Update: January 23, 2019.
Copyright
Publisher
National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda (MD)
NLM Citation
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Minocycline. [Updated 2019 Jan 23].