NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LeBlanc EL, Patnode CD, Webber EM, et al. Behavioral and Pharmacotherapy Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults: An Updated Systematic Review for the U.S. Preventive Services Task Force [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018 Sep. (Evidence Synthesis, No. 168.)
Included Studies
Our literature search resulted in 15,483 unique citations. For these, we provisionally accepted 572 articles for full-text review based on titles and abstracts (Appendix C). Following review of full-text articles and critical appraisal, we included 124 trials of weight loss or weight loss maintenance interventions160, 161, 168, 172, 173, 205, 206, 213-330 reported in 238 publications (Appendix D). Of the included trials, 80 trials examined the effectiveness and/or harms of behavior-based weight loss interventions,205, 206, 214, 215, 217, 219, 221, 224, 225, 228-232, 234, 235, 237, 240, 242, 243, 245, 249-258, 261, 262, 264-267, 269-272, 274-281, 283, 286, 288-291, 293, 295, 300-302, 305, 306, 308, 310, 314-316, 318-330 and 32 examined the effectiveness and/or harms of medication for weight loss160, 161, 168, 172, 173, 213, 216, 218, 220, 222, 226, 227, 236, 238, 239, 241, 244, 246, 248, 259, 260, 263, 268, 273, 285, 292, 297-299, 304, 307, 311 (Table 2). An additional 12 trials (nine behavior-based223, 233, 282, 284, 294, 296, 303, 309, 313, 317 and three medication-based247, 287, 312) evaluated the effectiveness of a weight loss maintenance intervention. We carried forward 41 studies from our prior review and added 83 new studies (Table 2).
Of the 572 articles that were reviewed, the most common reasons for exclusion were: a lack of relevant outcomes (k=51), less than 12-month followup (for effectiveness studies) (k=59), and a lack of an appropriate comparator (comparative effectiveness, controls told specifically not to lose weight) (k=92). Appendix E contains a list of all excluded studies and their reasons for exclusion.
Given the diversity of interventions included in this review, we organized the results by: 1) behavior-based weight loss interventions (k=80), 2) behavior-based weight loss maintenance interventions (k=9), 3) medication-based weight loss interventions (k=32), and 4) medication-based weight loss maintenance interventions (k=3). Weight loss maintenance trials are those in which participant randomization occurred after weight loss (either as part of or outside of the study).
Study and Population Characteristics
Behavior-Based Weight Loss Interventions
Of the 80 behavior-based weight loss trials, 20 were carried forward from the previous review and 60 new studies were added (Table 2). All of the included studies were RCTs; 11 were cluster RCTs with randomization of health centers or primary care practices, physicians, or families.214, 225, 231, 232, 235, 269, 271, 318, 320, 329, 330 Sample sizes ranged from 30 to 2161, and the median sample size was 240. Followup at 12 months ranged from 57 to 100 percent. The majority of the trials (k=47) took place in the United States, and the remaining trials were conducted in Europe (k=15), the United Kingdom (k=11), Japan (k=3), Australia (k=2), and Canada (k=2). Recruitment varied, with at least some self-selected into the trial based on broad-based recruitment methods (35 trials), or direct recruiting through methods such as targeted mailings or appointments with their primary care providers (PCPs) (40 trials). The remaining trials applied mixed recruitment methods.
Half of the behavior-based weight loss trials represented a general, unselected population of adults who were eligible for participation based on their BMI alone (k=40) (with or without other demographic limitations [e.g., age, race/ethnicity]) (Table 3). Five additional trials specifically enrolled adults at elevated cancer risk (i.e., cancer survivors, those with colorectal adenomas).217, 229, 235, 288, 310 The remaining 35 trials selected participants based on increased subclinical (k=19) (e.g., prediabetes, family history of diabetes, high-normal blood pressure) or clinical (k=16) (e.g., hypertension, dyslipidemia) cardiovascular risk. Across all 80 trials, regardless of participant selection into the trials, cardiovascular risk status of the participants was underreported and variable among those that did report baseline prevalence. Among those that reported risk status, the proportion of affected participants varied broadly: prediabetes (8.5% to 100%; k=16), diabetes (0% to 43%; k=49), hypertension (0% to 100%; k=24), and dyslipidemia (0% to 67.7%; k=12).
The majority of trials (k=71) included adults who were overweight or had obesity, with eight trials limited to adults with obesity (i.e., BMI ≥30 kg/m2) and one trial limited to adults who were overweight (BMI 25 to 29.9 kg/m2).251 Very few trials placed an upper bound for eligible BMIs; in those that did, the upper bound ranged from 29.9 kg/m2 (in the only trial limited to adults who were overweight) to 60 kg/m2. The mean baseline BMI ranged from 25.2 kg/m2 (among a sample of Japanese adults ages 50 to 69 years) to 39.2 kg/m2 (among a sample of African American women ages 30 to 65 years) with a median of 33.4 kg/m2. The standard deviations (SDs) were large, indicating that there was a wide range of baseline BMIs and that baseline BMIs overlapped, even among trials with different BMI inclusion criteria (Figure 2). Only five trials225, 265, 270, 286, 291 included eligibility criteria based on central adiposity (i.e., waist circumference).
The mean age of included participants ranged from 22.4 to 66.0 years (median, 50.3 years). While none of the trials restricted participation to older adults, the mean age was older than 60 years in six trials.217, 229, 235, 243, 270, 326 One trial focused on college students ages 18 to 35 years.242 Four trials were limited to men249, 272, 281, 286 and 14 were limited to women.229, 234, 235, 240, 250, 261, 269, 277, 288, 289, 295, 310, 321, 330 Of the trials restricted to women, some were further restricted to specific subgroups of women, including women with a history of breast229, 235, 288 or endometrial cancer,310 postpartum women,250, 277, 330 and African American women.240, 269 Eleven trials focused on specific racial/ethnic groups, including African Americans,240, 269 Asians257, 270, 274, 316 and South Asians,225 American Indian,276 or those of Hispanic ethnicity.278, 290, 321 There was no consistent reporting of socioeconomic status of the participants; however, based on the variables that were reported, most of the sample represented adults with medium to high socioeconomic status based on education, income, and employment.
Behavior-Based Weight Maintenance Interventions
Of the nine behavior-based weight loss maintenance trials, three were carried forward from the previous review (Table 2). The nine studies included eight RCTs and one cluster RCT (randomized based on assignment to a previous weight loss intervention).233 Sample sizes ranged from 92 to 1032 (median, 201), with a followup of 74 to 95 percent at 12 to 18 months. The majority of the trials (k=6) took place in the United States, and the remaining trials were conducted in the United Kingdom, Finland, and Australia. Recruitment procedures varied across trials, but at least some of the participants self-selected into the trials as a result of broad-based recruitment methods such as advertising with the community, health insurance, or PCP.
All but one behavior-based weight loss maintenance trial represented a general, unselected population of adults who were eligible for participation based on BMI alone (k=8), with one trial specifically enrolling adults with cardiovascular risk (i.e., hypertension and/or dyslipidemia) (Table 3).303 Six trials233, 282, 284, 303, 309, 317 conducted weight loss interventions prior to randomizing participants into the maintenance interventions, with three trials randomizing only those with at least 4 kg of weight loss.233, 282, 284 The mean BMI at enrollment in these trials was 34.2 kg/m2. The remaining three trials selected patients based on achieving a weight loss of 5 to 10 percent in the 1 to 2 years before randomization and did not include weight loss as part of the trial (mean BMI, 33.1 kg/m2).294, 296, 313
The mean age of included participants across studies ranged from 46.4 to 61.8 years (median, 49.2 years). One study examined only women,233 and one was limited to men.317 The majority of studies did not report information regarding participant race/ethnicity or socioeconomic status. Based on the limited information available, the study populations appeared to be majority white (percent of nonwhite participants ranged from 5.4% to 41.9%) with medium to high socioeconomic status based on limited data on education, income, and/or employment.
Medication-Based Weight Loss Interventions
Of the 32 medication-based weight loss studies, 16 were carried forward from the previous review (all related to orlistat) and 16 new studies were added (Table 2). Among the 32 studies, 20 RCTs were included in the review of the benefits of weight loss medications (KQ1 and KQ2), and all of the studies (30 RCTs, one retrospective cohort, and one event monitoring study) were included in the review of potential harms of medications (KQ3). Sample sizes ranged from 48 to 3731 in the RCTs (median, 542). About one-half of the trials (k=15) took place solely in the United States. The remaining trials were conducted in Europe (k=14), Australia/New Zealand (k=1), and multiple countries/regions (k=2). Fourteen studies had run-in periods to assess compliance with taking the medication. The trials that examined health outcomes (KQ1 and KQ2) lasted 12 to 48 months, with six trials contributing outcome data at 24 months or longer.160, 161, 172, 220, 241, 246, 285, 292, 297 Of the trials included for the effectiveness of weight loss, followup at 12 to 18 months ranged from 50 to 96 percent. The body of evidence regarding harms (KQ3) also included trials with shorter followup (1 to 6 months). The retrospective cohort and event monitoring study examined harms over a median of 150 days to 3 years.213, 248
The majority of studies recruiting from academic, research, or specialty care settings; recruitment procedures were not well described. Five trials specifically reported conducting at least some communitywide recruitment (via local advertising).161, 220, 239, 259, 297 One trial recruited participants from a primary health care setting,246 and two studies were conducted in a primary care setting.246, 263
Almost two-thirds of the weight loss medication trials (21 of 30 trials) were conducted in generally unselected populations based on their BMI alone. Thirteen of these trials in unselected populations required BMI to be greater than or equal to 30 kg/m2 but allowed those with BMIs greater than or equal to 27 kg/m2 if cardiovascular risk factors were present.160, 161, 168, 172, 173, 216, 218, 220, 239, 244, 246, 285, 311 One trial selected participants based on the presence of prediabetes,259 and eight trials selected those with one or more cardiovascular risk factors (e.g., hypertension, dyslipidemia).222, 226, 227, 236, 241, 263, 273, 304 Across all 30 trials, cardiovascular risk status of the participants was underreported. In those reporting risk status, 1 to 68 percent had prediabetes (k=8), 0 to 27 percent had type 2 diabetes (k=21), 0 to 100 percent had hypertension (k=11), and 21 to 100 percent had dyslipidemia (k=13). Overall, approximately two-thirds of the trials (k=19) included adults who were overweight or had obesity, with 11 trials limited to adults with obesity (BMI ≥30 kg/m2). The mean baseline BMI ranged from 31 to 42 kg/m2 (median, 36.1 kg/m2). The large SDs indicate a wide range of baseline BMIs that overlapped among trials with different BMI inclusion criteria (Figure 3). No trial had eligibility criteria based on central adiposity (i.e., waist circumference).
The mean age of included participants ranged from 41 to 58 years (median, 45 years). All studies comprised both men and women (25% to 90% female), with all but one study299 including more females than males. Of the 18 trials that reported race/ethnicity of the sample, the percent of nonwhite participants ranged from 5 to 37 percent. No trials focused on specific racial/ethnic groups and there was no reporting of socioeconomic status. Baseline characteristics were similar in the two non-RCT studies.213, 248
Medication-Based Weight Maintenance Interventions
Two medication-based weight loss maintenance trials were carried forward from the previous review,247, 287 and one new trial was added (Table 2).312 All were RCTs conducted in research clinics and were set in the United States, Canada, and Scandinavia. Sample sizes ranged from 309 to 542, with a followup of 65 to 74 percent at 12 to 36 months. All three trials began with an active weight loss phase, which lasted for 4 to 24 weeks, during which all participants were prescribed hypocaloric diets and exercise with no pharmacologic intervention. Participants were required to lose 5 to 8 percent of their baseline weight prior to randomization to the maintenance intervention. One trial was limited to adults with at least one cardiovascular risk factor. The mean baseline BMI at enrollment into the maintenance phase ranged from 32.8 to 37.5 kg/m2.287 The mean age of included participants was 46 to 47 years, with the majority of the participants being female (51% to 84%) and white (12% to 16% nonwhite). There was no reporting of socioeconomic status.
Intervention Characteristics
Behavior-Based Weight Loss Interventions
Within the 80 weight loss trials, 105 unique weight loss interventions were evaluated against control conditions (Table 4). The interventions were highly variable across the included trials in terms of the modes of delivery, number of sessions and contacts, and interventionists. However, specific weight loss messages and behavior change techniques were consistent across the trials (Table 5; Appendix F Table 1). Duration of interventions ranged from 3 months (in six trials) to 5 years (in one trial), with the majority taking place for a minimum of 1 year. One-third of interventions provided a “core” intervention period (described as “core,” “active,” or “intense” phases) generally for 3 months to 1 year and then followed up with a support phase (also described as “maintenance” in some trials), generally for 9 to 12 months. The remaining interventions did not distinguish between “core” and “support” phases.
To better summarize the interventions, we categorized each intervention arm according to the main mode of intervention delivery into the following groups: 1) group, 2) individual, 3) mixed, 4) technology-based, and 5) print-based (Table 4). Across the 105 intervention arms, one-third (35 arms in 25 trials) were primarily group-based counseling interventions.214, 215, 221, 230, 243, 249, 253-255, 261, 262, 266, 267, 270, 276, 280, 295, 300, 301, 314, 316, 321, 323, 327, 329 Group-based interventions ranged from eight group sessions over 2.5 months to 52 weekly group sessions over 1 year (median, 23 total sessions in the first year). Twelve interventions (in seven trials254, 261, 300, 301, 314, 327, 329) provided group sessions beyond 1 year (1.5 to 3 years total intervention time). Groups typically consisted of classroom-style sessions with 8 to 12 participants per group, and each session lasted 1 to 2 hours. Within the group-based interventions, five trials (nine arms) provided referral and free access to commercially available group-based weight loss programs including Weight Watchers,253, 255, 267, 323 Slimming World221, 255 and the Size Down program255 (both provided by the U.K. National Health Service), and Rosemary Conley (U.K.-based weight loss program).255 Six of the group-based interventions offered minimal supplemental support, with one brief individual counseling session.214, 221, 300, 301, 327, 329
In 30 trials (with 33 arms), the main mode of intervention delivery was individual-based support.205, 206, 217, 219, 224, 225, 229, 232, 234, 237, 250, 252, 255, 257, 265, 269, 271, 275, 283, 286, 289, 291, 305, 306, 308, 318, 320, 324, 325, 328 In most of these (24 arms), counseling was provided through face-to-face intervention sessions with or without ongoing telephone support. The remaining nine individual-based interventions were provided remotely through telephone counseling calls (average 15 to 30 minutes) and Web-based self-monitoring and support. One trial evaluated three individual-based strategies that included telephone support only, a mailed food basket only, and telephone support plus the mailed food basket.320 In general, the individual-based counseling interventions had fewer sessions or contacts than the group-based interventions; the median number of sessions in the first year for individual-based interventions was 12 compared with 23 in group-based interventions. DPP was the most intense individual-based intervention, offering participants weekly and then bimonthly individual counseling sessions with case managers over 3 years.205 Another example of an intense individual intervention was one that offered free access to weekly individual counseling sessions through Jenny Craig.289
We categorized 17 interventions (within 15 trials219, 228, 240, 251, 256, 258, 274, 278, 288, 290, 302, 310, 315, 326, 330) as “mixed” interventions as they included relatively equal numbers of group- and individual-based counseling sessions with or without other forms of support (telephone, print, Web-based). All but four of these interventions took place for more than 1 year, and most had more than 12 sessions in the first year (median number of sessions [23] was same as median for group-based interventions).
In another 18 interventions (16 trials), the main component of the intervention was technology-based, including computer- or Web-based intervention modules,231, 264, 272, 277, 279, 281, 308, 315 Web-based self-monitoring, mobile phone-based text messages, smartphone applications, or social networking platforms,242, 245, 265, 293, 302, 319, 322 or DVD learning.266 In all but two of these interventions,231, 264 there was no face-to-face interaction with an interventionist. There was only one trial (two arms) that delivered its intervention entirely through print-based tailored materials.235
Across all intervention types, 19 interventions included interaction with a PCP, although the level of interaction with the provider was variable across the interventions.206, 219, 221, 224, 231, 232, 237, 255, 257, 269, 271, 305, 310, 318, 324, 327, 328 In three of these interventions, PCP involvement was limited to encouragement to take part in and/or referral to interventions conducted by other providers (i.e., group-based interventions conducted by lifestyle coaches or registered dietitians) or in other settings (i.e., commercial weight loss program).219, 221, 224 In seven trials, PCPs reinforced intervention messages through brief counseling sessions.206, 231, 237, 310, 324, 327, 328 A PCP was the primary interventionist in only six interventions, providing 3 to 12 months of individual counseling.232, 255, 257, 269, 305, 318 The intervention providers were highly diverse in the remaining trials not involving PCPs and included behavioral therapists, psychologists, registered dietitians, exercise physiologists, lifestyle coaches, and other study-hired medical or public health staff. Most trials included interventionist training prior to the start of the intervention; in those that gave specific details (k=43), training was fairly intense, ranging from 2 hours to 4 days as well as regular check-ins or supervised sessions to ensure fidelity to the intervention protocol. In one trial,271 the focus of the intervention was to educate PCPs on the benefits of weight loss and effective treatment options through small group meetings. Each practice was then asked to devise an individual weight management protocol for their patients who had obesity to help them achieve 10 percent loss of their body weight.
The trials had very similar messages in terms of specific weight loss and behavioral goals. Most of the interventions were designed to help participants achieve a 5 percent or greater weight loss through a combination of dietary changes (including specific caloric goals) and a gradual increase in physical activity (generally promoting at least 150 minutes of moderate-intensity activity per week). A few trials mentioned promoting specific dietary approaches including the DASH diet (Dietary Approaches to Stop Hypertension),228, 302, 320 a Mediterranean food pattern,291 or the Magedeburg Dual Diet (500 kcal/day reduction and consumption of low-glycemic index foods).265 Only one trial314 encouraged a very low-calorie diet (800 to 1000 kcal/day). In two trials,254, 289 prepackaged meals were provided directly to participants. In one trial,256 the intervention was exclusively focused on dietary changes and participants were specifically told not to exercise.
In addition to group, individual, and technology-based education and counseling, most interventions provided additional tools to assist with weight loss (e.g., pedometers, food scales, exercise videos). One intervention provided monetary incentives for weight loss.254 Most of the trials targeted individual participants, but a few encouraged participants to invite family members to join intervention activities228, 243, 300, 301, 306, 316, 320 and two specifically targeted family pairs or units (i.e., mother-daughter pairs235 or adult relatives225).
Twelve trials (14 intervention arms) provided interventions modeled closely after the DPP lifestyle intervention for application in the community214, 215, 230, 258, 277, 278, 290, 316, 319, 321 or primary care.266, 328 A number of these trials tailored the DPP intervention for a specific population (e.g., Latinos, postpartum women with recent gestational diabetes) and included additional intervention components such as individual counseling sessions with community health workers. All but one328 of these trials were among adults at increased diabetes (9 trials) or cardiovascular risk (2 trials). Three of the trials adapted the DPP core curriculum to be provided strictly by DVD,266 text messages,319 or a Web site.277 Three additional trials described using or adapting DPP materials as part of their interventions but did not closely follow the DPP framework and were conducted among unselected adults or those at low cardiovascular and diabetes risk.237, 261, 305
In general, rates of participation or participant adherence were relatively high (Appendix F Table 1). Most of the studies reported that more than two-thirds of the intervention participants completed the full intervention, or alternatively, that all participants completed more than two-thirds of the intervention. However, participation rates appeared to decline over time, especially as intervention intensity lessened. This pattern held true even among interventions that were primarily technology-based.
The majority of trials employed a minimal weight loss intervention (k=41) or usual care (k=23) arm for the control group (Appendix F Table 1). Most of the minimal intervention and usual care groups consisted of generic self-help print or Web-based materials focused on weight loss, diet, and physical activity changes, and diabetes prevention (e.g., the NHBLI’s “Aim for a Healthy Weight” brochure). A handful, however, were more intense and included 30 minutes to 2 hours of nontailored group weight-loss counseling sessions, brief (2 to 3 minutes) quarterly counseling sessions with a PCP, or more intense individualized counseling two to four times per year.205, 225, 237, 265, 267, 272, 288, 289, 305, 306, 324, 326, 328, 329
Behavior-Based Weight Maintenance Interventions
Within the nine behavior-based maintenance trials,233, 282, 284, 294, 296, 303, 309, 313, 317 there were 15 unique weight loss interventions evaluated against control conditions; four trials had more than one active intervention arm compared with a control condition (Table 6; Appendix F Table 2). The maintenance interventions included group interventions (six arms),282, 284, 313 technology-based (four arms),233, 303, 313, 317 individual counseling sessions conducted in person or by phone (four arms),294, 296, 303 or a combination of individual and group counseling (one arm)309 (Table 7). Duration of the maintenance interventions ranged from 6 months to 5 years, with the majority taking place for 12 to 18 months. The number of sessions within the first year ranged from 0 (Web-based self-monitoring only) to 26, with the majority of the interventions having greater than 12 sessions in the first year. Only one study, which included four intervention arms, specifically reported that the intervention included interaction with a PCP (physician or nurse) paired with a clinical psychologist.284
The interventions were designed to help participants maintain weight loss by continuing dietary changes and physical activity. There was a focus on reviewing nutrition, exercise, and behavioral topics as well as self-monitoring, identifying barriers, problem-solving, peer support, and relapse prevention. Programs also provided participants with tools to assist in weight loss maintenance (e.g., food diaries, pedometers) and one intervention included monetary incentives for program adherence.284
In most trials, the majority of the sessions were attended or contacts completed during the first 6 to 12 months (Appendix F Table 2). However, similar to the trials of behavior-based weight loss interventions, participation began to drop off, especially beyond 12 months.
Following an administered weight loss intervention233, 282, 284, 303, 309, 317 or after study enrollment,294, 296, 313 the control groups received either no intervention (k=4),233, 282, 284, 317 minimal intervention (e.g., generic self-help print or Web-based materials or minimal phone contact) (k=3),294, 303, 313 or usual care (e.g., care offered as part of health plan enrollment) (k=2).296, 309
Medication-Based Weight Loss Interventions
All of the medication-based weight loss studies examined FDA-approved dosages of medications (Table 8): liraglutide at 1.8 mg QD or 3.0 mg QD, lorcaserin at 20 mg (10 mg BID), naltrexone and bupropion at 32/360 mg (16/180 mg TID), orlistat at the prescription strength dosage of 360 mg daily (120 mg TID) and over-the-counter dosage of 180 mg (60 mg TID), and phentermine-topiramate at 15/92 mg and 7.5/46 mg. We did not abstract data on nonapproved dosages.
Within all trials, both groups received identical behavioral interventions. Participants were told to follow energy-restricted diets (generally with a 500- to 800-kcal/day deficit) and increase physical activity in addition to taking the medication. The extent of the behavior-based component of the intervention varied widely among studies—from a single visit with a study physician246 to weekly, 90-minute group sessions.311 The most common behavior-based intervention was to require participants to complete food records that were discussed with nutritionists at study visits (which ranged from monthly to quarterly).
Medication adherence was rarely reported; however, almost all trials reported the percentage of participants who completed the trial on the drug/placebo. Completion rates ranged from 10 to 93 percent, with most studies having completion rates between 50 and 70 percent. Of note, completion rates tended to be higher among the intervention groups than control groups.
Medication-Based Weight Maintenance Interventions
Three trials examined the effect of medication on weight loss maintenance following a weight loss intervention. Two medication-based weight loss maintenance studies examined orlistat, one at the prescription strength dosage of 360 mg daily (120 mg TID)287 and one at both prescription and over-the-counter strengths (180 mg [60 mg TID]),247 and one study examined liraglutide 3.0 mg QD (Table 8).312 During the maintenance phase, participants were prescribed energy intakes to either maintain weight or result in a 500- to 600-kcal/day energy restriction, were encouraged to exercise regularly, and met with dieticians or behavioral counselors. While no trials reported on pill compliance, the percentage of participants who completed the trial on the drug/placebo ranged from 70 to 77 percent in the two trials that reported these data.
Study Quality
Within the 89 included behavior-based weight loss and weight loss maintenance trials, we rated 26 as good quality and the remaining 63 as fair quality (Table 2). One study included in KQ3 (harms) had intermediate health outcome data, but these data were not evaluated as the study was rated poor quality for KQ1 and KQ2 because of greater than 20 percent differential attrition.320 In general, the 26 good-quality trials were characterized by valid randomization procedures, comparable groups at baseline (or adequate adjustment for known baseline differences in the analysis), high sample retention (i.e., ≥85% retention at 12 months), the use of reliable and valid measurement instruments applied equally across arms, evidence of fidelity to the intervention protocol, no evidence of selective outcome or analysis reporting, and appropriate analyses, including intention-to-treat principles using multiple imputation or other conservative data imputation procedures for missing data (e.g., baseline observation carried forward). Most of the trials rated as good quality included published design papers or protocols with extensive details on their randomization methods, procedures for maintaining fidelity to the intervention, and data analysis plans. Additionally, several of the good-quality trials were multisite trials with data coordinating centers, including the three POWER trials,206, 219, 224, 331 TOHP phases I and II,300, 301 the TONE trial,326 and DPP.205 Some common limitations of the fair-quality studies included lack of reporting details about allocation concealment, relatively higher (i.e., >20%) and differential attrition between groups, and no attempt (or lack of reporting) to account for missing data or only completers-only analyses. The main risks of bias for the 12 behavior-based intervention studies we rated as poor quality included differential attrition between intervention arms (approximately 10% to 30% differential attrition) with completers-only analyses or unclear methods for handling missing data coupled with other issues in trial conduct, analysis, or reporting of results (e.g., intervention fidelity, possible selective reporting, inappropriate exclusion of participants from analyses, questionable validity of randomization and allocation concealment procedures). In addition, three of the studies excluded for poor quality used different procedures for measuring participants’ weight at baseline and followup. In these trials, baseline weight was objectively measured using standard protocols, whereas weight at followup was self-reported by participants for the full or partial sample and the percent of self-reported weights was not reported by treatment group.
All 35 of the medication trials were rated as fair quality; none were rated as good quality (Table 2). One study included in KQ3 (harms) had intermediate health outcome data, but these data were not evaluated as the study was rated poor quality for KQ1 and KQ2 because of greater than 20 percent differential attrition early on in the study with limited data substitution methods.222 In addition, one study only eligible for inclusion for KQ3 (harms) was excluded for poor quality due to incomplete description of the collection and reporting of adverse events.332 The biggest threat to internal validity within this body of evidence is high rates of attrition and missing data, which is a substantial and frequent issue in weight loss medication trials.201 Because most dropouts are due to adverse events or lack of effectiveness of the intervention and not study design flaws, we rated studies with high attrition as fair quality if they used adequate data substitution methods with sensitivity analyses evaluating various substitution methodologies. A study evaluating data substitution methods in obesity medication trials concluded that data substitution methods were generally adequate for protecting against false-positive and false-negative results in the majority of medication weight loss trials.201
KQ1. Do Primary Care–Relevant Behavioral and/or Pharmacotherapy Weight Loss and Weight Loss Maintenance Interventions Lead to Improved Health Outcomes Among Adults Who Are Overweight or Have Obesity and Are a Candidate for Weight Loss Interventions?
Summary of Results
Health outcomes were minimally reported in the behavior-based weight loss and maintenance trials (k=20; n=9910). In four weight loss trials (n=4442) reporting mortality, there were no significant differences between groups over 2 to 16 years. Two weight loss trials (n=2666), reported on cardiovascular events, with neither finding differences between groups over 3 and 10 years. Health-related QOL was evaluated in 17 weight loss and maintenance trials (n=7120), with almost all showing no differences between groups.
Trials of medications for weight loss examined few health outcomes beyond QOL (k=10; n=13,145). Although there was evidence of greater improvement on an obesity-specific QOL scale in those randomized to medications for weight loss compared with placebo within most of the trials, the differences were small and of unclear clinical significance, especially given high dropout rates in medication trials. None of the medication-based maintenance trials reported the effects of the interventions on health outcomes.
Detailed Results
Behavior-Based Weight Loss Interventions
Eighteen trials reported the effects of behavior-based weight-loss interventions on at least one health outcome (n=9543);205, 206, 219, 234, 235, 243, 249, 252, 262, 275, 278, 288, 301, 306, 310, 315, 323, 326 we rated half of these trials as good quality. Thirteen of the 18 trials were newly identified as part of our update; the remaining 5 trials–which included the DPP, the Finnish DPS, PREDIAS, TOHP Phase II, and TONE–were included in our previous review.
All-Cause Mortality
Four good-quality trials (n=4442), all included in our previous review, reported the effect of the intervention on all-cause mortality.205, 301, 306, 326, 333-335 Overall, few deaths occurred in the three trials of adults (ages 25 to 65 years). One trial in older hypertensive adults (ages 60 to 80 years) found higher overall rates of death in both arms; however, none of the four trials found significant between-group differences in mortality over 2 to 16 years of followup. After approximately 4.5 years of followup, DPP (n=2161) found that the placebo group had a nonsignificant higher mortality rate per 100 person-years compared with the lifestyle intervention group (0.2 vs. 0.1).205 In Phase II of TOHP, a hypertension prevention trial (n=1191), 5 versus 2 participants in the intervention and control groups died, respectively, over 2 years.301, 333 The Finnish DPS (n=505) found no significant difference in all-cause mortality after 10.2 years of followup with 6 versus 10 deaths in the intervention versus control groups (hazard ratio [HR], 0.57 [95% CI, 0.21 to 1.58]).306, 334 Finally, TONE (n=585), a study in hypertensive adults ages 60 to 80 years, found no significant difference in the all-cause mortality after 16 years of follow up (HR, 0.82 [95% CI, 0.55 to 1.22]).335
CVD
The DPP205, 336 and the Finnish DPS306, 334 trials (n=2666) reported on the incidence of cardiovascular events over the course of the study, including stroke or myocardial infarction. There was no statistically significant difference between groups on the number of participants in the intervention groups of DPP and DPS who experienced cardiovascular events compared with control participants after 3 and 10 years of followup, respectively.205, 306 Within DPP, nonfatal cardiovascular events occurred in 2.2 percent of lifestyle intervention participants (9.7 events/1000 patient-years) (n=1079) compared with 1.7 percent of placebo participants (7.3 events/1000 patient-years) (n=1082), which was not statistically different.336 Cardiovascular-related deaths occurred in only 2 and 4 participants in the lifestyle and placebo groups, respectively.336 In the Finnish DPS trial, after 10.2 years, there were 57 new cardiovascular events (22.9 per 1000 person-years) in the intervention group and 54 events (22.0 per 1000 person-years) in the control group (HR, 1.04 [95% CI, 0.72 to 1.51]).334
Health-Related QOL and Depression
Fifteen trials (n=6893 examined health-related QOL outcomes) (Table 9).205, 206, 219, 234, 235, 243, 249, 252, 262, 275, 278, 288, 310, 315, 323 The data were limited in that only six trials presented absolute changes in QOL scores; the remaining just reported whether or not there were significant differences between groups in QOL outcomes. Three of 14 trials found statistically significantly greater improvement on the physical component summary score (but not the mental component summary score) after 1 to 3 years of followup among intervention participants versus control participants (absolute between-group differences ranging from 1.5 to 2.5 points on a 100-point scale).205, 215, 249 There were no other significant differences between groups on other measures of QOL.
None of the included trials reported the effect of the intervention on the incidence or prevalence of depression over the course of the study. Two trials (DPP and the Finnish DPS) reported the prevalence of participants on antidepressant medications after 3 to 4 years of followup and found no significant differences across treatment arms.337, 338
Behavior-Based Weight Loss Maintenance Interventions
The only health outcome reported in behavior-based weight loss maintenance interventions was QOL, which was evaluated in two trials; both found no significant effects after 1 to 2 years of followup (Table 9).282, 296
Medication-Based Weight Loss Interventions
Ten of 32 medication-based weight loss trials reported the effects of the intervention on health outcomes, including QOL (10 trials) and cardiovascular events (two trials).172, 173, 218, 220, 241, 244, 285, 292, 304, 311 In general, findings related to health outcomes were limited by reduced long-term followup, with many trials reporting rates of 35 to 55 percent loss to followup by 12 to 24 months (Table 2, Table 8).
CVD
Liraglutide. Within one trial (n=3723), there were three cardiovascular events in both the liraglutide and placebo arms (0.12% and 0.24%, respectively) after 13 months (statistical testing not reported).285 Participants with prediabetes at baseline (n=2201) were followed for an additional 23 months (total of 36 months), with an additional two cardiovascular events in those randomized to liraglutide and none in the placebo arm (statistical testing not reported).339
Phentermine and topiramate. One trial of phentermine and topiramate (n=2487) reported similarly low rates of cardiovascular events in the intervention and placebo arms (0.4%, 0.6%, and 0.7% in the 15/92 mg, 7.5/46 mg, and placebo arms, respectively) across 13 months followup (statistical testing not reported).241
QOL
Liraglutide. Two liraglutide trials examined changes in QOL (Table 10).220, 285 The smaller trial (n=196) reported QOL improvement in both arms during the first 12 months, without between-group statistical testing.220 The larger trial (n=3662) found significant improvements in QOL in those randomized to liraglutide versus placebo at 13 months (absolute between-group differences ranging from 0.9 to 3.1 points on a 100-point scale). 285 Among a subset of participants with prediabetes, there were mixed results in QOL changes at 36 months.285, 339
Lorcaserin. Two trials of lorcaserin (n=6139) examined changes in QOL at 12 months, both finding172, 173 that greater improvements in QOL were seen in those randomized to lorcaserin compared with those in the placebo arm (absolute between-group differences not reported; p<0.001) (Table 10).172, 173
Naltrexone and bupropion. Three trials (n=2815) of naltrexone and bupropion examined QOL after 12 to 13 months (Table 10).218, 244, 311 All trials reported that QOL improved more in those who received naltrexone and bupropion compared with those who received placebo (absolute between-group differences not reported; p<0.001).
Orlistat. Changes in QOL were evaluated in two orlistat trials (Table 10).292, 304 One (n=333) noted a statistically significant higher score on one QOL subscale in those on orlistat compared with placebo after 12 months; however, there were no other significant differences.304 Another trial (n=481) found those randomized to orlistat for 24 months had statistically significant greater satisfaction with their medication and overall therapy, and less overweight distress.292
Phentermine and topiramate. One trial (n=2487) identified significantly greater improvements in QOL with 15/92 mg phentermine and topiramate compared with placebo (data not reported) (Table 10).241
Medication-Based Weight Loss Maintenance Interventions
None of the three trials examining the effect of medications for weight loss maintenance reported the effects of the intervention on health outcomes.
KQ2. Do Primary Care–Relevant Behavioral and/or Pharmacotherapy Weight Loss and Weight Loss Maintenance Interventions Lead to Weight Loss, Weight Loss Maintenance, or a Reduction in the Incidence or Prevalence of Obesity-Related Conditions Among Adults Who Are Overweight or Have Obesity and Are a Candidate for Weight Loss Interventions?
Summary of Results
Participants who received behavior-based weight loss interventions generally lost more weight and had greater reductions in waist circumference than those in control conditions at up to 24 months followup. Intervention participants had a pooled −2.4 kg (95% CI, −2.85 to −1.92) greater weight loss at 12 to 18 months. Mean absolute changes in weight ranged from −0.5 kg (−1.1 lb) to −9.3 kg (−20.5 lb) among intervention participants and from 1.4 kg (3.0 lb) to −5.6 (−12.3 lb) among control participants. In addition, intervention participants had a 1.94 (95% CI, 1.70 to 2.22) times greater chance of losing 5 percent weight, which translated into a number needed to treat (NNT) of 8. Although weight outcomes were less well-reported beyond 12 months, weight loss remained significantly greater in intervention compared with control conditions in interventions lasting up to 36 months. Participants who received behavior-based weight loss maintenance interventions generally maintained more of their weight loss compared with those in control conditions. The heterogeneity in each individual intervention arm and differences in the populations, settings, and trial quality made it difficult to disentangle what variables might be driving larger effects.
In the two largest and longest good-quality trials (n=1818), participants randomized to behavior-based weight loss interventions had a decreased probability of developing type 2 diabetes compared with control conditions over 3 to 9 years. Although 11 smaller and generally shorter-duration weight loss trials did not find significant differences between groups, when pooled with the larger trials, there was a significant 33% reduction in risk of developing diabetes over 1 to 9 years (pooled risk ratio [RR], 0.67 [95% CI, 0.51 to 0.89]; k=9; n=3140; I2=49.2%). Three large trials (n=3916) noted benefits of behavior-based weight loss on hypertension and hyperlipidemia diagnosis and/or medication use; however, effects were not found in five smaller trials. Effects on metabolic syndrome and CVD risk score were mixed.
Participants randomized to weight loss medications had more weight loss and a greater decrease in waist circumference than those on placebo. Participants who received medications to assist with weight loss maintenance generally maintained more of their weight loss and waist circumference decrease compared with those in control conditions. However, the results were limited by high dropout rates and relatively short followup duration in some trials. The most common intermediate outcome reported (k=4; n=9763) was incident diabetes, and there was a decreased risk of developing diabetes over 1 to 4 years in those given medications; however, these trials were similarly limited by high dropout rates. Other intermediate outcomes were sparsely reported with mixed results.
Detailed Results
Behavior-Based Weight Loss Interventions
Weight Loss
All of the included trials reported treatment effects on at least one measure related to weight change (i.e., weight change in kilograms [kg] or pounds [lb], percent weight loss, BMI, waist circumference, or the proportion of participants losing 5%, 7%, 10%, or 15% of their weight from baseline). All weight-related outcomes for all time points and all arms for all trials are reported in Appendix G Table 1 for continuous outcomes and Appendix G Table 2 for dichotomous outcomes. Table 11 summarizes the results for all pooled analyses.
A meta-analysis combining the 67 behavior-based weight loss trials that reported kilograms or pounds lost at 12 to 18 months found a pooled mean difference of −2.4 kg (−5.3 lb) more lost in the intervention versus control groups (mean difference [MD], −2.39 kg [95% CI, −2.86 to −1.93]; k=67; n=22,065; I2=90.0%) (Figure 4). Although not all trials found statistically significant results, in all but two cases, intervention participants showed greater reductions in weight than control participants. Absolute changes in weight ranged from −0.5 kg (−1.1 lb) to −9.3 kg (−20.5 lb) among intervention participants and from 1.4 kg (3.1 lb) to −5.6 (−12.3 lb) among control participants at 12 to 18 months. Across the trials, however, a wide range of effects was seen within all arms (intervention and control) as demonstrated by large SDs relative to the average change. In other words, some adults showed fairly large reductions in weight, some showed no or modest changes, and some gained weight. All but nine221, 231, 243, 255, 264, 269, 272, 275, 318 of the trials that reported weight change at 12 to 18 months had interventions that spanned at least 12 months. Within the eight trials that had interventions less than 12 months long (i.e., 3 to 9 months), only one reported a statistically significant difference in weight loss at 12 months.221
Weight change at followup beyond 12 to 18 months was not as well reported. The pooled MD in weight change at 24 months was −1.45 kg (−3.2 lb) in favor of the intervention versus control groups [95% CI, −2.03 to −0.87]; k=21; n= 7268; I2=67.9%) (Figure 5). Absolute changes in weight ranged from a 1.0 kg (2.2 lb) to −5.6 kg (−12.3 lb) among intervention participants and from 0.3 kg (0.7 lb) to −4.0 kg (−8.8 lb) among control participants. Absolute differences between groups ranged from 0.75 kg in favor of the control group to −4.78 kg in favor of the intervention group. Only eight trials reported weight change at greater than 24 months, with most reporting outcomes at 2.5 to 4 years;225, 234, 254, 256, 261, 301, 306, 326 one reported effects of the intervention at both 2.5 and 6.6 years, over 4 years after the intervention ended234).
Twenty-eight trials reported effects of the interventions on weight change over time.206, 219, 224, 225, 234, 237, 242, 251, 254, 256, 258, 261, 266, 269, 271, 286, 288, 290, 291, 301, 302, 306, 314, 318, 323-326 Ten trials showed consistent although attenuated, statistically significant benefit of the interventions over time (from 12 to 48 months followup),219, 224, 258, 261, 266, 288, 301, 306, 323, 325 whereas 10 trials showed consistent null effects over time.206, 237, 251, 254, 256, 269, 271, 290, 318 Six trials reported initial statistically significant benefit of the interventions at 12 to 18 months, with attenuation of effects over time such that effects were no longer statistically significant at 18 to 80 months.234, 242, 286, 291, 314, 324 One trial326 reported a consistent (not attenuated) benefit from a 28-month intervention at 12, 18, and 30 months. One trial225 reported no benefit from the 3-year intervention at 12 and 24 months but found a statistically significant greater weight loss at 3 years. A forest plot showing all of the trials that reported weight change over time (i.e., more than one time point), without pooling, is included to visualize the change in effects over time within each trial (Figure 6). Within the 10 trials with a lag time between intervention end and final followup (lag of 2 to 50 months),234, 254, 261, 266, 269, 271, 286, 318, 323, 326 four reported statistically significant differences in weight loss at the final time point.261, 266, 323, 326
Nine trials that reported a weight outcome could not be included in the meta-analyses for weight change at 12 to 18 months or 24 months because of limitations in data reporting (e.g., no measure of dispersion) (Appendix G Table 1).214, 230, 254, 256, 257, 276, 278, 280, 295 Most of these were relatively small trials with sample sizes ranging from 50 to 280. Within all of these trials, intervention group participants experienced greater mean or median weight loss than control group participants, but only three trials reported these differences as statistically significant at 12 to 18 months.278, 280, 295
Separate meta-analyses for between-group mean differences in percent weight change and BMI at 12 to 18 months followup also showed statistically significant associations with weight loss interventions (Table 11).
There was no evidence of small-study effects for weight loss based on the Egger’s test.
Weight Loss of 5 Percent or Greater
Forty-five of the 80 trials reported the proportion of participants losing at least 5 percent of their baseline weight at 12 months or more followup (Appendix G Table 2). A meta-analysis of 38 trials reported that intervention participants had a 1.94 times greater probability of losing 5 percent of their initial weight compared with control groups over 12 to 18 months (RR, 1.94 [95% CI, 1.70 to 2.22], k=38; n=12,231, I2=67.2%) (Figure 7). Based on an assumed control risk of 14 percent, the NNT to achieve one more adult losing at least 5 percent of their body weight over 12 to 18 months is 8 (NNT, 7.6). At 24 months, the pooled RR was attenuated but still suggested an association between behavior-based weight loss interventions and the proportion of participants losing at least 5 percent of their baseline weight (pooled RR, 1.51 [95% CI, 1.25 to 1.81], k=13; n=4824, I2=63.0%) (Figure 8). There was no evidence of small-study effects for the proportion losing at least 5 percent of their body weight based on the Peters’ test.
Fewer trials reported the percent of participants losing 10 percent or more of their body weight. Meta-analyses found that intervention participants were 3.1 times more likely to lose 10 percent of their weight compared with controls at 12 to 18 months (RR, 3.06 [95% CI, 2.41 to 3.88]; k=16; n=6975; I2=49.0%) (Figure 9). In the nine trials reporting this effect at 24 months or greater, the effects were attenuated over time; however, six trials still had statistically significant greater probability of 10 percent weight loss in intervention compared with controls, with RRs ranging from 1.6 to 3.8 (Appendix G Table 2).
Waist Circumference
A meta-analysis of 41 trials reported a mean greater reduction of approximately 2.51 cm (1.0 in) in waist circumference among those in behavior-based weight loss interventions compared with control conditions at 12 to 18 months followup (95% CI, −3.15 to −1.87; k=41; n=12,180; I2=94.6%) (Table 11). Absolute changes in waist circumference ranged from 0.1 cm to −11.3 cm among intervention participants and from 1.5 cm to −7.4 cm among control participants. Fewer trials reported the effects of the intervention on other adiposity outcomes such as waist-to-hip ratio and percent body fat; results related to these outcomes are presented in Appendix G Table 1.
Incident Type 2 Diabetes
Thirteen trials (n=4095) reported incident type 2 diabetes associated with behavior-based weight loss interventions (Table 12).205, 215, 225, 258, 265, 266, 277, 280, 283, 288, 306, 314, 321 Twelve of the 13 trials were limited to adults with prediabetes or those who were otherwise at risk for diabetes (family history, history of gestational diabetes, metabolic syndrome); the one remaining trial was conducted among breast cancer survivors.288 Most of the trials reported cases of diabetes over 1 year of followup; only five trials reported type 2 diabetes incidence at 2 or more years. In DPP (n=1295), the estimated cumulative incidence of diabetes at 3 years was 14.4 versus 28.9 percent in the lifestyle-intervention versus placebo groups, respectively (between-group crude incidence difference of −58% [95% CI, 48 to 66]; study-reported NNT, 6.8).205 Similarly, the good-quality Finnish DPS (n=523), a 4-year behavior-based weight loss intervention trial,306, 340 found that after 9 years, intervention group participants were significantly less likely to develop type 2 diabetes compared with the control group (40.0% vs. 54.5%, respectively; HR, 0.4 [95% CI, 0.3 to 0.7]).306, 340 The European Diabetes Prevention Study (EDIPS) (n=102) applied the DPS intervention in the United Kingdom and found a large but nonsignificant reduction in the incidence of diabetes in the intervention group compared with the control group after 5 years (9.8% vs. 21.6%, respectively; RR, 0.45 [95% CI, 0.2 to 1.2]).283 In the remaining 10 trials, progression to diabetes was observed less frequently with absolute cumulative incidence of diabetes at up to 3 years followup ranging from 0 to 15.0 percent in intervention participants and 0 to 28.9 percent among control participants. Although the differences between intervention and control groups were not statistically significant, the studies were generally of shorter duration and smaller than DPP and FDPS.215, 225, 258, 265, 266, 277, 280, 288, 314, 321 When the two larger and seven of the smaller trials that reported rates of incident diabetes were pooled, there was a significant 33 percent reduction in risk of developing diabetes over 1 to 9 years (pooled RR, 0.67 [95% CI, 0.51 to 0.89]; k=9; n=3140; I2=49.2%) (Figure 10).
Other Intermediate Outcomes
Other intermediate outcomes, including the prevalence of hypertension, use of CVD medications, prevalence of metabolic syndrome, and estimated 10-year risk of CVD were sparsely reported within the trials. Rates of hypertension at 18 months to 3 years of followup were reported for the TOHP Phase I (n=564) and Phase II (n=1191) trials as well as the DPP trial (n=2161) and a smaller study by Nilsen et al (n=213).301, 327, 333, 336 TOHP I and II reported 34 and 22 percent reduced risk of incident hypertension at 18 months among those in the weight loss condition (which also included sodium reduction) compared with the control condition, respectively.333, 336 By 3 years in TOHP II, fewer participants in the intervention group (32%) met criteria for hypertension compared with the control group (39%) (absolute risk difference [RD], 7.3 [NNT=14]). In DPP (n=2161), the prevalence of hypertension remained stable among intervention participants (approximately 30%) but increased among control participants (from approximately 30% to 40%) over 3 years (p<0.001).336 Similarly, use of antihypertensive medications rose from 17 to 23 percent among DPP intervention participants and from 17 to 31 percent among control participants over 3 years (p<0.001). Likewise, fewer weight loss participants (12%) required drug therapy for either elevated triglyceride or low-density lipoprotein cholesterol levels compared with control participants (16%) (p<0.001).205, 336 A smaller study by Nilsen et al (n=213) found no significant difference between groups in the percent of individuals with hypertension by the end of the study; however, there was a high baseline prevalence of hypertension (74%).327 Four smaller trials examining medication changes (n=30 to 772) did not find significant differences in antihypertensive or lipid-lowering medication use between intervention and control arms.232, 253, 288, 291 Five trials (n=3356) reported on incidence of metabolic syndrome in intervention and control arms at 1 to 3 years followup with mixed results.205, 243, 265, 286, 291 Similarly, two trials (n=165) reported mixed findings on the effects of weight loss interventions on estimated 10-year CVD risk at 1 year based on the U.K. Prospective Diabetes Study risk engine or QRISK2.214, 243
Subpopulations
Subpopulation analyses were infrequently reported among included studies and often not prespecified. Even when prespecified analyses were performed, they often lacked interaction testing, limiting the allowable interpretation of treatment effect by subpopulation.
The differential effects of weight loss interventions for individuals with varying baseline BMIs was examined in five trials,234, 266, 288, 301, 302 only two of which266, 301 prespecified such subgroup analyses. No trial found that baseline weight was associated with weight change following interaction testing.
Prespecified analyses of the effect of age were reported in two studies with mixed results. In the CITY trial among young adults (mean age, 29.4 years), a cell-phone based intervention, the oldest tertile of participants (mean age not reported) lost less weight than the youngest tertile of participants (mean age not reported).302 However, in DPP there was a suggestion of a stronger effect of the lifestyle intervention in older individuals (ages 60 to 85 years); however, there was no interaction testing, limiting interpretation of this finding.341
Whether sex influenced the effectiveness of weight loss interventions was reported in eight trials, with six prespecifying interaction testing analyses. Men were generally observed to lose a greater percentage of their baseline weight than women; however, only two301, 342 of six studies found the sex differences to be significant in interaction testing.254, 266, 300, 302 Two exploratory analyses255, 279 also had mixed results, with one trial reporting greater weight loss in men following interaction testing.279
The effect of race/ethnicity on the effectiveness of weight loss interventions was examined in seven trials; six of these analyses were prespecified.215, 300-302, 326, 342 There was a trend toward greater weight loss among white participants than black or Hispanic participants. However, this finding became nonsignificant in three215, 300, 302 of the five trials following interaction testing. The two trials that found a significant racial/ethnic difference were TOHP II and DPP. In TOPH II, white participants lost a net 1.8 kg more than African American participants at 18 months.301 Within DPP, black women exhibited significantly smaller (approximately half) weight losses (p<0.01) with the lifestyle intervention than other race-sex groups.342 One additional trial (TONE) found significantly greater weight loss in white participants than black participants; however, no interaction testing was performed.326, 343 One exploratory analysis among a predominantly non-Hispanic white female population found no difference by race/ethnicity.288
Subgroup analyses for all other outcomes were limited by sparse reporting and limited interaction testing.
Effect Modification
We conducted subgroup analyses and a series of meta-regressions to explore potential effect modification by prespecified study, population, and intervention characteristics (see Appendix B for the full list of variables). We limited these analyses to the main outcome of change in weight at 12 to 18 months followup, and all meta-regressions controlled for risk status of the population.
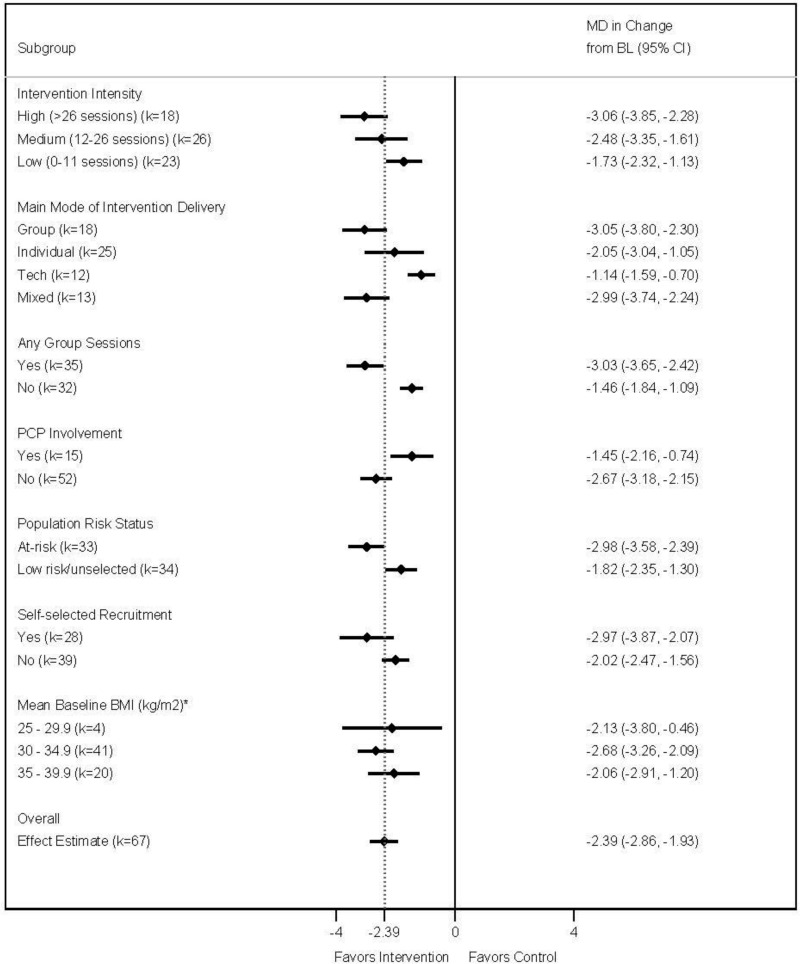
In terms of intervention characteristics, subgroup analyses according to the number of intervention sessions in the first year (>26 sessions, 12–26 sessions, and <12 sessions) showed slightly higher effect estimates among interventions with more sessions; however, the confidence intervals among all three of the subgroups overlapped (Figure 11). When examined as a continuous measure, a higher number of intervention sessions in the first 12 months was associated with significantly more weight loss (coefficient, −0.03; p=0.023); however, total number of contacts (including text messages, emails, and print materials) was not (coefficient, 0.001; p=0.488). Likewise, the number of sessions in the first 12 months was not associated with greater weight loss after controlling for the presence of any group sessions (coefficient, −0.015; p=0.212). In addition, there was no pattern of effects according to the main mode of intervention delivery (i.e., group vs. individual vs. technology-based vs. mixed) (Figure 11). However, there was evidence of a greater effect among interventions that included any group sessions versus those that did not (coefficient, −1.19; p=0.004). This held true after controlling for the total number of sessions within the first year and the risk status of the population (coefficient, −0.97; p=0.029). Among the subset of trials that included any group sessions (whether or not it was the main mode of delivery), the pooled difference in weight change was −3.03 kg (95% CI, −3.65 to −2.42; k=35; n=15,132; I2=91.3%). Those without any group sessions resulted in a smaller pooled effect estimate (although still statistically significant) and reduced statistical heterogeneity (MD, −1.46 kg [95% CI, −1.84 to −1.09]; k=32; n=6933; I2=49.8%). None of the other intervention characteristics we looked at modified the effect of the intervention, including duration of the intervention, whether there was in-person support, whether individual in-person or telephone sessions were offered, whether the intervention was technology-based, whether self-monitoring of weight or behaviors was encouraged, or whether the intervention was based on the DPP. Descriptions of each intervention, including specific intervention components, are fully described in Table 4, Table 5, and Appendix F Table 1.
In terms of population characteristics, larger differences in weight change were seen among trials that specifically enrolled adults with increased cardiovascular risk, subclinical risk, and elevated cancer risk versus those who were unselected or generally at low risk (coefficient, −1.15; p=0.004). A meta-analysis of the subset of 33 trials among participants at elevated risk found a pooled MD in change of −2.98 kg (95% CI, −3.58 to −2.39; k=33; n=10,554; I2=87.7%) at 12 to 18 months (Figure 11). A statistically significant association was also found for the subset of trials among low risk or unselected participants but with a significantly smaller effect estimate than that seen for those at risk (MD, −1.82 kg (95% CI, −2.35 to −1.30; k=34; n=11,511; I2=82.8%). Those who self-selected or volunteered to take part in the interventions were also more likely to experience greater weight loss (MD, −2.97 kg (95% CI, −3.87 to −2.07; k=28; n=9626; I2=94.0%) than participants who were recruited directly into the trial (MD, −2.02 kg (95% CI, −2.47 to −1.56; k=39; n=12,439; I2=79.7%) (coefficient, −1.14; p=0.004), after controlling for risk status. Baseline BMI and baseline weight category (i.e., overweight, Class I obesity, and Class II obesity) were not associated with differences in the effects of the intervention on weight change, percent weight change, or the proportion of participants losing at least 5 percent of their baseline weight.
There was no evidence of effect modification by study quality or U.S.- versus non-U.S.-based studies. Sample retention at 12 months was associated with the pooled effect size in that trials with higher retention rates experiencing greater weight loss (coefficient, −0.05; p=0.011).
In summary, a few factors were identified in the subgroup analyses and meta-regressions as potential effect modifiers. However, the heterogeneity in each individual intervention arm, confounded with differences in the populations, settings, and trial quality, make it nearly impossible to disentangle what variables may be driving larger effects. The consistency—yet wide range in effects—seen across specific interventions and across various adult subgroups emphasizes a broad range of benefit that is likely dependent on other individual, social, and environmental factors influencing an individual’s weight loss.
Behavior-Based Weight Loss Maintenance Interventions
Maintenance of Previous Weight Loss
All weight-related outcomes for all time points for the nine behavior-based weight loss maintenance trials are reported in Appendix G Table 3 for continuous outcomes and Appendix G Table 4 for dichotomous outcomes.
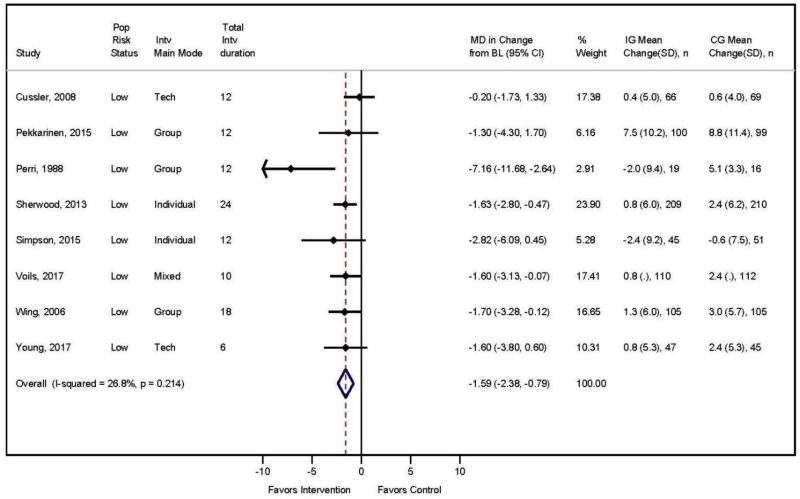
Six trials included an initial weight loss intervention (mean weight loss of 5 to 15 kg [11 to 33.1 lb]) for all study participants (Appendix F Table 2).233, 282, 284, 303, 309, 317 Three additional trials did not include a weight loss portion but required that participants have recently lost 5296 or 10294, 313 percent of their body weight. In eight trials, both the intervention and control arms regained weight over a 12- to 18-month followup; however, the intervention arm experienced less weight regain (gain of 0.1 kg [0.2 lb] to 7.5 kg [16.5 lb] in intervention arms and 0.6 kg [1.3 lb] to 8.8 kg [19.4 lb] in control arms), although all participants maintained some of their previous weight loss.233, 282, 284, 294, 303, 309, 313, 317 Only four of the eight trials had statistically significant results. In the ninth trial both the intervention and control arms continued to lose weight (loss of 2.4 kg [5.3 lb] in intervention and 0.6 [1.3 lb] in controls); however these within-group changes were not statistically significant.296 A meta-analysis combining the eight behavior-based weight loss trials that reported kilograms or pounds lost at 12 to 18 months found a pooled mean difference of −1.6 kg (−3.5 lb) in the intervention versus control groups (MD, −1.59 kg [95% CI, −2.38 to −0.79]; k=8; n=1408; I2=26.8%) (Figure 12). The one trial that could not be included in the meta-analysis had similar results.303 Three studies included participant followup beyond 18 months with mixed findings.294, 303, 317
Maintenance of 5 Percent or Greater Weight Loss
Only three of the maintenance trials (n=1320) examined maintenance of 5 percent weight loss over 12 to 36 months, finding mixed results. In two small trials (n=92 and 200), those randomized to a maintenance intervention were not more likely to have maintained 5 percent weight loss by 12 to 36 months.282, 317 However, in the larger trial (n=1029), those in the maintenance group were slightly more likely to have maintained 5 percent of their weight loss at 30 months (42% vs. 34%; RR, 1.24 [95% CI, 1.02 to 1.51]) and 60 months (37% vs. 27%; RR, 1.37 [95% CI, 1.03 to 1.82]) compared with the minimal intervention arm.303
Waist Circumference
Three small trials (n=453) reported change in waist circumference after behavior-based maintenance interventions.296, 309, 317 Changes in waist circumference were not significantly different between intervention and control groups at 12 months. Extension of one trial for 36 months did not reveal any significant differences in waist circumference over the longer-term followup.317
Incident Diabetes and Other Intermediate Outcomes
No study reported these outcomes.
Medication-Based Weight Loss Interventions
All weight-related outcomes for all time points for all medication-based weight loss trials are reported in Appendix G Table 5 for continuous outcomes and Appendix G Table 6 for dichotomous outcomes. Findings were often limited by reduced long-term followup, with the majority of trials reporting 30 percent or greater loss to followup or greater by 12 to 13 months (Figure 13), and limited data reporting (often not reporting statistical significance of findings and lack of description of variance) (Table 2). The study-specific results below and in tables reflect analyses using an mITT analysis (i.e., participants’ last observation postbaseline while still on study drug) as that was the primary analysis reported by studies (mITT is required by the FDA). Results from sensitivity analyses within trials using other data substitution methods (baseline observation carried forward, multiple imputation using mixed effects models) were generally consistent with the mITT results.
Weight Loss
Liraglutide. Two trials reported on degree of weight loss in liraglutide versus placebo arms (n=3853).220, 285 Those in the liraglutide groups lost statistically more weight (−7.8 to −8.4 kg [−17.2 to −18.5 lb]) than those in placebo group (−2.0 to −2.8 kg [−4.4 to −6.2 lb]) over 12 to 13 months, a statistically significant difference (p<0.001) (Table 13). One trial extended followup in those with prediabetes to 36 months; mean weight loss was less by 36 months in both groups, but the mean difference in weight loss between arms was still statistically different (liraglutide arm lost 4.6 kg more than placebo at 36 months; p<0.0001).339
Lorcaserin. Two trials reported on degree of weight loss in lorcaserin versus placebo arms using mean or least square mean (LSM) (n=6139) (Table 13).172, 173 Those randomized to lorcaserin lost a mean or LSM of 5.8 kg (12.8 lb), while those in placebo lost 2.2 to 2.9 kg (4.9 to 6.4 lb) over 12 months, which was statistically significantly different in both trials (p<0.001).
Naltrexone and bupropion. Three trials reported on degree of weight loss in naltrexone and bupropion compared with placebo arms (Table 13).218, 244, 311 Those randomized to naltrexone and bupropion lost more weight over 13 months compared with those randomized to placebo (LSM, −6.1 to −6.2 kg [−13.4 to −13.7 lb] and −1.3 to −1.4 kg [−2.9 to −3.1 lb] in the intervention and placebo groups, respectively; p<0.001).218, 244 One trial reported only the percent change in weight, with those in the naltrexone and bupropion arm showing greater percent weight loss than the placebo arm (LSM, −9.1% vs. −5.1%, respectively; p<0.001) (Appendix G Table 5).311
Orlistat. Eleven trials reported on degree of weight loss in orlistat versus placebo arms.160, 161, 227, 236, 239, 246, 260, 263, 292, 297, 304 In every trial, those randomized to orlistat lost statistically significantly more weight loss (mean of 1.0 to 4.4 kg [2.2 to 9.7 lb] more) than those on placebo over 12 months. (Table 13).161, 260, 297 In the two trials that compared the 60 mg TID dosage to 120 mg TID, weight loss was about 0.8 to 0.9 kg less with 60 mg TID compared with 120 mg TID over 12 months.246, 292 Two studies examined weight loss at later time points (18 to 48 months). Mean weight loss was less in both arms at the later time points (1.2 to 2 kg had been regained); however, those in the orlistat arm had still lost more weight since randomization compared with the placebo arm (mean difference, −3.1 to −3.37 kg in 120 mg TID of orlistat and −2.3 to −2.81 kg in 60 mg TID of orlistat vs. placebo arms, respectively; p<0.01).246, 292 Following 4 years of treatment, participants had regained approximately half of their weight loss since randomization; however, the 120 mg orlistat arm still had lost significantly more weight than the placebo arm (p<0.001).161
Phentermine and topiramate. Two trials reported on degree of weight loss for those randomized to phentermine and topiramate versus placebo arms.216, 241 In one trial, participants randomized to phentermine and topiramate lost statistically significantly more weight than those on placebo (LSM, −8.1 kg [−17.8 lb] with 15/92 mg, −10.2 kg [−22.5 lb] with 7.5/46 mg, and −1.4 kg [−3.1 lb] with placebo; p<0.0001) (Table 13).241 The second trial only reported the percentage of weight loss in the two arms. Those randomized to phentermine and topiramate lost a greater percentage of weight compared with the placebo arm at 12 months (LSM, 10.9% vs. 1.5%, respectively; p<0.0001) (Appendix G Table 5).216
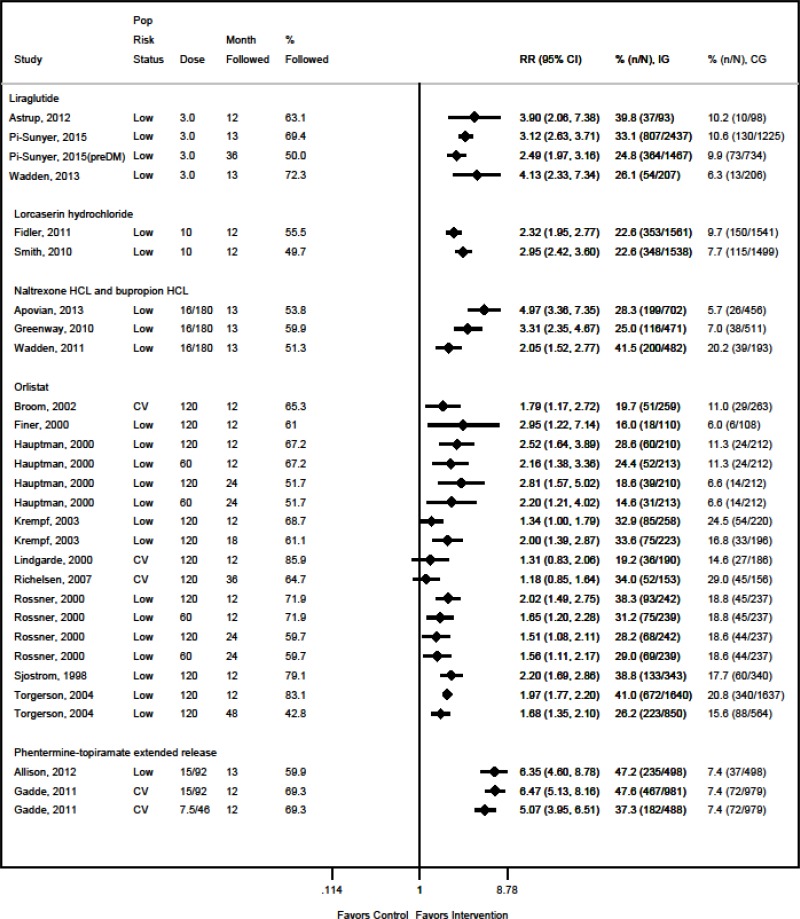
Weight Loss of 5 Percent or Greater
Liraglutide. At 12 to 13 months, participants randomized to liraglutide were 2.8 to 4.8 times more likely to lose 5 percent of their body weight compared with those in the placebo arm (63% to 79% compared with 27% to 29%, respectively) and 3.9 to 4.3 times more likely to lose 10 percent of their weight (33% to 40% compared with 10% to 11%, respectively) (p<0.001) (Figure 13, Figure 14).220, 285 In additional followup of a subgroup with prediabetes at baseline, those randomized to orlistat were over 3 times more likely to have achieved 5 and 10 percent weight loss after 36 months compared with those on placebo (p-values<0.001), although absolute percentages who reached this milestone was smaller in both arms.339
Lorcaserin. Compared with placebo, those randomized to lorcaserin were 1.9 to 2.3 times more likely to lose 5 percent of their body weight (47% vs. 20%–25% in lorcaserin and placebo arms respectively; p<0.001) (Figure 13) and 2.3 to 2.9 times more likely to lose 10 percent of their weight by 12 months (23% vs. 8%–10% in in lorcaserin and placebo arms, respectively; p<0.001) (Figure 14).
Naltrexone and bupropion. Those randomized to naltrexone and bupropion were 1.6 to 3.0 times more likely to lose 5 percent of their weight (48%–66% in naltrexone and bupropion arm vs. 16%–42% in placebo arm; p<0.01)218, 244, 311 (Figure 13) and 2.0 to 5.0 times more likely to lose 10 percent of their weight (25%–42% in naltrexone and bupropion arm compared with 6%–20% in placebo arm; p<0.001) (Figure 14).
Orlistat. Ten trials reported the percentage of participants who lost at least 5 and 10 percent of their baseline weight.160, 161, 227, 239, 246, 260, 263, 287, 292, 297 Participants randomized to orlistat were 1.3 to 2.3 times more likely to lose 5 percent of their weight at 12 months compared with those given placebo (35%–73% vs. 21%–49%, respectively; p<0.05) (Figure 13).160, 161, 227, 239, 246, 260, 263, 287, 292, 297 In the two trials that examined both orlistat dosages (60 TID and 120 TID), there was little evidence of a dosage effect.246, 292 In the four trials that extended followup beyond 12 months,161, 246, 260, 292 those on either dose of orlistat were still significantly more likely to be 5 percent below their starting weight at 24 to 48 months (RR, 1.41 to 1.74; p<0.05). Nine of these 10 trials also reported 10 percent weight loss;161, 227, 239, 246, 260, 263, 287, 292, 297 the results were similar with those on either dosage of orlistat being more likely to have 10 percent weight loss at 12 to 48 months (RR, 1.31 to 2.95; p<0.05 in all but one study263) (Figure 14); however, the absolute percentage of participants who reached this milestone was smaller in both arms, with rates decreasing as followup time increased.161, 227, 239, 246, 260, 263, 292, 297
Phentermine and topiramate. Those randomized to 15/92 mg or 7.5/46 mg phentermine and topiramate were 3.0 to 3.9 times more likely to lose 5 percent of their weight, respectively, by 12 to 13 months (67% to 70% of 15/92 mg, 62% of 7.5/46 mg, and 17% to 21% of placebo; p<0.0001) (Figure 13). They were 5.1 to 6.4 times more likely to lose 10 percent of their body weight (47% to 48% of 15/92 mg, 37% of 7.5/46 mg, and 7% of placebo); p<0.0001) (Figure 14).216, 241
Waist Circumference
Liraglutide. Participants randomized to liraglutide had significantly greater mean waist circumference decreases than placebo (means, 7.8 to 8.2 cm over 12 to 13 months compared with 3.0 to 3.9 cm in the placebo arm; p<0.001) (Table 14). Among participants with prediabetes at baseline, the change was slightly attenuated by 36 months; however, those randomized to liraglutide still had a statistically significant greater 3.5-cm decrease in waist circumference.339
Lorcaserin. Waist circumference decreased more in those randomized to lorcaserin compared with those randomized to placebo by 12 months (LSM/means, −6.3 to −6.8 cm vs. −3.9 to −4.1 cm, respectively; p<0.001) (Table 14).172, 173
Naltrexone and bupropion. Waist circumference decreased more in those randomized to naltrexone and bupropion compared with those in placebo over 12 months (LSM/means, −6.2 to −10.2 cm vs. −2.1 to −7.0, respectively; p<0.001) (Table 14).218, 244, 311
Orlistat. There was a greater decrease in waist circumference in the orlistat arms over 12 to 18 months compared with placebo (LSM/means, −3 to −9.6 cm vs. −1.9 to −7.0 cm) (Table 14).161, 227, 236, 260, 263, 292, 304 Statistical significance was reported in only six of the seven trials, with four showing a statistically significance difference between arms. In the one study that examined both 60 mg TID and 120 TID dosages, there was no evidence of a dosage effect.292 By 24 and 48 months, there was regain in waist circumference in both arms, but the statistically significant differences remained except for one 60 mg TID arm.161, 292
Phentermine and topiramate. Over 12 to 13 months, waist circumference decreased significantly more for participants randomized to phentermine-topiramate 15/92 mg compared with placebo (LSM, −9.2 to −10.9 vs. −2.4 to −3.1 cm, respectively; p<0.0001). This effect was also significant in participants randomized to 7.5/46 mg (LSM, −7.6 vs. −2.4 cm, respectively; p<0.0001) (Table 14).216, 241
Incident Diabetes
Liraglutide. In the single liraglutide trial examining incident diabetes (n=3662), fewer participants randomized to liraglutide (n=4 [0.2%]) developed diabetes over 13 months compared with those given placebo (n=14 [1.1%]) (odds ratio [OR], 8.1 [95% CI, 2.6 to 25.3]; p<0.001) (Table 15).285 The trial continued past 13 months among 2210 participants with prediabetes at baseline; participants randomized to liraglutide were less likely to develop type 2 diabetes by 36 months compared with placebo (1.8% vs. 6.2% of participants), with a mean time from randomization to diagnosis of 99 (SD, 47) versus 87 (SD, 47) weeks, respectively (HR, 0.21 [95% CI, 0.13 to 0.34; p<0.0001]). However, these findings are limited by the large number of participants who discontinued medication during the 36-month followup (53% of those on liraglutide and 45% of those on placebo completed the study on medication).339
Lorcaserin. No study reported this outcome.
Naltrexone and bupropion. No study reported this outcome.
Orlistat. A trial of over 3300 persons (21% with prediabetes) found that 6 percent of those randomized to 120 mg TID of orlistat developed type 2 diabetes over 48 months compared with 9 percent of those in the placebo arm (HR, 0.63 [95% CI, 0.46 to 0.87]; p=0.005). However, applicability of these findings is limited by the high discontinuation rate (only 52% and 35% of intervention and placebo participants, respectively, completed a 48-month followup on study medication).161
Phentermine and topiramate. One trial of over 2400 participants with elevated cardiovascular risk (68% with prediabetes) reported that 14 (1.7%) and 12 (2.8%) of those randomized to 15/92 mg and 7.5/46 mg of phentermine and topiramate, respectively, developed type 2 diabetes compared with 30 (3.6%) of those on placebo (RR, 0.47 [95% CI, 0.25 to 0.88] and 0.78 [95% CI, 0.40 to 1.50] for 15/92 mg and 7.5/46 mg arms, respectively) (Table 15).241
Other Intermediate Outcomes
Liraglutide. Compared with placebo at 13 months, those randomized to liraglutide in one trial (n=3662) were less likely to increase use of lipid-lowering medication (2.1% vs. 3.7%) and antihypertensive medication (3.7% vs. 5.7%) and were more likely to decrease use of antihypertensives (6.0% vs. 3.8%), but statistical significance was not reported.285
A second, smaller trial (n=191), in which there was a high prevalence of metabolic syndrome at baseline (42% and 51% in liraglutide and placebo arms, respectively), reported that those randomized to liraglutide had a statistically significant lower prevalence of metabolic syndrome compared with placebo at 12 months of followup (17% vs. 43%; p=0.005).220
Lorcaserin. In one 12-month trial (n=3102),173 4.0 and 5.0 percent of those randomized to lorcaserin and placebo arms, respectively, increased use of lipid-lowering medications and 2.6 and 1.4 percent decreased use. Use of antihypertensive medications decreased in 4.0 and 3.1 percent of participants randomized to lorcaserin and placebo, respectively. However, the number taking these classes of medications at baseline was not given, and statistical significance was not reported.
Naltrexone and bupropion. No study reported other intermediate outcomes.
Orlistat. One trial reported that over 12 months there was no significant difference between change in 10-year CVD risk score and usage of cardiovascular medications in those randomized to 120 mg TID of orlistat compared with placebo.304
Phentermine and topiramate. No study reported other outcomes.
Medication-Based Weight Loss Maintenance Interventions
All weight-related outcomes for all time points for all medication-based weight loss trials are reported in Appendix G Table 7 for continuous outcomes and Appendix G Table 8 for dichotomous outcomes.
Maintenance of Previous Weight Loss
Liraglutide. One trial (n=413) examined weight loss maintenance with liraglutide after a run in weight loss period in which qualifying participants were required to lose 5 percent of their body weight (mean weight loss, 6.3 kg [13.9 lb]) through a hypocaloric diet.312 During the 13-month maintenance phase, those in the placebo arm lost an additional 0.1 kg (0.2 lb), while those randomized to liraglutide lost an additional 6.0 kg (13.3 lb) (p<0.0001).
Orlistat. In the two trials247, 287 examining the use of orlistat for weight loss maintenance, participants had lost an average of 9.9 to 12.0 kg (21.8 to 26.5 lb) through hypocaloric diets prior to being randomized into the weight loss maintenance phase. Those randomized to 120 mg TID of orlistat gained 1.8 to 1.9 kg (4.0 to 4.2 lb) less than those given placebo over 12 to 18 months (2.6–2.8 vs. 4.4–4.7 kg, respectively, a statistically significant difference in the one study reporting statistical results247). In the one trial with both 120 mg TID and 60 mg TID arms, the 60 mg TID arm did not have significantly less weight gain than those in the placebo group over 12 months (3.8 vs. 4.4 kg gain, respectively).247 During longer-term followup in one trial of 120 mg TID, those randomized to orlistat continued to have less weight gain by 36 months compared with placebo (5.1 vs. 7.1 kg; p=0.028).287
Maintenance of Weight Loss of 5 Percent or Greater
Liraglutide. In the one maintenance trial,312 all participants had experienced at least 5 percent weight loss on entry. Compared with placebo participants, those on liraglutide were 2.3 times more likely to have maintained 5 percent weight loss (RR, 2.32 [95% CI, 1.74 to 3.11]) and 4.1 times more likely to have achieved 10 percent weight loss (RR, 4.13 [95% CI, 2.33 to 7.34]) at the end of the 12-month weight loss maintenance period (p<0.0001) (Figure 13).
Orlistat. In the one maintenance trial reporting percent weight loss, all participants had lost at least 5 percent of their weight at study entry (Figure 13, Figure 14).287 After 12 months of maintenance treatment, those randomized to orlistat 120 mg TID were 1.2 times more likely to have maintained their 5 percent weight loss (RR, 1.18 [95% CI, 1.05 to 1.33]; p<0.001), and this difference remained by 36 months (RR, 1.20 [95% CI, 1.00 to 1.43]; p<0.05). However, the percentage with 10 percent weight loss at 36 months was not statistically different between arms (RR, 1.18 [95% CI, 0.85 to 1.64]; p=NS).
Maintenance of Waist Circumference Decrease
Liraglutide. While both arms had continued decreases in waist circumference during the 13-month maintenance trial, the decrease was greater among those randomized to liraglutide (−4.7 vs. −1.2 cm; p<0.0001).312
Orlistat. In the one trial reporting waist circumference, those randomized to 120 TID of orlistat had no increase in waist circumference at 18 months, while the placebo group experienced an average 3 cm increase (p=NR).287 By 36 months, those randomized to orlistat had an average 4.3 cm increase in waist circumference, which was less than the 6.6-cm gain reported in the placebo arm (p=0.032).
Incident Diabetes
Liraglutide. No study reported this outcome.
Orlistat. One trial of 309 participants with at least one cardiovascular risk factor (27% with prediabetes) reported that compared with those randomized to 120 mg of orlistat, almost twice as many persons on placebo developed type 2 diabetes over the 36-month weight loss maintenance intervention (5.2% vs. 10.9%; p=0.041) (Table 15).287
Other Intermediate Outcomes
No study reported other intermediate outcomes.
KQ3. What Are the Adverse Effects of Primary Care–Relevant Behavioral and/or Pharmacotherapy Weight Loss and Weight Loss Maintenance Interventions in Adults Who Are Overweight or Have Obesity and Are a Candidate for Weight Loss Interventions?
Summary of Results
Rates of adverse events were sparsely reported in the behavior-based weight loss and weight loss maintenance trials (30 trials; n=12,824). In general, there were no serious harms related to the interventions and most trials noted no differences between groups in the rates of adverse events, including cardiovascular events. In the three trials large enough to examine musculoskeletal issues between groups, results were mixed.
Almost all medication trials reported adverse events. Weight loss medications were associated with more adverse events than placebo, which resulted in higher dropout rates due to adverse events in the medication than placebo arms. However, serious adverse events were not generally more common in those randomized to medications. There are multiple potential harms required by the FDA to be listed on weight loss medication labels, but these harms have not been well evaluated in the trials included in this review.
Detailed Results
Behavior-Based Weight Loss Interventions
Twenty-seven trials reported harms (or lack of harms) associated with a behavior-based weight loss intervention (n=12,235).205, 206, 215, 217, 219, 224, 225, 235, 237, 242, 249, 251, 253, 258, 264, 266, 278, 289-291, 305, 320, 321, 323, 325, 328, 330 We rated 15 of these trials as good quality and 12 as fair quality. Only two of these trials (DPP205 and SLIM325) were included in the previous review; the remaining 25 are new as part of this update. Very few trials reported their methods for capturing adverse events or provided definitions for adverse events or for serious adverse events.
Within the 27 trials, eight stated that no harms or serious adverse events were reported217, 251, 253, 264, 278, 321, 325, 328 and three simply stated that none of the adverse events that were reported were related to the study.290, 305, 323 Within the remaining 16 trials that reported actual data, the rates of any adverse event and serious adverse events were relatively low (ranging from 0.6% to 25% of participants experiencing any adverse event) and often not reported by group. In all but two trials,205, 291 rates of any adverse event, serious adverse events, and specific adverse events did not differ between the intervention versus control participants based on statistical testing or in comparing event rates. Those that did show differences between intervention and control groups are discussed below. Four trials specifically reported that no deaths occurred during the trial period.205, 206, 219, 290
Among four trials reporting specifically on cardiovascular-related adverse events or symptoms (e.g., chest pain, difficulty breathing, and fainting and dizziness),206, 215, 224, 291 three of the four reported low rates of self-reported cardiovascular events (<1%)215, 224 and cardiac disorders (10 cases of angina pectoris, atrial fibrillation, atrial flutter, or syncope among the intervention group and 6 cases of angina pectoris, atrial fibrillation, congestive heart failure, and myocardial infarction among the control group)206 and no differences between groups.215, 224 In the remaining trial among sedentary adults (categorized as low risk, as no data given on baseline comorbidities) (n=490), cardiovascular symptoms (including chest pain, difficulty breathing, and dizziness or loss of consciousness) were less common in the intervention group (115 events among 249 participants [46.2%]) compared with the usual care group (137 events among 241 participants [56.8%]), as were cardiovascular symptoms resulting in physician visits (30.5% vs. 34.4%) or hospitalizations (3.6% vs. 7.5%).291
The adverse events most commonly rated as being related to the intervention were musculoskeletal issues, which varied in severity from soreness to sprains to ruptured tendons.205, 206, 215, 224, 235, 237, 291, 330 Rates of musculoskeletal issues ranged from one musculoskeletal injury (0.006 event rate) to nearly 50 percent of participants experiencing muscle or joint aches. Within the seven trials specifically reporting event rates by group, only three had enough events to make comparisons between groups.205, 215, 291 In the DPP trial (n=2161), a statistically significant higher rate of musculoskeletal symptoms (myalgia, arthritis, arthralgia) was seen among those in the lifestyle intervention group (24.1 events per 100 person-years) compared with those in the control group (21.1 events per 100 person-years) (p<0.0167) over 4 years of followup.205 In the PROACTIVE trial (n=490), rates of musculoskeletal events during or after exercise (pain or cramping in leg, knee, or foot; strained muscle, tendon, or ligament; and broken bone) were slightly higher in the usual care group (311 events among 241 participants [129.0%]) compared with the intervention group (300 events among 249 participants [120.5%]) over the course of the 2-year intervention; musculoskeletal events requiring a physician visit were slightly higher in the intervention (70.3%) versus control (66.4%) participants.291 However, in DEPLOY (n=509),215 intervention participants did not experience more muscle or joint aches (48.6% vs. 50.5%; p=NR) or joint sprains or strains (22.6% vs. 22.9%; p=NR) compared with controls.
Six trials (n=2767) reported on incidence of gallbladder disease, which is more common among those who are overweight and have obesity and is associated with rapid weight loss.206, 224, 242, 249, 289, 320 Across these trials, 6 intervention versus 2 control participants experienced either gallstones or cholecystectomy over 1 to 2 years of followup.
One trial of postpartum women showed higher (38% to 42%) rates of reduced breast milk supply; however, these differences were not significant.330
Behavior-Based Weight Loss Maintenance Interventions
Three of the nine behavior-based weight loss maintenance interventions reported harms (n=589).282, 296, 309 In one trial (n=201), a similar number of participants (31%) in the intervention and control group were treated for adverse events over 24 months.282 In a second trial (n=222), there was one (0.1%) death in the control group and four (3.6%) adverse events (knee pain, low blood pressure, bradycardia, and anxiety) in the intervention group over 56 weeks; of note, the intervention group had more contacts at which to report adverse events compared with controls.309 The third trial (n=166) reported one serious adverse event (group not given) that was felt to be related to a pre-existing condition and not to the intervention.296
Medication-Based Weight Loss Interventions
Liraglutide
Three trials reported harms (or lack of harms) related to liraglutide (n=3990).220, 259, 285 Compared with placebo, those randomized to liraglutide had a higher prevalence of experiencing at least one adverse event (Table 16) (80%–96% vs. 63%–89%) and slightly more serious adverse events (Table 17) (6%–15% vs. 3%–13%) over 12 to 36 months, although statistical testing was not reported.220, 285 As a result, more participants withdrew from the liraglutide (8% to 33%) compared with the placebo arm (0% to 6%) because of adverse events;220, 259, 285 statistical testing was only presented in one study, which noted a statistical difference between groups (p=0.009). One trial reported on total mortality with 1 to 2 deaths per arm.285 Compared with placebo, there was no evidence that more participants on liraglutide developed depression (1%–17% vs. 0%–18%),220, 285 suicidal behavior and/or ideation (0.5% vs. 0.9%),285 or anxiety (2% vs. 1%)220 at 12 to 18 months (p=NR). The most common adverse events were gastrointestinal,285 and 77 to 79 percent of those randomized to liraglutide experienced at least one gastrointestinal event compared with 31 to 46 percent of those on placebo (p=NR).220, 259 Of those on liraglutide, 4 to 8 percent withdrew from the trial because of gastrointestinal adverse events compared with 1 to 2 percent of placebo participants (p=NR).220, 285
Other potential harms that are listed in the “warnings and precautions” section of the liraglutide label include malignant thyroid c-cell carcinomas (black box warning), pancreatitis, gallbladder disease, renal impairment, increased heart rate, hypersensitivity/anaphylaxis, hypoglycemia, and cancer.220, 259, 285 One large trial of individuals with prediabetes339 reported 10 cases of confirmed pancreatitis during 3 years among 1505 individuals randomized to liraglutide treatment (0.7%; 0.3 events per 100 person-years) compared with two cases in 747 placebo-group individuals (0.3%; 0.1 events per 100 person-years), with most events (8/12) occurring within the first year of treatment.339 Data on other outcomes were generally sparse among the trials.220, 259, 285
Lorcaserin
Four trials reported harms (or lack of harms) related to lorcaserin (n=6490).172, 173, 238, 268 More participants in the lorcaserin arms experienced at least one adverse event (12% at 1 month, 83% at 1 year) compared with those on placebo (4% at 1 month, 75% at 1 year), although statistical testing was not conducted (Table 16).173, 238 Compared with placebo, the adverse event most commonly associated with lorcaserin was dizziness, with 8 to 10 percent of those randomized to lorcaserin experiencing dizziness compared with 4 percent of controls (p=NR).172, 173, 268 Rates of serious adverse events were low in both groups (0% to 3% in lorcaserin and 0% to 2% in placebo; p=NR) (Table 17).172, 173, 238 In one trial, six serious adverse events were deemed to be potentially related to lorcaserin; three occurred in the placebo group (syncope, ventricular tachycardia, and anaphylactic reaction), and three occurred in the lorcaserin group (syncope, moderate depression, and acute anxiety attack).173 Withdrawals due to adverse events were less than 10 percent in both arms (7% in lorcaserin arm and 5% to 7% in placebo arm; statistical testing was not conducted).172, 173 There were only 2 deaths, both in control groups.172, 173 There was no evidence of increased risk of developing depression or suicidal ideation among those randomized to lorcaserin (2% to 3% and 1%, respectively) compared with placebo (2% and 1%) (p-values=NR).172, 173
Other potential harms that are listed in the “warnings and precautions” section of the lorcaserin label include serotonin syndrome, valvular heart disease, cognitive impairment, and priapism. There were no reports of serotonin syndrome and two studies that conducted echocardiograms during the trial did not report any increased incidence of valvular heart disease in those given lorcaserin.172, 173 There were scarce to no data on cognitive impairment, psychiatric disorders beyond depression, or priapism.
Naltrexone and Bupropion
Three trials reported harms (or lack of harms) related to naltrexone and bupropion (n=3453).218, 244, 311 More participants randomized to naltrexone and bupropion experienced at least one adverse event (83% to 86%) compared with those on placebo (69% to 75%) over 12 to 13 months, although statistical testing was not reported (Table 16).218, 244 The most frequent treatment-related adverse events during the primary treatment period were nausea, constipation, headache, dry mouth, and dizziness.218, 244, 311 Serious adverse events were rare and low in both the naltrexone and bupropion (0.3% to 2%) and placebo arms (0% to 1%) (Table 17). More participants withdrew from the naltrexone and bupropion group for adverse events (20% to 25%) compared with placebo (10% to 14%), although statistical testing was not reported.218, 244, 311 Of the two trials reporting deaths (n=1948), one death occurred in the naltrexone and bupropion group.244, 311 There was no statistically significant association with depression or anxiety; 0 to 5 percent in the naltrexone and bupropion arm developed depression and/or anxiety compared with 1 to 4 percent of the placebo arm.218, 244, 311
In the “warnings and precautions” sections of the naltrexone and bupropion label, additional potential harms include seizures, neuropsychiatric events, increased blood pressure/heart rate, cognitive effects, renal dysfunction (increases in creatinine), liver dysfunction, and glaucoma. Many of these warnings come from trials of naltrexone or bupropion alone. Two of the three trials noted that naltrexone and bupropion may attenuate the positive effects of weight loss on blood pressure as the naltrexone and bupropion arm did not have as much of a decrease in blood pressure (p<0.05),244, 311 and an average 1-bpm greater increase in heart rate (p-values<0.05)218, 244 compared with controls. The other harms were not well reported; however, those with certain conditions such as history of psychiatric illness and seizures were excluded from participating in the trials.
Orlistat
Seventeen trials160, 161, 222, 226, 227, 236, 239, 246, 260, 263, 273, 292, 297-299, 304, 307 (n=10,392) and two observational studies213, 248 (n=209,993) reported harms (or lack of harms) related to orlistat. Sixteen are from the previous review, and three are new as part of this update.248, 298, 299 More participants in the orlistat groups (80% to 96%) experienced at least one adverse event compared with those in the placebo group (67% to 94%) (k=8) over 6 to 18 months; statistical testing was only reported in three studies and between-group differences were significant (Table 16) (p<0.05). The number who withdrew for adverse events was also higher in the orlistat groups (2% to 16%) compared with placebo (0% to 7%), although statistical testing was not presented (k=14). However, the number of participants with serious adverse events was low in both groups and not consistently higher in those randomized to orlistat (0% to 15%) compared with placebo (2% to 26%) (Table 17) (p=NR; k=13). Six trials reported on deaths, but only 0 to 1 deaths were reported in each trial, and none were felt to be related to orlistat. One prescription event monitoring study of 16,021 orlistat users reported 33 deaths (0.21%) in orlistat users over 12 months, but none were felt to be related to orlistat.213
The most commonly reported adverse events were gastrointestinal.213 Sixty-three to 91 percent of participants randomized to orlistat experienced at least one gastrointestinal adverse event (e.g., intestinal borborygmi and cramps, flatus, fecal incontinence, oily spotting, and flatus with discharge) in the first 12 to 24 months of the trials compared with 39 to 65 percent of placebo participants (k=16);160, 161, 213, 222, 226, 227, 239, 246, 260, 263, 273, 297-299, 304, 307 only three trials reported statistical testing and all found statistically significant differences (p<0.05).222, 246, 304 Similarly, compared with placebo participants, more of those randomized to orlistat dropped out because of gastrointestinal adverse events (1%–10% vs. 0%–4%; p=NR; k=12).213, 222, 226, 227, 236, 239, 246, 263, 292, 297, 299, 307 The number of serious gastrointestinal adverse events was much lower in both groups, ranging from 2 to 10 percent in the orlistat group and from 1 to 3 percent in the placebo group (k=3; p=NR).161, 248, 307 There was no clear association with dosage (i.e., 120 mg TID was not associated with more adverse events or gastrointestinal adverse events than 60 mg TID). Gastrointestinal symptoms were described as being of relatively short duration and decreased over time with continued usage. Orlistat was not related to risk of colorectal cancer in a retrospective cohort (n=193,972) designed to examine this association.248
One trial (n=551) found an increased incidence of musculoskeletal problems/injuries in those randomized to orlistat (23%) compared with placebo (16%) (p≤0.05).222 In six trials, more of those randomized to orlistat had episodes of beta carotene or vitamins A, D, or E deficiency (low levels or need for supplementation) compared with those given placebo (0%–12% vs. 0%–8%);161, 239, 246, 292, 297, 307 however, statistical testing was only reported in one trial, which noted differences were significant for beta carotene and vitamin E (p-values<0.01).246
On the orlistat label, there are warnings for specific conditions, including cholelithiasis, liver injury, and impaired renal function. Four trials (n=1230) reported cholelithiasis or cholecystectomy events, with most trials having only 1 or 2 cases.226, 239, 292, 298 One trial (n=222) conducted gallbladder ultrasounds at baseline and at treatment end, reporting that 7 percent of those randomized to orlistat and 11 percent of those on placebo developed gallbladder abnormalities (mostly asymptomatic stones detected by ultrasound; p=NR) over 12 months.239 In the prescription event-monitoring study of 1602 orlistat users, there were 12 reported cases of abnormal liver tests;213 one subject (arm not identified) withdrew in a different trial because of a liver disorder.260 One trial that conducted kidney ultrasounds at baseline and end of treatment noted that renal abnormalities (mainly stones and cysts) developed in 3 percent of those on orlistat and 2 percent of those on placebo over 12 months;239 in a second trial, there was one person in the orlistat arm with a kidney stone exacerbation on orlistat.298
Phentermine and Topiramate
Three trials reported harms (or lack of harms) related to phentermine and topiramate (n=3837).168, 216, 241 In the only trial reporting this outcome, 85 percent of those on 15/92 mg phentermine and topiramate and 73 percent of those on placebo experienced at least one adverse event (p=NR) (Table 16).216 Serious adverse events were rare in all three trials (2%–5%, 1%–3%, and 0%–4% of those randomized to phentermine and topiramate 15/92 mg, 7.5/46 mg, and placebo, respectively); statistical testing was only reported in one study, with no between-group differences noted (Table 17).241 More participants withdrew from phentermine and topiramate (16%–21% on 15/92 mg and 12%–15% on 7.5/46 mg) compared with placebo (7% to 9%) over 6 to 12 months (p=NR).168, 216, 241 In the two trials reporting mortality, only one cardiovascular-related death was reported in the placebo arm of one trial.168, 241 Those randomized to 15/92 mg of phentermine and topiramate had more anxiety (4%) than those in the control arm (1% to 2%) (p≤0.01); the 7.5/46-mg dosage was not associated with increased anxiety compared with control.216, 241 Results on the effects on depression were mixed, with one trial finding a significantly increased incidence of depression in those randomized to 15/92 mg of phentermine and topiramate (5%) compared with placebo (1%) (p=0.0007);216 however, a second trial did not find a significant difference between groups (4% of those on 15/92 mg, 3% of those on 7.5/46 mg, and 3% of those on placebo had incident depression; p=0.90).241 There were no suicide attempts or ideation in either study.
The “warnings and precautions” section of the phentermine and topiramate label list additional potential harms, including fetal toxicity, myopia, mood disorders (irritability), cognitive dysfunction (attention), elevated heart rate, metabolic acidosis, and elevated creatinine. Fetal toxicity risk is based on registries and epidemiologic studies of topiramate alone (with an FDA REMS in place). There was a slightly higher incidence of blurred vision in those on 15/92 mg phentermine and topiramate (5% to 6%) compared with placebo (3% to 5%), but between-group differences were only significant in one of two studies reporting statistical significance; the 7.5/46-mg dose was not associated with an increased risk.168, 216, 241 Irritability and insomnia were higher in the phentermine and topiramate arms (2%–5% and 6%–12%, respectively) compared with placebo (<1%–2% and 5%–6%; p≤0.05).168, 216, 241 Those in phentermine and topiramate arms reported more disturbance in attention (3% to 7%) compared with placebo (<1%) (p<0.001).168, 216, 241 The trials monitored heart rate with conflicting findings.168, 216, 241 Mild decreases in bicarbonate were seen more frequently in those on phentermine and topiramate (p<0.05) but less than 2 percent of all arms experienced substantial reductions.216, 241
Medication-Based Weight Loss Maintenance Interventions
All three medication-based weight loss maintenance trials reported adverse events.247, 287, 312 The adverse events during weight loss maintenance interventions were similar to those seen during weight loss trials.
Orlistat
Two trials reported harms (or lack of harms) during weight loss maintenance with orlistat.247, 287 Adverse events, especially gastrointestinal-related adverse events, were higher in those on orlistat (88% to 95% with gastrointestinal-related adverse events) than placebo (63% to 68% with gastrointestinal-related adverse events) (p≤0.01 and p=NR, respectively). The number who withdrew for adverse events, especially gastrointestinal-related adverse events, was also generally higher in the orlistat groups (5%–15% and 7%–12% for any and gastrointestinal- related adverse events, respectively) compared with placebo (3% to 5% and 0.5%), although statistical testing was not presented. However, the number of participants with serious adverse events was not statistically different in those randomized to orlistat (12%) compared with placebo (18%) in the one study reporting this outcome (Table 16).287 Few participants (<4%) in one orlistat trial required additional vitamin supplementation, and the results are not described by study arm.247
Liraglutide
One trial reported harms (or lack of harms) during weight loss maintenance with liraglutide.312 Persons given liraglutide did not experience more adverse events overall (92%) compared with those on placebo (89%), although statistical testing was not presented (Table 16). However, more participants experienced gastrointestinal adverse events (74% vs. 45% for liraglutide vs. placebo, respectively; p=NR). More participants randomized to liraglutide experienced at least one serious adverse event (4%) than those on placebo (2%), although statistical testing was not conducted (Table 17). Although overall withdrawals for adverse events were similar in the two arms (9%), more participants in the liraglutide arm withdrew for gastrointestinal adverse events (5% vs. 0%; p=NR).312
Figures
Figure 4Pooled Analysis of Change in Weight (kg) at 12 to 18 Months in Behavior-Based Weight Loss Interventions Compared With Controls
Abbreviations: BL = baseline; Cancer = elevated cancer risk; CG = control group; CI = confidence interval; CV = increased cardiovascular risk; IG = intervention group; Intv = intervention; Low = low cardiovascular risk or unselected; MD = mean difference; Pop = population; SD = standard deviation; Subclinical = increased subclinical cardiovascular risk
Figure 5Pooled Analysis of Change in Weight at 24 Months in Behavior-Based Weight Loss Interventions Compared With Controls
Abbreviations: BL = baseline; Cancer = elevated cancer risk; CG = control group; CI = confidence interval; CV = increased cardiovascular risk; IG = intervention group; Intv = intervention; Low = low cardiovascular risk or unselected; MD = mean difference; Pop = population; SD = standard deviation; Subclinical = increased subclinical cardiovascular risk
Figure 7Pooled Analysis of Risk of Losing ≥5% of Body Weight at 12 to 18 Months in Behavior-Based Weight Loss Interventions Compared With Controls
Abbreviations: Cancer = elevated cancer risk; CG = control group; CI = confidence interval; CV = increased cardiovascular risk; IG = intervention group; Intv = intervention; Low = low cardiovascular risk or unselected; Pop = population; RR = risk ratio; Subclinical = increased subclinical cardiovascular risk
Figure 8Pooled Analysis of Risk of Losing ≥5% of Body Weight at 24 Months in Behavior-Based Weight Loss Interventions Compared With Controls
Abbreviations: Cancer = elevated cancer risk; CG = control group; CI = confidence interval; CV = increased cardiovascular risk; IG = intervention group; Intv = intervention; Low = low cardiovascular risk or unselected; Pop = population; RR = risk ratio; Subclinical = increased subclinical cardiovascular risk
Figure 9Pooled Analysis of Risk of Losing ≥10% of Body Weight at 12 to 18 Months in Behavior-Based Weight Loss Interventions Compared With Controls
Abbreviations: Cancer = elevated cancer risk; CG = control group; CI = confidence interval; CV = increased cardiovascular risk; IG = intervention group; Intv = intervention; Low = low cardiovascular risk or unselected; Pop = population; RR = risk ratio; Subclinical = increased subclinical cardiovascular risk
Figure 11Pooled Analysis for Prespecified Subgroups of Trials for Change in Weight at 12 to 18 Months in Behavior-Based Weight Loss Interventions Compared With Controls
*k=65. Two trials’ baseline mean BMI were not reported.
Abbreviations: BMI = body mass index; BL = baseline; CI = confidence interval; MD = mean difference; PCP = primary care provider
Figure 12Pooled Analysis of Change in Weight at 12 to 18 Months in Behavior-Based Weight Maintenance Interventions Compared With Controls
Abbreviations: BL = baseline; Cancer = elevated cancer risk; CG = control group; CI = confidence interval; CV = increased cardiovascular risk; IG = intervention group; Intv = intervention; Low = low cardiovascular risk or unselected; MD = mean difference; Pop = population; SD = standard deviation; Subclinical = increased subclinical cardiovascular risk
Figure 13Risk of Losing ≥5% of Body Weight in Medication-Based Weight Loss Interventions Compared With Controls, All Studies and All Time Points
Abbreviations: CG = control group; CI = confidence interval; CV = increased cardiovascular risk; IG = intervention group; Low = low cardiovascular risk or unselected; Pop = population; RR = risk ratio
Figure 14Proportion of Participants Losing ≥10% of Body Weight in Medication-Based Weight Loss Interventions Compared With Controls at Multiple Followup Time Points
Abbreviations: CG = control group; CI = confidence interval; CV = increased cardiovascular risk; IG = intervention group; Low = low cardiovascular risk or unselected; Pop = population; RR = risk ratio
Tables
Table 2Characteristics for All Trials, by Intervention Type and Author (k=124)
| Type | Author, year | Study name | PR | Quality | N rand | % FU (mos) | Study duration | Country | KQ1 | KQ2 | KQ3 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Behavior-based weight loss interventions | Ackermann, 2008214 | DEPLOY | Fair | 92 | 67.4 (12) | 12 | US | X | |||
| Ackermann, 2015215 | RAPID-YDPP | Fair | 509 | 84.5 (12) | 12 | US | X | X | |||
| Ahern, 2017323 | WRAP | Fair | 1267 | 64.9 (12) | 12 | UK | X | X | X | ||
| Anderson, 2014217 | BeWEL | Good | 329 | 92.7 (12) | 12 | UK | X | X | |||
| Appel, 2011219 | POWER Hopkins | Good | 415 | 85.5 (12) | 24 | US | X | X | X | ||
| Aveyard, 2016221 | Fair | 1882 | 75.4 (12) | 12 | UK | X | |||||
| Beeken, 2017318 | 10TT | X | Fair | 537 | 59.2 (12) | 24 | UK | X | |||
| Bennett, 2012224 | Be Fit, Be Well [POWER] | Good | 365 | 69.3 (12) | 24 | US | X | X | |||
| Bhopal, 2014225 | PODOSA | Good | 171 | 97.7 (36) | 36 | UK | X | X | |||
| Burke, 2005228 | ADAPT | X | Fair | 241 | 79.7 (16) | 40 | Australia | X | |||
| Cadmus-Bertram, 2016229 | HELP | Fair | 105 | 83.8 (12) | 12 | US | X | ||||
| Chirionos, 2016230 | CHARMS | Fair | 120 | 77.5 (12) | 12 | US | X | ||||
| Christian, 2011231 | Fair | 279 | 94.3 (12) | 12 | US | X | |||||
| Cohen, 1991232 | X | Fair | 30 | 100 (12) | 12 | US | X | ||||
| de Vos, 2014234 | PROOF | Fair | 407 | 90.4 (12) | 80 | The Netherlands | X | X | |||
| Demark-Wahnefried, 2014235 | DAMES | Good | 136 | 94.1 (12) | 12 | US | X | X | X | ||
| Eaton, 2016237 | Choose to Lose | Fair | 211 | 75.4 (12) | 24 | US | X | X | |||
| Fischer, 2016319 | Fair | 163 | 96.3 (12) | 12 | US | X | |||||
| Fitzgibbon, 2010240 | ORBIT | X | Fair | 213 | 89.2 (18) | 18 | US | X | |||
| Godino, 2016242 | SMART | Good | 404 | 93.3 (12) | 24 | US | X | X | |||
| Greaves, 2015243 | Waste the Waist | Fair | 108 | 88.9 (12) | 12 | UK | X | X | |||
| Haapala, 2009245 | X | Fair | 125 | 68.0 (12) | 12 | Finland | X | ||||
| Hunt, 2014249 | FFIT | Good | 748 | 92.0 (12) | 12 | Scotland | X | X | X | ||
| Huseinovic, 2016250 | Fair | 110 | 80.9 (12) | 12 | Sweden | X | |||||
| Jakicic, 2011251 | Fair | 269 | 72.9 (18) | 18 | US | X | X | ||||
| Jansson, 2013252 | Fair | 133 | 70.7 (12) | 24 | Sweden | X | X | ||||
| Jebb, 2011253 | Fair | 772 | 57.6 (12) | 24 | Germany, UK, Australia | X | X | ||||
| Jeffery, 1993254 | Trial of Food Provision and Monetary Incentives | X | Fair | 202 | 87.0 (12) | 30 | US | X | |||
| Jenkins, 2017320 | Fair | 919 | 64.7 (18) | 18 | Canada | X | |||||
| Jolly, 2011255 | Lighten Up | Fair | 740 | 68.0 (12) | 12 | UK | X | ||||
| Jones, 1999256 | HOT | X | Fair | 112 | 91.1 (30) | 30 | US | X | |||
| Kanke, 2015257 | Fair | 50 | 80.0 (12) | 12 | Japan | X | |||||
| Katula, 2011258 | HELP PD | Good | 301 | 90.7 (12) | 24 | US | X | X | |||
| Knowler, 2002205 | DPP | X | Good | 2161 | 95.0 (12) | 55 | US | X | X | X | |
| Kuller, 2012261 | WOMAN | Good | 508 | 89.8 (18) | 48 | US | X | ||||
| Kulzer, 2009262 | PREDIAS | X | Fair | 182 | 90.7 (12) | 12 | Germany | X | X | ||
| Kumanyika, 2012328 | Fair | 261 | 71.6 (12) | 12 | US | X | X | ||||
| Little, 2016264 | Fair | 818 | 81.4 (12) | 12 | UK | X | X | ||||
| Logue, 2005324 | REACH | Fair | 665 | 65.0 (12) | 24 | US | X | ||||
| Luley, 2014265 | Fair | 184 | 76.6 (12) | 12 | Germany | X | |||||
| Ma, 2013266 | E-LITE | Good | 241 | 91.7 (15) | 24 | US | X | X | |||
| Marrero, 2016267 | Fair | 225 | 77.8 (12) | 12 | US | X | |||||
| Martin, 2008269 | X | Fair | 144 | 64.6 (12) | 18 | US | X | ||||
| Mensink, 2003325 | SLIM | X | Fair | 114 | 80.7 (24) | 24 | The Netherlands | X | X | ||
| Mitsui, 2008270 | X | Fair | 46 | 93.5 (12) | 12 | Japan | X | ||||
| Moore, 2003271 | X | Fair | 843 | 67.0 (12) | 18 | UK | X | ||||
| Morgan, 2011272 | SHED-IT | Fair | 65 | 70.8 (12) | 12 | Australia | X | ||||
| Nakade, 2012274 | SCOP | Fair | 235 | 96.2 (12) | 24 | Japan | X | ||||
| Nanchahal, 2012275 | CAMWEL | Fair | 381 | 57.0 (12) | 12 | UK | X | X | |||
| Narayan, 1998276 | X | Fair | 95 | 92.6 (12) | 12 | US | X | ||||
| Nicklas, 2014277 | Balance after Baby | Fair | 75 | 80.0 (12) | 12 | US | X | ||||
| Nilsen, 2011327 | Fair | 213 | 85.4 (18) | 18 | Norway | X | |||||
| O’Brien, 2017321 | PREVENT-DM | Good | 63 | 92.1 (12) | 12 | US | X | X | |||
| Ockene, 2012278 | LLDPP | Fair | 312 | 92.6 (12) | 12 | US | X | X | X | ||
| Pacanowski, 2015279 | Fair | 162 | 83.3 (12) | 24 | US | X | |||||
| Parikh, 2010280 | HEED | X | Fair | 99 | 72.7 (12) | 12 | US | X | |||
| Patrick, 2011281 | Fair | 441 | 70.1 (12) | 12 | US | X | |||||
| Penn, 2009283 | EDIPS-Newcastle | Fair | 102 | 80.4 (12) | 60 | UK | X | ||||
| Phelan, 2017330 | Good | 371 | 81.9 (12) | 12 | US | X | X | ||||
| Puhkala, 2015286 | Fair | 113 | 84.1 (12) | 24 | Finland | X | |||||
| Rock, 2007289 | Fair | 70 | 92.9 (12) | 12 | US | X | X | X | |||
| Rock, 2015288 | ENERGY | Good | 697 | 84.2 (24) | 24 | US | X | ||||
| Rodriguez-Cristobal, 2017329 | IMOAP | Fair | 864 | 67.6 (12) | 24 | Spain | X | ||||
| Rosas, 2015290 | VAFO | Good | 207 | 83.6 (12) | 24 | US | X | X | |||
| Ross, 2012291 | PROACTIVE | Fair | 490 | 80.8 (24) | 24 | Canada | X | X | |||
| Shapiro, 2012293 | Text4Diet | Fair | 170 | 76.5 (12) | 12 | US | X | ||||
| Silva, 2009295 | X | Fair | 239 | 87.0 (12) | 24 | Portugal | X | ||||
| Stevens, 1993300 | TOHP I | X | Good | 564 | 93.6 (18) | 18 | US | X | |||
| Stevens, 2001301 | TOHP II | X | Good | 1191 | 92.0 (18) | 48 | US | X | X | ||
| Svetkey, 2015302 | CITY | Good | 365 | 89.0 (12) | 24 | US | X | ||||
| Thomas, 2017322 | Good | 271 | 86.3 (12) | 12 | US | X | |||||
| Tsai, 2010305 | Good | 50 | 94.0 (12) | 12 | US | X | X | ||||
| Tuomilehto, 2001306 | Finnish DPS | X | Good | 523 | 96.9 (12) | 126 | Finland | X | X | ||
| van Wier, 2011308 | ALIFE@WORK | Fair | 1386 | 57.6 (24) | 24 | The Netherlands | X | ||||
| von Gruenigen, 2012310 | SUCCEED | Fair | 75 | 78.7 (12) | 12 | US | X | X | |||
| Wadden, 2011206 | POWER-UP | Good | 261 | 85.1 (12) | 24 | US | X | X | X | ||
| Whelton, 1998326 | TONE | X | Good | 585 | 86.0 (18)# | 30 | US | X | X | ||
| Wing, 1998314 | Fair | 154 | 77.9 (12) | 24 | US | X | |||||
| Wylie-Rosett, 2001315 | Fair | 588 | 80.6 (12) | 12 | US | X | X | ||||
| Yeh, 2016316 | Fair | 60 | 96.7 (12) | 12 | US | X | |||||
| Behavior-based weight loss maintenance interventions | Cussler, 2008233 | HW4L | X | Fair | 135 | 82.2 (12) | 12 | US | X | ||
| Pekkarinen, 2015282 | Fair | 201 | 81.6 (12) | 24 | Finland | X | X | X | |||
| Perri, 1988284 | X | Fair | 123 | 74.0 (18) | 18 | US | X | ||||
| Sherwood, 2013294 | Keep It Off | Good | 419 | 86.6 (12) | 24 | US | X | ||||
| Simpson, 2015296 | WILMA | Fair | 166 | 83.7 (12) | 12 | UK | X | X | X | ||
| Svetkey, 2008303 | WLM | X | Good | 1032 | 95.4 (12) | 60 | US | X | |||
| Voils, 2017309 | Fair | 222 | 85.1 (13) | 13 | US | X | X | ||||
| Wing, 2006313 | STOP | Fair | 314 | 92.4 (12) | 18 | US | X | ||||
| Young, 2017317 | Good | 92 | 82.6 (12) | 36 | Australia | X | |||||
| Medication-based Weight loss interventions | Acharya, 2006213 | X | Fair | NA | NA† | 12 | UK | X | |||
| Allison, 2012216 | EQUIP | Fair | 1026 | 59.9 (13) | 13 | US | X | X | |||
| Apovian, 2013218 | COR-11 | Fair | 1496 | 53.8 (13) | 13 | US | X | X | X | ||
| Aronne, 2013168 | EQUATE | Fair | 324 | 99.7 (6) | 6 | US | X | ||||
| Astrup, 2012220 | Fair | 191 | 63.1 (12) | 24 | Europe‡ | X | X | X | |||
| Bakris, 2002222 | Orlistat and Resistant Hypertension | X | Fair | 554 | 96.6 (12) | 12 | US | X | |||
| Broom, 2002226 | Orlistat UK Study | X | Fair | 142 | 96.5 (6) | 12 | UK | X | |||
| Broom, 2002227 | UK Multimorbidity Study | X | Fair | 531 | 65.3 (12) | 12 | UK | X | X | ||
| Davidson, 1999160 | X | Fair | 892 | 66.3 (12) | 24 | US | X | X | |||
| Derosa, 2003236 | X | Fair | 50 | 96.0 (12) | 12 | Italy | X | X | |||
| Farr, 2016238 | Fair | 48 | 75.0 (1) | 1 | US | X | |||||
| Fidler, 2011173 | BLOSSOM | Fair | 3203 | 55.5 (12) | 12 | US | X | X | X | ||
| Finer, 2000239 | X | Fair | 228 | 61.0 (12) | 12 | UK | X | X | |||
| Gadde, 2011241 | CONQUER/SEQUEL | Fair | 2487 | 69.3 (12) | 25 | US | X | X | X | ||
| Greenway, 2010244 | COR-1 | Fair | 1164 | 59.9 (13) | 13 | US | X | X | X | ||
| Hauptman, 2000246 | X | Fair | 635 | 67.2 (12) | 24 | US | X | X | |||
| Hong, 2013248 | Fair | 193,972 | NR | NA† | UK | X | |||||
| Kim, 2013259 | Fair | 68 | 75.0 (3.5) | 4 | US | X | |||||
| Krempf, 2003260 | X | Fair | 696 | 61.1 (18) | 18 | France | X | X | |||
| Lindgarde, 2000263 | Swedish Multimorbidity Study | X | Fair | 376 | 85.9 (12) | 12 | Sweden | X | X | ||
| Martin, 2011268 | Fair | 57 | 91.2 (2) | 2 | US | X | |||||
| Muls, 2001273 | ObelHyx | X | Fair | 294 | 86.7 (6) | 12 | Belgium | X | |||
| Pi-Sunyer, 2015285 | SCALE Obesity and Prediabetes | Fair | 3731 | 69.4 (13) | 36 | Multisite§ | X | X | X | ||
| Rossner, 2000292 | X | Fair | 729 | 71.9 (12) | 24 | Europe | X | X | X | ||
| Sjostrom, 1998297 | X | Fair | 688 | 79.1 (12) | 24 | Europe‖ | X | X | |||
| Smith, 2010172 | BLOOM | Fair | 3182 | 49.7 (12) | 24 | US | X | X | X | ||
| Smith, 2011298 | Fair | 131 | 96.9 (6) | US, Sweden | X | ||||||
| Smith, 2012299 | Fair | 435 | 57.9 (6) | 6 | US | X | |||||
| Swinburn, 2005304 | X | Fair | 339 | 79.4 (12) | 12 | Australia, New Zealand | X | X | X | ||
| Torgerson, 2004161 | XENDOS | X | Fair | 3305 | 83.1 (12) | 48 | Sweden | X | X | ||
| Van Gaal, 1998307 | Orlistat Dose-Ranging Study Group | X | Fair | 367 | 79.1 (6) | 6 | Europe¶ | X | |||
| Wadden, 2011311 | COR-BMOD | Fair | 793 | 51.3 (13) | 12 | US | X | X | X | ||
| Medication-based weight loss maintenance interventions | Hill, 1999247 | X | Fair | 542 | 73.7 (12) | 12 | US | X | X | ||
| Richelsen, 2007287 | X | Fair | 309 | 64.7 (36) | 36 | Scandinavia | X | X | |||
| Wadden, 2013312 | SCALE Maintenance | Fair | 422 | 72.3 (13) | 16 | US, Canada | X | X |
- *
- †
Not RCT
- ‡
8 EU countries
- §
27 countries
- ‖
15 EU sites, specific countries NR
- ¶
Austria, Belgium, Brazil, Finland, Germany, Italy, Sweden, Switzerland, and UK
- #
For full sample, including overweight and non-overweight participants
Abbreviations: 10TT = Ten Top Tips; ADAPT = Activity, Diet and Blood Pressure Trial; BLOOM = Behavioral Modification and Lorcaserin for Overweight and Obesity Management; CAMWEL = Camden Weight Loss; BLOSSOM = Behavioral Modification and Lorcaserin Second Study for Obesity Management; CHARMS = Community Health and Risk-reduction for Metabolic Syndrome; CITY = Cell Phone Intervention for You; COR-1 = Contrave Obesity Research-1; COR-11 = CONTRAVE Obesity Research-II; COR-BMOD = Contrave Obesity Research - Behavior Modification; DAMES = Daughters And Mothers Against Breast Cancer; DEPLOY = Diabetes Education & Prevention with a Lifestyle Intervention offered at the YMCA; DPP = Diabetes Prevention Program; DPS = Diabetes Prevention Study; EDIPS = European Diabetes Prevention Study; E-LITE = Evaluation of Lifestyle Interventions to Treat Elevated Cardiometabolic Risk in Primary Care; ENERGY = Exercise and Nutrition to Enhance Recovery and Good Health for You; FFIT = Football Fans in Training; FU = followup; HEED = Project Help Educate to Eliminate Diabetes; HELP PD = Healthy Partnerships to Prevent Diabetes; HOT = Hypertension Optimal Treatment; HW4L = Healthy Weight for Life; IMOAP = Group motivational intervention in overweight/obese patients in primary prevention of cardiovascular disease in the primary healthcare area; KQ = key question; LLDPP = Lawrence Latino Diabetes Prevention Project; mos = months; ObelHyx = Obesity Linked with Hypercholesterolemia treated with Xenical; ORBIT = Obesity Reduction Black Intervention; PODOSA = Prevention of Diabetes and Obesity in South Asians; POWER = Practice Based Opportunities for Weight Reduction; POWER-UP = Practice-based Opportunities for Weight Reduction at the University of Pennsylvania; PREDIAS = Prevention of Diabetes Self-Management Program; PROACTIVE = Prevention and Reduction of Obesity through Active Learning; PR = previous review; PREVENT-DM = The Promotora Effectiveness Versus Metformin Trial; PROOF = Prevention of Knee Osteoarthritis in Overweight Females; rand = randomized; RAPID-YDPP = Reaching Out to Prevent Increases in Diabetes - YMCA model for Diabetes Prevention Program; REACH = Reasonable Eating and Activity to Change Health; SCOP = Saku Control Obesity Program; SHED-IT = Self-Help, Exercise, and Diet using Information Technology; SLIM = Study on lifestyle-intervention and impaired glucose tolerance Maastricht; SMART = Social Mobile Approaches to Reduce weighT; STOP = Study to Prevent Regain; SUCCEED = Survivors of Uterine Cancer Empowered by Exercise and Healthy Diet; TOHP = Trials of Hypertension Prevention Phase; TONE = Group motivational intervention in overweight/obese patients in primary prevention of cardiovascular disease in the primary healthcare area; UK = United Kingdom; US = United States; VAFO = Vivamos Activos Fair Oaks; WILMA = Weight Loss Maintenance in Adults; WLM = Weight Loss Maintenance; WOMAN = Women on the Move through Activity and Nutrition; WRAP = Weight-loss programme referrals for adults in primary care; XENDOS = XENical in the prevention of Diabetes in Obese Subjects
Table 3Population Characteristics for All Included Trials, Sorted by Intervention Type and Author (k=124)
| Intervention type | Author, year (Study name; medication) | Population description | Risk category | N rand | Self-selected | Eligible BMI (kg/m2) | Mean BL BMI (kg/m2)(SD) | Mean BL WC (cm) | Mean age | Female (%) | Race/Ethnicity (%) | Baseline comorbidities (%)* |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Behavior-based weight loss | Ackermann, 2008214 (DEPLOY) | Adults with prediabetes | Sub CV Risk | 92 | Yes | ≥24 | 31.4 (5.0) | NR | 58.3 | 55.4 | White: 81.5 Black: 12.0 Hisp: 3.3 Other: 5.4 | Prediabetes: 100 |
| Ackermann, 2015215 (RAPID-YDPP) | Adults with prediabetes, aged ≥18 years | Sub CV Risk | 509 | No | ≥24 | 36.8 (8.5) | NR | 51.0 | 70.7 | White: 35.0 Black: 57.0 Hisp: 3.1 Other: 4.9 | Prediabetes: 100 | |
| Ahern, 2017323 (WRAP) | Adults aged ≥18 years | Low Risk/Unselected | 1267 | No | ≥28 | 34.5 (5.2) | 110.4 | 53.2 | 67.8 | White: 89.7 Black: 1.8 Asian: 2.8 Other: 1.2 | NR | |
| Anderson, 2014217 (BeWEL) | Adults with screen-detected colorectal adenoma, aged 50-74 years | Cancer Risk | 329 | No | >25 | 30.7 (4.2) | 104.3 | 63.6 | 26.1 | White: 99.4 Asian: 0.3 Other: 0.3 | Diabetes: 14.0 | |
| Appel, 2011219 (POWER Hopkins) | Adults with ≥1 CV risk factor, aged >21 years | CV Risk | 415 | No | 30-50 | 36.6 (5.0) | 118.1 | 54.0 | 63.6 | White: 56.1 Black: 41.0 Hisp: 2.2 Asian: 1.0 Other: 1.9 | Diabetes: 23.1 Dyslipidemia: 67.7 Hypertension: 76.3 | |
| Aveyard, 2016221 | Adults, aged ≥18 years | Low Risk/Unselected | 1882 | No | ≥30† | 34.9 (4.9) | NR | 56.0 | 57.2 | White: 94.9 Black: 1.5 Asian: 2.6 AI/NA: 0.0 Other: 0.7 | NR | |
| Beeken, 2017318 (10TT) | Adults, aged ≥ 18 years | Low Risk/Unselected | 537 | No | ≥ 30 | 35.0 (NR) | 111.5 | 59.4 | 65.7 | White: 94.9 Black: 1.9 Asian: 2.2 Other: 0.9 | NR | |
| Bennett, 2012224 (Be Fit, Be Well [POWER]) | Adults with hypertension, aged ≥21 years | CV Risk | 365 | No | 30-50 | 37.0 (5.1) | NR | 54.6 | 68.5 | White: 3.6 Black: 71.2 Hisp: 13.2 Asian: 1.1 AI/NA: 1.6 Other: 0.8 | Hypertension: 100 | |
| Bhopal, 2014225 (PODOSA) | South Asian adults with prediabetes, aged ≥35 years | Sub CV Risk | 171 | No | NR‡ | 30.5 (4.8) | 103.0 | 52.5 | 54.4 | Other: 100 | Prediabetes: 100 | |
| Burke, 2005228 (ADAPT) | Adults with hypertension, aged 40-70 years | CV Risk | 241 | Yes | >25 | 30.1 (2.7) | 95.2 | 56.2 | 55.6 | NR | Diabetes: 0 Hypertension: 100 | |
| Cadmus-Bertram, 2016229 (HELP) | Women with history of breast cancer or elevated risk, aged 40-75 years | Cancer Risk | 105 | No | ≥27.5 | 32.1 (4.0) | NR | 60.2 | 100 | White: 86.6 | NR | |
| Chirionos, 2016230 (CHARMS) | Adults with metabolic syndrome, ages 30-70 years | CV Risk | 120 | NR | ≥25 | NR | 104.9 | 51.7 | 55.8 | White: 5.0 Black: 10.9 Hisp: 84.0 Asian: 0 AI/NA: 0 Other: 0 | Diabetes: 0 | |
| Christian, 2011231 | Adults with ≥2 components of the metabolic syndrome, aged 18-75 years | CV Risk | 279 | No | ≥25 | 34.3 (7.4) | 115.3 | 49.6 | 68.4 | White: 50.6 Hisp: 44.1 Other: 5.3 | Diabetes: 0 | |
| Cohen, 1991232 | Adults with hypertension, aged 20-75 years | CV Risk | 30 | No | ≥27.8 (men), ≥27.3 (women) | 34.1 (NR) | NR | 59.5 | 73.3 | NR | Hypertension: 100 | |
| de Vos, 2014234 (PROOF) | Women, aged 50-60 years, free of knee osteoarthritis | Low Risk/Unselected | 407 | No | ≥27.0 | 32.4 (4.3) | 105.5 | 55.7 | 100 | White: 93.4 Black: 0.6 Asian: 1.4 Other: 4.6 | Hypertension: 71.5 | |
| Demark-Wahnefried, 2014235 (DAMES) | Mother/daughter dyads (post-menopausal breast cancer survivor and her adult daughters) | Cancer Risk | 136 | Yes | 25-39.9 | 31.0 (2.6) | 96.1 | 61.3 | 100 | White: 74.0 Black: 18.0 Hisp: 7.0 Asian: 1.0 AI/NA: 0.0 Other: 0.0 | NR | |
| Eaton, 2016237 (Choose to Lose) | Adults, aged 18-79 years | Low Risk/Unselected | 211 | No | ≥25 | 37.7 (6.6) | 115.4 | 48.5 | 79.2 | White: 82.9 Black: 9.5 Hisp: 4.3 Other: 3.3 | Diabetes: 16.6 Dyslipidemia: 41.7 Hypertension: 49.3 | |
| Fischer, 2016319 | Adults with prediabetes adults, aged ≥ 18 years | Sub CV Risk | 163 | No | 25-50 | NR | NR | 46.4 | 75.8 | NR | Diabetes: 0 Prediabetes: 100 | |
| Fitzgibbon, 2010240 (ORBIT) | African American women, aged 30-65 years | Low Risk/Unselected | 213 | Yes | 30-50 | 39.2 (5.7) | NR | 46.0 | 100 | White: 0 Black: 100 Asian: 0 AI/NA: 0 Other: 0 | NR | |
| Godino, 2016242 (SMART) | College students, aged 18 to 35 years | Low Risk/Unselected | 404 | Yes | ≥25.0-34.9 | 29.0 (2.7) | 87.8 | 22.7 | 70.3 | White: 41.8 Black: 3.7 Hisp: 30.9 Asian: 23.8 AI/NA: 1.5 Other: 20.0 | NR | |
| Greaves, 2015243 (Waste the Waist) | Adults with ≥1 CV risk factor, aged 40–74 years | CV Risk | 108 | No | ≥28 | 32.7 (3.1) | 110.0 | 65.1 | 30.6 | White: 100 Black: 0 Asian: 0 AI/NA: 0 Other: 0 | Diabetes: 0 Prediabetes: 8.5 | |
| Haapala, 2009245 | Adults, aged 25-44 years | Low Risk/Unselected | 125 | Yes | 26-36 | 30.5 (2.7) | 97.6 | 38.1 | 77.4 | NR | Diabetes: 0 | |
| Hunt, 2014249 (FFIT) | Men, aged 35-65 years | Low Risk/Unselected | 748 | Yes | ≥28.0 | 35.3 (4.9) | 118.4 | 47.1 | 0 | White: 98.4 Other: 0.9 | NR | |
| Huseinovic, 2016250 | Postpartum women | Low Risk/Unselected | 110 | Yes | ≥27 | 31.7 (3.7) | 97.8 | 32.2 | 100 | NR | NR | |
| Jakicic, 2011251 | Adults, aged 18-55 years | Low Risk/Unselected | 269 | Yes | 25-29.9 | 27.1 (1.7) | 90.4 | 44.4 | 91.4 | White: 79.8 Black: 14.9 Hisp: 1.6 Asian: 1.2 AI/NA: 0.4 Other: 1.6 | NR | |
| Jansson, 2013252 | Adults, aged 18-70 years | Low Risk/Unselected | 133 | No | NR§ | 33.7 (NR) | NR | 47.0 | 72.2 | NR | Diabetes: 13.5 Dyslipidemia: 33.1 Hypertension: 36.8 | |
| Jebb, 2011253 | Adults with ≥1 risk factor for obesity-related disease, aged ≥18 years | CV Risk | 772 | No | 27–35 | 31.4 (2.6) | 99.9 | 47.4 | 86.5 | NR | Diabetes: 6.6 | |
| Jeffery, 1993254 (Trial of Food Provision and Monetary Incentives) | Adults, aged 25-45 years | Low Risk/Unselected | 202 | Yes | NR‖ | 31.0 (NR) | NR | 37.5 | 50.0 | White: 92.1 Other: 7.9 | NR | |
| Jenkins, 2017320 | Adults, aged ≥ 18 years | Low Risk/Unselected | 919 | Yes | >25 | 32.4 (NR) | 101.4 | 44.7 | 77.3 | White: 60.0 Other: 28.7 | Diabetes: 0 | |
| Jolly, 2011255 (Lighten Up) | Adults, aged ≥18 years | Low Risk/Unselected | 740 | No | ≥30¶ | 33.8 (3.8) | NR | 49.3 | 69.3 | White: 87.5 Black: 6.0 Asian: 3.0 Other: 3.5 | NR | |
| Jones, 1999256 (HOT) | Adults with hypertension, aged 50-80 years | CV Risk | 112 | NR | ≥27 | 34.0 (6.0) | NR | 58.0 | 52.0 | White: 59.8 Black: 40.2 | Diabetes: 0 Hypertension: 100 | |
| Kanke, 2015257 | Japanese adults with ≥1 CV risk factor, aged 30-69 years | CV Risk | 50 | No | ≥25 | NR | NR | NR | 36.0 | Asian: 100 | Diabetes: 16.0 Dyslipidemia: 38.0 Hypertension: 84.0 | |
| Katula, 2011258 (HELP PD) | Adults with prediabetes, aged ≥21 years | Sub CV Risk | 301 | Yes | 25-39.9 | 32.7 (4.0) | 104.7 | 57.9 | 57.5 | White: 74.0 Black: 24.7 Hisp: 1.3 Other: 1.3 | Diabetes: 0 Prediabetes: 100 Hypertension: 0 | |
| Knowler, 2002 (DPP) | Adults with prediabetes, aged ≥25 years | Sub CV Risk | 2161 | Yes | ≥24 | 34.0 (6.7) | 105.1 | 50.4 | 68.5 | White: 54.0 Black: 19.6 Hisp: 16.0 Asian: 5.0 AI/NA: 5.5 | Diabetes: 0 Prediabetes: 100 Dyslipidemia: 44.1 Hypertension: 30.0 | |
| Kuller, 2012261 (WOMAN) | Postmenopausal women, current or recent users of hormone therapy, aged 52-62 years | Low Risk/Unselected | 508 | Yes | 25-39.9 | 30.8 (3.8) | 105.9 | 57.0 | 100 | White: 88.0 Black: 11.0 | Diabetes: 0 Dyslipidemia: 0 Hypertension: 0 | |
| Kulzer, 2009262 (PREDIAS) | Adults with prediabetes, aged 20-70 years | Sub CV Risk | 182 | NR | ≥26 | 31.5 (5.3) | 106.6 | 56.3 | 43.0 | NR | Diabetes: 0 Prediabetes: 100 | |
| Kumanyika, 2012328 | Adults with obesity, ages 18-70 years | Low Risk/Unselected | 261 | No | 27-55 | 37.2 (6.4) | 111.4 | 47.2 | 84.3 | White: 18.0 Black: 65.0 Hisp: 16.0 Asian: 1.0 | Diabetes: 18.4 Hypertension: 43.7 | |
| Little, 2016264 | Adults, aged ≥18 years | Low Risk/Unselected | 818 | No | ≥30# | 36.7 (5.7) | NR | 53.7 | 63.6 | NR | Diabetes: 16.6 | |
| Logue, 2005324 (REACH) | Adults, aged 40-69 years | Low Risk/Unselected | 665 | Yes | >27†††† | NR | NR | NR | 68.9 | Black: 26.3 | Diabetes: 13.8 Dyslipidemia: 33.4 Hypertension: 43.5 | |
| Luley, 2014265 | Adults with metabolic syndrome, aged 30-60 years | CV Risk | 184 | Yes | NR** | 33.3 (5.2) | 109.8 | 50.2 | 41.0 | NR | Diabetes: 0 | |
| Ma, 2013266 (E-LITE) | Adults with prediabetes or metabolic syndrome, aged ≥18 years | CV Risk | 241 | No | ≥25 | 32.0 (5.4) | 106.3 | 52.9 | 46.5 | White: 78.0 Hisp: 4.1 Asian: 17.0 | Diabetes: 0 Prediabetes: 54.0 | |
| Marrero, 2016267 | Adults with prediabetes adults, aged ≥18 years | Sub CV Risk | 225 | Yes | ≥24†† | 36.8 (7.1) | NR | 51.6 | 84.8 | White: 64.4 Black: 25.3 Hisp: 6.0 Asian: 6.7 Other: 1.8 | Diabetes: 0 | |
| Martin, 2008269 | African American women, aged 18-65 years | Low Risk/Unselected | 144 | No | ≥25 | 39.1 (7.7) | 110.3 | 41.8 | 100 | White: 0 Black: 100 Hisp: 0 Asian: 0 AI/NA: 0 Other: 0 | NR | |
| Mensink, 2003325 (SLIM) | Adults, aged 40-70 years | Sub CV Risk | 114 | No | ≥25‡‡‡‡ | 29.5 (0.5) | 102.4 | 56.7 | 43.9 | White: 100 Black: 0 Hisp: 0 Asian: 0 AI/NA: 0 Other: 0 | Diabetes: 0 Prediabetes: 100 | |
| Mitsui, 2008270 | Japanese adults, aged 50-69 years | Low Risk/Unselected | 46 | Yes | NR‡‡ | 25.2 (2.4) | 93.8 | 63.3 | 54.3 | Asian: NR§§ | Hypertension: 17.4 | |
| Moore, 2003271 | Adults, aged 16-64 years | Low Risk/Unselected | 843 | No | ≥30 | 36.9 (5.7) | NR | 48.6 | 73.9 | NR | NR | |
| Morgan, 2011272 (SHED-IT) | Men, aged 18–60 years | Low Risk/Unselected | 65 | Yes | 27-37 | 30.6 (2.8) | 103.1 | 35.9 | 0 | NR | NR | |
| Nakade, 2012274 (SCOP) | Japanese adults, aged 40-64 years | Low Risk/Unselected | 235 | No | ≥28.4 | 30.6 (3.1) | 102.2 | 54.2 | 50.0 | White: 0 Black: 0 Hisp: 0 Asian: 100 AI/NA: 0 Other: 0 | Dyslipidemia: 56.2 Hypertension: 69.5 | |
| Nanchahal, 2012275 (CAMWEL) | Adults, aged ≥18 years | Low Risk/Unselected | 381 | No | ≥25 | 33.5 (5.5) | 106.7 | 48.8 | 72.2 | White: 72.6 | Diabetes: 12.3 | |
| Narayan, 1998276 | Gila River Indian Community adults, aged 25-54 years | Low Risk/Unselected | 95 | Yes | ≥27 (men), ≥25 (women) | 34.9 (NR) | 113.0 | 33.5 | 75.8 | White: 0 Black: 0 Asian: 0 AI/NA: 100 Other: 0 | Diabetes: 0 | |
| Nicklas, 2014277 (Balance after Baby) | Postpartum (6 weeks) women with prior gestational diabetes mellitus, aged 18-45 years | Sub CV Risk | 75 | No | ≥24‖‖ | 31.4 (5.6) | NR | 33.4 | 100 | White: 57.3 Black: 30.7 Hisp: 20.0 Asian: 12.0 | Diabetes: 0 Prediabetes: 32.0 | |
| Nilsen, 2011327 | Adults, aged 18-64 years | Sub CV Risk | 213 | No | NA§§§§ | 36.8 (6.0) | NR | 46.5 | 50.0 | NR | Diabetes: 0 Hypertension: 73.7 | |
| O’Brien, 2017321 (PREVENT-DM) | Hispanic women with prediabetes, aged ≥20 years | Sub CV Risk | 63 | Yes | ≥23 | 33.4 (7.0) | 98.3 | 44.8 | 100 | White: 0 Black: 0 Hisp: 100 Asian: 0 AI/NA: 0 Other: 0 | Diabetes: 0 Prediabetes: 100 Dyslipidemia: NR Hypertension: NR | |
| Ockene, 2012278 (LLDPP) | Latino/Hispanic adults at risk of developing diabetes aged ≥25 years | Sub CV Risk | 312 | No | >24 | 33.9 (5.5) | 104.4 | 51.9 | 74.4 | Hisp: 100 | Diabetes: 0 | |
| Pacanowski, 2015279 | Adults, ≥18 years | Low Risk/Unselected | 162 | Yes | ≥27 | 33.5 (5.0) | NR | 46.6 | 81.9 | White: 88.9 Black: 3.7 Hisp: 0.6 Asian: 1.2 AI/NA: 1.9 Other: 1.3 | Diabetes: 0 | |
| Parikh, 2010280 (HEED) | Adults with prediabetes, aged ≥18 years | Sub CV Risk | 99 | Yes | ≥25 | 31.5 (4.8) | 101.6 | 48.0 | 85.0 | Black: 9.0 Hisp: 89 | Diabetes: 0 Prediabetes: 100 Dyslipidemia: 25.0 Hypertension: 31.0 | |
| Patrick, 2011281 | Men, aged 25-55 years | Low Risk/Unselected | 441 | Yes | ≥25 | 34.2 (4.1) | 113.3 | 43.9 | 0 | White: 71.0 Black: 5.2 Hisp: 18.1 Asian: 1.6 AI/NA: 0.5 Other: 1.6 | NR | |
| Penn, 2009283 (EDIPS-Newcastle) | Adults with prediabetes, aged >40 years | Sub CV Risk | 102 | No | >25 | 33.8 (5.0) | 104.4 | 57.1 | 59.8 | NR | Prediabetes: 100 | |
| Phelan, 2017330 | Low-income postpartum women, aged 18-40 years | Low Risk/Unselected | 371 | No | 25-40 | 31.7 (5.1) | 98.4 | 28.1 | 100.0 | Hisp: 81.6 | Diabetes: 0.0 | |
| Puhkala, 2015286 | Men, aged 30-62 years who are truck or bus drivers | Low Risk/Unselected | 113 | Yes | NR## | 33.0 (4.5) | 114.4 | 47.0 | 0 | NR | NR | |
| Rock, 2007289 | Women | Low Risk/Unselected | 70 | NR | ≥25 | 34.0 (3.5) | 111.6 | 41.1 | 100 | White: 57.1 Black: 10.0 Hisp: 22.9 Asian: 2.9 Other: 7.1 | NR | |
| Rock, 2015288 (ENERGY) | Breast cancer survivors | Cancer Risk | 697 | Yes | 25-45 | 31.5 (4.6) | 104.2 | 56.0 | 100 | White: 79.0 Black: 10.3 Hisp: 6.6 AI/NA: 1.6 Other: 2.2 | Diabetes: 5.8 | |
| Rodriguez-Cristobal, 2017329 (IMOAP) | Adults, aged 30-70 years | Low Risk/Unselected | 864 | No | >25 | 34.1 (4.8) | 107.7 | 56.5 | 77.2 | NR | Diabetes: 17.1 Dyslipidemia: 60.2 | |
| Rosas, 2015290 (VAFO) | Latino adults with ≥1 CV risk factor | CV Risk | 207 | No | 30-60 | 35.6 (5.3) | NR | 47.1 | 76.8 | Hisp: 100.0 | Diabetes: 43.0 | |
| Ross, 2012291 (PROACTIVE) | Sedentary adults | Low Risk/Unselected | 490 | No | 27-39*** | 32.3 (4.2) | 106.6 | 51.8 | 70.2 | NR | NR | |
| Shapiro, 2012293 (Text4Diet) | Adults, aged 21-65 years | Low Risk/Unselected | 170 | Yes | 25.0-39.9 | 32.2 (4.1) | NR | 41.9 | 65.0 | White: 64.0 | NR | |
| Silva, 2009295 | Premenopausal women, aged 25-50 years | Low Risk/Unselected | 239 | Yes | 25-40 | 31.5 (4.1) | NR | 37.6 | 100 | NR | NR | |
| Stevens, 1993300 (TOHP I) | Adults with prehypertension, aged 30-54 years | Sub CV Risk | 564 | NR | 26.1-36.1 (men), 24.3-36.1 (women) | 29.5 (2.8) | NR | 42.8 | 31.7 | White: 79.4 Black: 18.6 | Diabetes: 0 Hypertension: 0 | |
| Stevens, 2001301 (TOHP II) | Adults with prehypertension, aged 30-54 years | Sub CV Risk | 1191 | Yes | 26.1-37.4 (men), 24.4-37.4 (women) | 31.0 (3.2) | NR | 43.3 | 34.3 | White: 78.8 Black: 17.5 | Diabetes: 0 Hypertension: 0 | |
| Svetkey, 2015302 (CITY) | Adults, aged 18-35 years | Low Risk/Unselected | 365 | Yes | ≥25 | 35.2 (7.8) | 110.0 | 29.4 | 69.6 | White: 56.2 Black: 36.2 Hisp: 5.8 Other: 7.7 | Hypertension: 16.2 | |
| Thomas, 2017322 | Adults, aged 18-70 years | Low Risk/Unselected | 271 | Yes | 27-40 | 33.9 (3.7) | NR | 55.0 | 77.5 | White: 91.5 Black: 5.9 Hisp: 2.2 Asian: 1.1 AI/NA: 0.4 | NR | |
| Tsai, 2010305 | Adults | Low Risk/Unselected | 50 | Yes | 27–50 | 36.5 (1.6) | 112.3 | 49.4 | 88.0 | White: 20.0 Black: 80.0 | Diabetes: 0 | |
| Tuomilehto, 2001306 (Finnish DPS) | Adults with prediabetes, aged 40-65 years | Sub CV Risk | 523 | Yes | >25 | 31.2 (4.5) | 101.3 | 55.0 | 67.0 | NR | Diabetes: 0 Prediabetes: 100 Dyslipidemia: 5.2 Hypertension: 30.5 | |
| van Wier, 2011308 (ALIFE@WORK) | Adults | Low Risk/Unselected | 1386 | No | ≥25 | 29.6 (3.5) | 101.7 | 43.0 | 33.0 | NR | NR | |
| von Gruenigen, 2012310 (SUCCEED) | Endometrial cancer survivors | Cancer Risk | 75 | No | ≥25 | 36.4 (7.6) | 106.4 | 57.9 | 100 | White: 90.7 Black: 6.7 Other: 2.7 | Diabetes: 21.3 Hypertension: 33.3 | |
| Wadden, 2011 (POWER-UP)206 | Adults with 2 of 5 components of metabolic syndrome, aged ≥21 years | CV Risk | 261 | No | 30-50 | 38.5 (4.7) | 118.4 | 51.8 | 79.7 | White: 59.8 Black: 37.6 Hisp: 4.6 Asian: 0.7 | Diabetes: 21.0 Dyslipidemia: 65.5 Hypertension: 70.9 | |
| Whelton, 1998326 (TONE) | Hypertensive adults, aged 60-80 years | CV Risk | 585 | No | ≥27.3 | 31.2 (2.3) | NR | 66.0 | 52.6 | White: 71.8 Black: 28.2 | Hypertension: 100 | |
| Wing, 1998314 | Adults at risk of diabetes,††† aged 40-55 years | Sub CV Risk | 154 | Yes | NR‡‡‡ | 35.9 (4.3) | NR | 45.7 | 79.0 | NR | Diabetes: 0 | |
| Wylie-Rosett, 2001315 | Adults | Low Risk/Unselected | 588 | Yes | ≥25§§§ | 35.6 (6.5) | 105.2 | 52.1 | 82.3 | White: 83.0 | NR | |
| Yeh, 2016316 | Chinese adults with prediabetes | Sub CV Risk | 60 | No | ≥23 | 26.1 (2.3) | 90.6 | 58.8 | 56.7 | White: 0 Black: 0 Hisp: 0 Asian: 100 AI/NA: 0 Other: 0 | Diabetes: 0 Prediabetes: 100 | |
| Behavior-based weight loss maintenance | Cussler, 2008233 (HW4L) | Adult peri-menopausal women, aged 40-55 years | Low Risk/Unselected | 135 | Yes | 25.0-38.0 | 30.7 (3.6) | NR | 48.2 | 100 | NR | NR |
| Pekkarinen, 2015282 | Adults, aged 18-65 years | Low Risk/Unselected | 201 | No | ≥35 | 41.7 (6.1) | NR | 47.3 | 71.4 | NR | NR | |
| Perri, 1988284 | Adults, aged 22-59 years | Low Risk/Unselected | 123 | Yes | NR‖‖‖ | NR | NR | NR | 78.9 | NR | NR | |
| Sherwood, 2013294 (Keep It Off) | Adults who lost ≥10% of their body weight during past year | Low Risk/Unselected | 419 | Yes | ≥20.5 | 28.4 (5.0) | NR | 46.4 | 81.6 | White: 91.2 Black: 5.2 Asian: 3.3 Other: 1.0 | NR | |
| Simpson, 2015296 (WILMA) | Adults who lost ≥5% of their weight in prio 12 months, aged 18-70 years | Low Risk/Unselected | 166 | Yes | ≥30 | 34.2 (5.9) | 104.1 | NR | 84.3 | White: 94.6 Other: 5.4 | Diabetes: 18.1 Dyslipidemia: 22.9 Hypertension: 39.2 | |
| Svetkey, 2008303 (WLM) | Adults with ≥1 CV risk factor, aged ≥ 25 years | CV Risk | 1032 | Yes | 25-45 | 34.1 (4.8) | NR | 55.6 | 63.4 | Black: 37.6 Other: 62.4 | Diabetes: 0 Dyslipidemia: 40.0 Hypertension: 87.0 | |
| Voils, 2017309 | Veterans, aged 18-75 years | Low Risk/Unselected | 222 | Yes | ≥30 | 34.0 (6.1) | 122 | 61.8 | 15.3 | White: 58.1 Black: 37.4 Other: 2.7 | Hypertension: 0.0 | |
| Wing, 2006313 (STOP) | Adults who lost ≥10% of their weight within prior 2 years | Low Risk/Unselected | 314 | Yes | NR | 28.6 (4.8) | NR | 51.3 | 81.2 | NR | NR | |
| Young, 2017317 | Men, aged 18-65 years | Low Risk/Unselected | 92 | Yes | 25-40 | 30.7 (NR) | 109.2 | 49.2 | 0 | NR | NR | |
| Medication-based weight loss | Acharya, 2006213 (Orlistat) | Adults prescribed orlistat | Low Risk/Unselected | NA | NR | NR | NR | NR | 45 | 80.1 | NR | NR |
| Allison, 2012216 (EQUIP; Phen/Tpm) | Adults, aged 18-70 years | Low Risk/Unselected | 1026 | NR | ≥35 | 42.0 (6.1) | 120.3 | 42.6 | 82.7 | White: 80.1 Black: 18.1 Hisp: 15.1 Asian: 0.8 AI/NA: 1.3 Other: 1.1 | NR | |
| Apovian, 2013218 (COR-11; Nal/Bup) | Adults, aged 18-65 years | Low Risk/Unselected | 1496 | NR | 30-45¶¶¶ | 36.2 (4.4) | 108.8 | 44.3 | 84.7 | White: 83.3 Black: 13.7 Other: 2.7 | Diabetes: 0 Dyslipidemia: 55.0 Hypertension: 21.3 | |
| Aronne, 2013168 (EQUATE; Phen/Tpm) | Adults, aged 18-70 years | Low Risk/Unselected | 324 | NR | 30-45 | 36.2 (3.9) | 110.6 | 44.7 | 79.0 | White: 77.5 Black: 20.7 Other: 2.2 | Diabetes: 0 Dyslipidemia: 21.0 Hypertension: 28.7 | |
| Astrup, 2012220 (Liraglutide) | Adults, aged 18-65 years | Low Risk/Unselected | 191 | Yes | 30-40 | 34.8 (2.8) | 108.5 | 45.9 | 75.0 | NR | Diabetes: 4.0 Prediabetes: 31.0 | |
| Bakris, 2002222 (Orlistat and Resistant Hypertension; Orlistat) | Adults with hypertension, aged ≥40 years | CV Risk | 554 | NR | 28-43 | 35.6 (3.9) | 109.7 | 52.9 | 61.1 | White: 85.5 Black: 11.5 Hisp: 2.4 Other: 0.6 | Diabetes: 8.4 Dyslipidemia: 37.5 Hypertension: 100 | |
| Broom, 2002226 (Orlistat UK Study; Orlistat) | Adults with dyslipidemia, aged ≥18 years | CV Risk | 142 | NR | ≥30 | 36.8 (5.9) | NR | 51.5 | 60.6 | NR | Diabetes: 24.8 Dyslipidemia: 100 | |
| Broom, 2002227 (UK Multimorbidity Study; Orlistat) | Adults with ≥1 CV risk factor, aged 18-80 years | CV Risk | 531 | NR | ≥28 | 37.0 (6.3) | 108.2 | 46.0 | 78.4 | NR | Prediabetes: 17.0 Dyslipidemia: 72.0 Hypertension: 43.0 | |
| Davidson, 1999160 (Orlistat) | Adults, aged ≥18 years | Low Risk/Unselected | 892 | NR | 30-43 | 36.3 (0.5) | NR | 43.5 | 84.2 | White: 80.8 Black: 14.0 Hisp: 4.2 | Diabetes: 4.1 Prediabetes: 6.0 | |
| Derosa, 2003236 (Orlistat) | Adults with dyslipidemia, aged >40 years | CV Risk | 50 | No | >30 | 31.9 (1.2) | 101.5 | 52.0 | 52.0 | NR | Dyslipidemia: 100 Hypertension: 0 | |
| Farr, 2016238 (Lorcaserin) | Adults | Low Risk/Unselected | 48 | NR | NR### | 36.9 (2.8) | 118.1 | 47.4 | 52.1 | NR | NR | |
| Fidler, 2011173 (BLOSSOM; Lorcaserin) | Adults, aged 18-65 years | Low Risk/Unselected | 3203 | No | 30-45¶¶¶ | 36.0 (4.2) | 109.5 | 43.8 | 79.2 | White: 66.9 Black: 19.5 Hisp: 11.1 Asian: 0.6 Other: 1.8 | Diabetes: 0 Prediabetes: 1.4 Dyslipidemia: 27.9 Hypertension: 24.0 | |
| Finer, 2000239 (Orlistat) | Adults, aged ≥18 years | Low Risk/Unselected | 228 | Yes | 30-43 | 36.8 (3.6) | NR | 41.4 | 88.5 | White: 94.9 Black: 1.4 Other: 3.7 | Diabetes: 0 | |
| Gadde, 2011241 (CONQUER/SEQUEL; Phen/Tpm) | Adults with ≥1 CV risk factor, aged 18-70 years | CV Risk | 2487 | No | 27-45 | 36.6 (4.5) | 113.3 | 51.1 | 69.8 | White: 86.0 Black: 11.9 Asian: 1.1 AI/NA: 0.6 Other: 1.0 | Diabetes: 15.8 Prediabetes: 67.7 Dyslipidemia: 36.1 Hypertension: 52.5 | |
| Greenway, 2010244 (COR-1; Nal/Bup) | Adults, aged 18-65 years | Low Risk/Unselected | 1164 | NR | 30-45¶¶¶ | 36.1 (4.2) | 109.4 | 44.0 | 85.2 | White: 75.6 Black: 18.6 Other: 5.9 | Diabetes: 0 Dyslipidemia: 49.1 Hypertension: 20.9 | |
| Hauptman, 2000246 (Orlistat) | Adults, aged >18 years | Low Risk/Unselected | 635 | NR | 30-44 | 36.0 (0.3) | NR | 42.5 | 78.3 | White: 90.9 Black: 6.8 Hisp: 1.9 AI/NA: 0.2 Other: 0.3 | NR | |
| Hong, 2013248 (Orlistat) | Adults, aged ≥18 years | Low Risk/Unselected | 19,3972 | No | NR | 35.7 (NR) | NR | 47 | 77.7 | NR | Diabetes: 6.1 Dyslipidemia: 1.8 Hypertension: 5.6 | |
| Kim, 2013259 (Liraglutide) | Adults with prediabetes, aged 40-70 years | Sub CV Risk | 68 | Yes | 27-40 | 31.9 (3.1) | 104.8 | 58.0 | 64.7 | White: 68.6 | Prediabetes: 100 | |
| Krempf, 2003260 (Orlistat) | Adults, aged 18-65 years | Low Risk/Unselected | 696 | NR | ≥28 | 36.1 (0.2) | 106.1 | 41.0 | 86.4 | NR | Diabetes: 0 | |
| Lindgarde, 2000263 (Swedish Multimorbidity Study; Orlistat) | Adults with ≥1 CV risk factor, aged 18-75 years | CV Risk | 376 | NR | 28-38 | 33.2 (3.0) | 106 | 53.5 | 63.6 | NR | Diabetes: 26.1 Dyslipidemia: 39.9 Hypertension: 74.5 | |
| Martin, 2011268 (Lorcaserin) | Adults, aged 18-65 years | Low Risk/Unselected | 57 | NR | 27-45 | 35.5 (4.8) | 108.0 | 48.7 | 68.4 | White: 63.2 Other: 36.8 | NR | |
| Muls, 2001273 (ObelHyx; Orlistat) | Adults with dyslipidemia, aged 18-70 years | CV Risk | 294 | NR | 27-40 | 32.9 (3.6) | 102.9 | 48.6 | 80.7 | NR | Diabetes: 0 Dyslipidemia: 100 | |
| Pi-Sunyer, 2015285 (SCALE Obesity and Prediabetes; Liraglutide) | Adults, aged ≥18 years | Low Risk/Unselected | 3731 | No | ≥30¶¶¶ | 38.3 (6.4) | 114.8 | 45.1 | 78.5 | White: 84.9 Black: 9.5 Hisp: 10.5 Asian: 3.6 AI/NA: 0.2 Other: 1.6 | Diabetes: 0 Prediabetes: 61.2 Dyslipidemia: 29.4 Hypertension: 34.8 | |
| Rossner, 2000292 (Orlistat) | Adults, aged ≥18 years | Low Risk/Unselected | 729 | NR | 28-43 | 35.1 (3.9) | NR | 44.2 | 82.3 | NR | NR | |
| Sjostrom, 1998297 (Orlistat) | Adults, aged ≥18 years | Low Risk/Unselected | 688 | Yes | 28-47 | 36.0 (NR) | 105.6 | 44.8 | 83.0 | NR | NR | |
| Smith, 2010172 (BLOOM; Lorcaserin) | Adults, aged 18-65 years | Low Risk/Unselected | 3182 | NR | 30-45¶¶¶ | 36.2 (0.1) | 109.4 | 44.1 | 83.4 | White: 66.8 Black: 18.7 Hisp: 12.4 Asian: 0.8 AI/NA: 0.5 Other: 0.6 | Diabetes: 0 | |
| Smith, 2011298 (Orlistat) | Adults, aged 18-60 years | Low Risk/Unselected | 131 | NR | 25-34.9**** | 31.0 (2.1) | 100.4 | 43.4 | 82.9 | White: 76.4 Black: 19.5 Hisp: 3.3 Asian: 0.8 | Diabetes: 0 | |
| Smith, 2012299 (Orlistat) | Active duty US army soldiers | Low Risk/Unselected | 435 | No | NR | 33.3 (3.4) | NR | NR | 25.3 | NR | NR | |
| Swinburn, 2005304 (Orlistat) | Adults with ≥1 CV risk factor, aged 40-70 years | CV Risk | 339 | No | 30-50 | 37.8 (5.0) | 113.6 | 52.2 | 56.9 | NR | Diabetes: 26.8 Dyslipidemia: 65.5 Hypertension: 56.6 | |
| Torgerson, 2004161 (XENDOS; Orlistat) | Adults, aged 30-60 years | Low Risk/Unselected | 3305 | Yes | ≥30 | 37.3 (4.3) | 115.2 | 43.3 | 55.2 | NR | Diabetes: 0 Prediabetes: 21.2 | |
| Van Gaal, 1998307 (Orlistat Dose-Ranging Study Group; Orlistat) | Adults, aged ≥18 years | Low Risk/Unselected | 367 | NR | 28-43 | 34.7 (4.0) | NR | 41.7 | 77.7 | NR | Diabetes: 0 | |
| Wadden, 2011 (Med)311 (COR-BMOD; Nal/Bup) | Adults, aged 18-65 years | Low Risk/Unselected | 793 | NR | 30-45¶¶¶ | 36.5 (4.2) | 109.2 | 45.8 | 89.9 | White: 69.8 Black: 23.8 Other: 6.3 | Diabetes: 0 | |
| Medication-based weight loss maintenance | Hill, 1999247 (Orlistat) | Adults, aged ≥18 years | Low Risk/Unselected | 542 | NR | 28-43 | 32.8 (0.2) | NR | 46.1 | 83.9 | White: 88.4 Black: 5.2 Hisp: 5.6 Other: 0.7 | Diabetes: 0 |
| Richelsen, 2007287 (Orlistat) | Adults with ≥1 CV risk factor, aged 18-65 years | CV Risk | 309 | NR | 30-45 | 37.5 (NR) | 119 | 47.0 | 50.8 | NR | Diabetes: 22.3 Prediabetes: 26.9 | |
| Wadden, 2013312 (SCALE Maintenance; Liraglutide) | Adults | Low Risk/Unselected | 422 | NR | ≥30¶¶¶ | 35.6 (5.9) | 108.6 | 46.2 | 81.5 | White: 84.1 Black: 13.5 Other: 2.6 | Diabetes: 0 Dyslipidemia: 29.4 Hypertension: 31.2 |
- *
Prediabetes defined by impaired fasting glucose (FPG: 100-125 mg/dL (5.6-6.9 mmol/L), impaired glucose tolerance (2 hour plasma glucose in the 75-g oral glucose tolerance test of 140-199 mg/dL (7.8-11.0 mmol/L), or A1C 5.7−6.4% (39−47 mmol/mol)
- †
Or, BMI ≥25 if Asian ethnicity
- ‡
WC ≥90 cm (men) or ≥80 cm (women)
- §
Patients seeking advice about overweight/obesity
- ‖
14-32 kg overweight
- ¶
Or, BMI ≥28 kg/m2 to <30 kg/m2 (≥23 to <25 kg/m2 for South Asians) required to have CV risk factor
- #
Or, BMI ≥28 to <30 kg/m2 with CV risk factor
- **
WC >80 cm (women), >94 cm (men)
- ††
≥23 if Asian
- ‡‡
WC ≥85 cm (men) or ≥90 cm (women)
- §§
Assume 100% given setting
- ‖‖
≥22 if Asian
- ¶¶
≥30% likelihood of being diagnosed with diabetes over the succeeding 7.5 years per risk factor algorithm
- ##
WC ≥100 cm
- ***
WC ≥102 cm (men) or ≥88 cm (women)
- †††
One or two biological parents with type 2 diabetes
- ‡‡‡
30-100% overweight
- §§§
Or, BMI>24 kg/m2 with CV risk factor
- ‖‖‖
20-100% over ideal weight
- ¶¶¶
Or, BMI ≥27 to <30 kg/m2 with CV risk factor
- ###
Article states that population has obesity but no inclusion BMI provided
- ****
WC >102 cm (men) or >88 cm (women)
- ††††
>27 or WHR >0.950 for men, >0.800 for women
- ‡‡‡‡
≥25 (or family history of DM)
- §§§§
FINDRISC (Finnish Diabetes Risk questionnaire) -score ≥9
Abbreviations: 10TT = Ten Top Tips; ADAPT = Activity, Diet and Blood Pressure Trial; AI/AN = American Indian/Alaska Native; BL = baseline; BLOOM = Behavioral Modification and Lorcaserin for Overweight and Obesity Management; BMI = body mass index; CAMWEL = Camden Weight Loss; cm = centimeter; BLOSSOM = Behavioral Modification and Lorcaserin Second Study for Obesity Management; BMI = body mass index; CHARMS = Community Health and Risk-reduction for Metabolic Syndrome; CITY = Cell Phone Intervention for You; cm = centimeter; COR-1 = Contrave Obesity Research-1; COR-11 = CONTRAVE Obesity Research-II; COR-BMOD = Contrave Obesity Research - Behavior Modification; CV = cardiovascular; DAMES = Daughters And Mothers Against Breast Cancer; DEPLOY = Diabetes Education & Prevention with a Lifestyle Intervention offered at the YMCA; DPP = Diabetes Prevention Program; DPS = Diabetes Prevention Study; EDIPS = European Diabetes Prevention Study; E-LITE = Evaluation of Lifestyle Interventions to Treat Elevated Cardiometabolic Risk in Primary Care; ENERGY = Exercise and Nutrition to Enhance Recovery and Good Health for You; FFIT = Football Fans in Training; FPG = Fasting Plasma Glucose; FU = followup; HEED = Project Help Educate to Eliminate Diabetes; IMOAP = Group motivational intervention in overweight/obese patients in primary prevention of cardiovascular disease in the primary healthcare area; kg = kilogram; KQ = key question; HELP PD = Healthy Partnerships to Prevent Diabetes; Hisp = Hispanic; HOT = Hypertension Optimal Treatment; HW4L = Healthy Weight for Life; LLDPP = Lawrence Latino Diabetes Prevention Project; mmol/L = millimoles per liter; Nal-Bup = Naltrexone HCL and bupropion HCL; NR = not reported; ObelHyx = Obesity Linked with Hypercholesterolemia treated with Xenical; ORBIT = Obesity Reduction Black Intervention; Phen-Top = Phentermine-topiramate extended release; PODOSA = Prevention of Diabetes and Obesity in South Asians; POWER = Practice Based Opportunities for Weight Reduction; POWER-UP = Practice-based Opportunities for Weight Reduction at the University of Pennsylvania; PREDIAS = Prevention of Diabetes Self-Management Program; PREVENT-DM = The Promotora Effectiveness Versus Metformin Trial; PROACTIVE = Prevention and Reduction of Obesity through Active Learning; PR = previous review; PROOF = Prevention of Knee Osteoarthritis in Overweight Females; rand = randomized; RAPID-YDPP = Reaching Out to Prevent Increases in Diabetes - YMCA model for Diabetes Prevention Program; REACH = Reasonable Eating and Activity to Change Health; SCOP = Saku Control Obesity Program; SHED-IT = Self-Help, Exercise, and Diet using Information Technology; SLIM = Study on lifestyle-intervention and impaired glucose tolerance Maastricht; SMART = Social Mobile Approaches to Reduce weighT; STOP = Study to Prevent Regain; SUCCEED = Survivors of Uterine Cancer Empowered by Exercise and Healthy Diet; TOHP = Trials of Hypertension Prevention Phase; TONE = Group motivational intervention in overweight/obese patients in primary prevention of cardiovascular disease in the primary healthcare area; VAFO = Vivamos Activos Fair Oaks; WC = waist circumference; WILMA = Weight Loss Maintenance in Adults; WLM = Weight Loss Maintenance; WOMAN = Women on the Move through Activity and Nutrition; WRAP = Weight-loss programme referrals for adults in primary care; XENDOS = XENical in the prevention of Diabetes in Obese Subjects
Table 4Behavior-Based Weight Loss Intervention Characteristics (k=80, 105 intervention arms)
| Author, year (Study name) | IG | Brief description | Main mode of delivery | In-person support | Duration (mos) | Core components | Support components | Total # of sessions in first 12 mos | Setting | PCP involved? | Provider |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ackermann, 2008214 (DEPLOY) | IG1 | YMCA-DPP group-based diabetes prevention intervention | Group | X | Total: 12 Core: 5 Support: 7 | 1 × brief individual session (2-5 min) 16 × group sessions (60-90 min) | 7-9 × group sessions (min NR) | 23 | Community (YMCA) | No | YMCA instructor |
| Ackermann, 2015215 (RAPID-YDPP) | IG1 | YMCA-DPP group-based diabetes prevention intervention | Group | X | Total: 12 Core: 6 Support: 6 | 16 × group sessions (60-90 min) | 6-8 × group sessions (60 min) | 24 | Community (YMCA) | No | YMCA instructor |
| Ahern, 2017 (WRAP)323 | IG1 | Weight Watchers (52-weeks) | Group | X | Total: 12 Core: 12 Support: 0 | 52 × group sessions (min NR) | 52 | Community | No | NR | |
| IG2 | Weight Watchers (12-weeks) | Group | X | Total: 3 Core: 3 Support: 0 | 12 × group sessions (min NR) | 12 | Community | No | NR | ||
| Anderson, 2014217 (BeWEL) | IG1 | Individual counseling plus telephone followup | Individual + Phone | X | Total: 12 Core: 3 Support: 9 | 3 × individual sessions (60 min) | 9 × telephone consultations (15 min) | 12 | Research center | NR | Lifestyle counselor |
| Appel, 2011219 (POWER Hopkins) | IG1 | Web-based self-monitoring and feedback plus in- person counseling | Mixed | X | Total: 24 Core: 24 Support: 0 | 24 × group counseling sessions (90 min) 27 × individual counseling sessions (20 min) 15 × phone sessions (20 min) + weekly visits to website and monthly email messages | +36 | Research clinic and home (web-based) | Yes | Lifestyle coach | |
| IG2 | Telephone coaching and web-based monitoring | Phone with tech support | Total: 24 Core: 24 Support: 0 | 33 × telephone calls (20 min) plus web-based self-monitoring | 21 | Home (web- and telephone-based) | Yes | Lifestyle coach | |||
| Aveyard, 2016221 | IG1 | Referral to free weight loss program (Slimming World) and FU appointment | Group | X | Total: 3 Core: 3 Support: 0 | 1 × individual session (<30 sec) 1 × followup appointment (NR min) 12 × optional group sessions (60 min) | 14 | Primary care | Yes | PCP | |
| Beeken, 2017318 (10TT) | IG1 | Individual counseling | Individual | X | Total: 3 Core: 3 Support: 0 | 1 × individual session (30 min) | 1 | Primary care clinic | Yes | Nurse or health care assistant | |
| Bennett, 2012224 (Be Fit, Be Well [POWER]) | IG1 | Web-based weight loss and hypertension self-monitoring and feedback plus telephone support | Phone with tech support | Total: 24 Core: 24 Support: 0 | Web-based self-monitoring 18 × telephone calls (20 min) 12 × optional group sessions (min NR) | 12 | Home (web-based) and community health center | Yes | Community health educator and PCP endorsement | ||
| Bhopal, 2014225 (PODOSA) | IG1 | Family-based dietary counseling | Individual | X | Total: 36 Core: 36 Support: 0 | 15 × individual counseling sessions (min NR) 3 × group sessions (min NR) | 8 | Home or community | No | Dietitian | |
| Burke, 2005228 (ADAPT) | IG1 | Individual and group-based counseling focused on decreasing blood pressure | Mixed | X | Total: 16 Core: 4 Support: 12 | 1 × individual session (30 min) 6 × group sessions (90 min) 5 nontailored print handouts | ≥6 × individual counseling sessions (min NR) 6 × group sessions (90 min) 4 nontailored print handouts “Regular” telephone contact | 19 | NR | No | NR |
| Cadmus-Bertram, 2016229 (HELP) | IG1 | Telephone coaching and web-based monitoring | Phone with tech support | Total: 12 Core: 6 Support: 6 | 12 × health coaching telephone calls (30 min) plus web-based self-monitoring | 6 × health coaching telephone calls (30 min) plus web-based self-monitoring | 18 | Home (telephone- and web-based) | No | Lay health coach | |
| Chirionos, 2016230 (CHARMS) | IG1 | DPP-based group counseling | Group | X | Total: 12 Core: 3 Support: 9 | 8 × group sessions (90 min) | 9 × monthly group counseling sessions (90 min) | 17 | NR | No | Research staff |
| Christian, 2011231 | IG1 | Computer-based self-management program with PCP feedback | Tech | X | Total: 6 Core: 6 Support: 0 | Computer-based self-management program plus 2 × individual sessions (min NR) | 2 | Community health center | Yes | Computer expert system and PCP | |
| Cohen, 1991232 | IG1 | PCP counseling on dietary changes | Individual | X | Total: 12 Core: 12 Support: 0 | 12 × individual sessions (min NR) | 12 | Primary care | Yes | PCP | |
| de Vos, 2014234 (PROOF) | IG1 | Individual counseling (Motivational interviewing) and group PA sessions | Individual | X | Total: 30 Core: 6 Support: 24 | Individual session (240 min, # of sessions NR) 20 × group physical activity sessions (60 min) | FU visits (NR) | 24 | NR | NR | Dietitian and physical therapist |
| Demark-Wahnefried, 2014235 (DAMES) | IG1 | Tailored print materials | Total: 12 Core: 12 Support: 0 | 6 mailed surveys and tailored print materials | 0 | Home (print-based) | NR | NA | |||
| IG2 | Tailored print materials using mother-daughter team-based approach | Total: 12 Core: 12 Support: 0 | 6 mailed surveys and tailored print materials | 0 | Home (print-based) | NR | NA | ||||
| Eaton, 2016237 (Choose to Lose) | IG1 | Individual counseling plus telephone and tailored print support | Individual + Phone | X | Total: 24 Core: 12 Support: 12 | 3 × individual sessions (90 min) 8 × phone calls (25 min) 12 printed materials (tailored exercise feedback reports) 2 exercise-related DVDs | 18 printed materials (tailored and non-tailored) 4 exercise feedback reports 2 nutrition-related DVDs | 11 | Research clinic | Yes | Registered dietitian |
| Fischer, 2016319 | IG1 | Text messages | Tech | Total: 12 Core: 12 Support: 0 | 6 × weekly text messages | 0 | Home | No | NR | ||
| Fitzgibbon, 2010240 (ORBIT) | IG1 | Intensive group and individual counseling | Mixed | X | Total: 18 Core: 6 Support: 12 | 52 × group sessions (60-90 min) 6 × individual motivational interview sessions (20-30 min) 26 weekly newsletters | 52 × group sessions (45-60 min) 12 × individual sessions (20-30 min) 12 × group exercise (min NR) 12 monthly newsletters | 80 | University | No | Research intervent-ionist |
| Godino, 2016242 (SMART) | IG1 | Social networking intervention | Tech | Total: 24 Core: 24 Support: 0 | Participants encouraged to interact with study technology (Facebook, mobile apps, website, technology-based communication with health coach) at least 5 times per week | 0 | Home (web-based) | No | Health coach | ||
| Greaves, 2015243 (Waste the Waist) | IG1 | Group counseling | Group | X | Total: 9 Core: 1 Support: 8 | 4 × group sessions (120 min) | 5 × group sessions (90 min) | 9 | Community | No | Lifestyle coach |
| Haapala, 2009245 | IG1 | Text-based intervention (Weight Balance®) | Tech | Total: 12 Core: 12 Support: 0 | Daily mobile phone messages as initiated by participants | 0 | Home (telephone-based) | No | NR | ||
| Hunt, 2014249 (FFIT) | IG1 | Group counseling and supervised exercise sessions | Group | X | Total: 12 Core: 3 Support: 9 | 12 × group and PA sessions (90 min) | 1 × group session (NR min) + 6 email prompts every 6-8 weeks | 12 | Community | NR | Community coaching staff |
| Huseinovic, 2016250 | IG1 | Individual counseling session plus ongoing phone and text-based support | Phone | Total: 12 Core: 3 Support: 9 | 1 × individual counseling session (0 min) followed by biweekly text messages or phone calls to track weight and provide feedback | Standardized monthly emails | 1 | Primary care | No | Dietitian | |
| Jakicic, 2011251 | IG1 | High physical activity prescription supported with individual and group counseling | Mixed | X | Total: 18 Core: 6 Support: 12 | 6 × individual sessions (min NR) 18 group sessions (min NR) | 24 × group sessions (min NR) 24 × telephone calls (min NR) | 48 | NR | NR | Physical activity counselor |
| IG2 | Moderate physical activity prescription supported with individual and group counseling | Mixed | X | Total: 18 Core: 6 Support: 12 | 6 × individual sessions (min NR) 18 × group sessions (min NR) | 24 × group sessions (min NR) 24 × telephone calls (min NR) | 48 | NR | NR | PA counselor | |
| Jansson, 2013252 | IG1 | Individual and telephone counseling | Individual + Phone | X | Total: 24 Core: 24 Support: 0 | 10 × individual sessions (min NR) 4 × telephone calls (min NR) | 5 | Primary care | NR | Research nurse and physio-therapist | |
| Jebb, 2011253 | IG1 | Free access to weekly Weight Watchers meetings | Group | X | Total: 12 Core: 12 Support: 0 | 52 × group sessions (min NR) | 52 | Community-based Weight Watchers sites | No | Weight Watchers group leader | |
| Jeffery, 1993254 (Trial of Food Provision and Monetary Incentives) | IG1 | Group counseling plus food provision and incentive | Group | X | Total: 18 Core: 18 Support: 0 | 33 × group sessions (min NR) | 28 | NR | No | Research intervent-ionist | |
| IG2 | Group counseling plus food provisions | Group | X | Total: 18 Core: 18 Support: 0 | 33 × group sessions (min NR) | 28 | NR | No | Intervent-ionist | ||
| IG3 | Group counseling plus incentive | Group | X | Total: 18 Core: 18 Support: 0 | 33 × group sessions (min NR) | 28 | NR | No | Intervent-ionist | ||
| IG4 | Group counseling | Group | X | Total: 18 Core: 18 Support: 0 | 33 × group sessions (min NR) | 28 | NR | No | Intervent-ionist | ||
| Jenkins, 2017320 | IG1 | Telephone counseling | Phone | Total: 6 Core: 6 Support: 0 | 9 × phone calls (20-30 mins) | 9 | Home (telephone-based) | No | NR | ||
| IG2 | Telephone counseling and food basket | Phone | Total: 6 Core: 6 Support: 0 | 9 × phone calls (20-30 mins) plus weekly food basket | 9 | Home (telephone-based) | No | NR | |||
| IG3 | Food basket | Phone | Total: 6 Core: 6 Support: 0 | Weekly food basket | 0 | Home | No | NA | |||
| Jolly, 2011255 (Lighten Up) | IG1 | NHS Size Down program | Group | X | Total: 3 Core: 3 Support: 0 | 8 × weekly group sessions (120 min) | 8 | Community | No | Community food advisors | |
| IG2 | Weight Watchers | Group | X | Total: 3 Core: 3 Support: 0 | 12 × weekly group sessions (60 min) | 12 | Community | No | NR | ||
| IG3 | Slimming World | Group | X | Total: 3 Core: 3 Support: 0 | 12 × weekly group sessions (90 min) | 12 | Community | No | NR | ||
| IG4 | Rosemary Conley | Group | X | Total: 3 Core: 3 Support: 0 | 12 × weekly group sessions (90 min) | 12 | Community | No | NR | ||
| IG5 | NHS General Practice counseling | Individual | X | Total: 3 Core: 3 Support: 0 | 1 × initial session (30 min) 11 × weekly individual sessions (15-20 min) | 12 | Primary care | Yes | PCP | ||
| IG6 | NHS Pharmacy counseling | Individual | X | Total: 3 Core: 3 Support: 0 | 1 × initial session (30 min) 11 × weekly individual sessions (15-20 min) | 12 | Pharmacy | No | Pharmacist | ||
| IG7 | Participant choice of intervention | Group | X | Total: 3 Core: 3 Support: 0 | 12 × weekly group or one-on-one sessions (min NR) | 12 | Community | Yes | Mixed by program (community members, PCPs, or pharmacists) | ||
| Jones, 1999256 (HOT) | IG1 | Individual and group counseling | Mixed | X | Total: 30 Core: 3 Support: 27 | 2 × individual sessions (min NR) 6 × group sessions (min NR) | 4-9 × group sessions (min NR) | 9 | NR | No | Registered dietitian |
| Kanke, 2015257 | IG1 | Individual PCP counseling | Individual | X | Total: 12 Core: 12 Support: 0 | 6-12 × individual sessions (7 min) | 12 | Primary care | Yes | PCP | |
| Katula, 2011258 (HELP PD) | IG1 | DPP-based group and individual counseling with community health worker and registered dietitian | Mixed | X | Total: 24 Core: 6 Support: 18 | 3 × individual sessions (min NR) 24 × group sessions (min NR) | 18 × phone sessions (min NR) 18 × group sessions (min NR) | 39 | Community | NR | Community health workers |
| Knowler, 2002205 (DPP) | IG1 | Intensive lifestyle intervention with individual counseling as well as optional exercise sessions | Individual | X | Total: 38 Core: 6 Support: 32 | 1 × initial individual session (20-30 min) 16 × individual sessions (30-45 min) 48 × optional supervised exercise sessions (45-60 min) | 32 × individual sessions with in-person contact at least every other month (30-45 min) 248 × optional supervised exercise sessions (45-60 min) 11 × optional group courses (min NR) | 23 | Research clinic | No | Case managers |
| Kuller, 2012261 (WOMAN) | IG1 | Group counseling | Group | X | Total: 36 Core: 12 Support: 24 | 40 × group sessions (min NR) | 24 × group sessions (min NR) | 40 | Research clinic | NR | Multi-disciplinary team |
| Kulzer, 2009262 (PREDIAS) | IG1 | Group counseling | Group | X | Total: 10 Core: 2 Support: 8 | 8 × group sessions (90 min) | 4 × booster group sessions (90 min) | 12 | NR | No | Diabetes educators or psychologists |
| Kumanyika, 2012328 | IG1 | DPP-based individual counseling | Individual | X | Total: 12 Core: 12 Support: 0 | 4 × PCP counseling sessions (10-15 mins) 12 × individual coaching sessions (10-15 mins) | 17 | Primary care | Yes | PCP and lifestyle coaches | |
| Little, 2016264 | IG1 | POWeR+ web-based intervention plus individual counseling | Tech | X | Total: 6 Core: 6 Support: 0 | 24 × web-based sessions (min NR) 3 × individual counseling sessions (min NR) 4 × optional individual counseling sessions (min NR) | 31 | Home (web-based) and research clinic | No | Research nurse | |
| IG2 | POWeR+ web-based intervention plus telephone or email counseling | Tech | Total: 6 Core: 6 Support: 0 | 24 × web-based sessions (min NR) 3 × phone or email contacts (min NR) 2 × optional phone or email contacts (min NR) | 29 | Home (web-based) | No | Research nurse | |||
| Logue, 2005324 (REACH) | IG1 | Individual and telephone counseling plus personalized mailings | Individual+Phone | X | Total: 24 Core: 24 Support: 0 | 4 × individual sessions (10 min) 24 × phone calls (15 min) | 14 | Primary care and home | Yes | Dietitians, weight loss advisors, PCPs | |
| Luley, 2014265 | IG1 | Self-monitoring via accelero-meter and 4Sigma telephone counseling | Phone with tech support | Total: 12 Core: 12 Support: 0 | 12 × telephone calls (20 min) | 12 | Home (web-based) | No | Doctor and nurse | ||
| IG2 | Self-monitoring via accelero-meter and Active Body Control tailored print materials | Tech | Total: 12 Core: 12 Support: 0 | 52 × weekly tailored mailed reports | 0 | Home (web-based) | NR | Carer | |||
| Ma, 2013266 (E-LITE) | IG1 | DPP-based group counseling | Group | X | Total: 15 Core: 3 Support: 12 | 12 × group sessions (90-120 min) including supervised PA (30-45 min) | Email contact every 2-4 weeks plus web-based self-monitoring | 12 | Primary care | NR | E-LITE lifestyle coach (registered dietitian) |
| IG2 | DPP-based DVD coaching (Group Lifestyle Balance) | Tech | Total: 15 Core: 3 Support: 12 | 1 × group orientation session (min NR) 12 × weekly sessions delivered via DVD (min NR) | Email contact every 2-4 weeks plus web-based self-monitoring | 12 | Home (DVD-based) | NR | E-LITE lifestyle coach (registered dietitian) | ||
| Marrero, 2016267 | IG1 | Weight Watchers | Group | X | Total: 12 Core: 12 Support: 0 | Free access to weekly Weight Watchers group counseling sessions | 52 | Community | No | Weight Watchers group leader | |
| Martin, 2008269 | IG1 | Individual PCP counseling | Individual | X | Total: 6 Core: 6 Support: 0 | 6 × individual sessions (15 min) | 6 | Primary care | Yes | PCP | |
| Mensink, 2003325 (SLIM) | IG1 | Individual counseling | Individual | X | Total: 24 Core: 24 Support: 0 | 11 × individual sessions (min NR) | 6 | NR | No | Dieticians, exercise trainers | |
| Mitsui, 2008270 | IG1 | Group-based education plus exercise training | Group | X | Total: 12 Core: 12 Support: 0 | 25 × group sessions (min NR) | 25 | Community | NR | Dietitian | |
| Moore, 2003271 | IG1 | PCP training | Individual | X | Total: 12 Core: 12 Support: 0 | Providers: 3 × group training sessions (90 min) Patients: Average of 8 individual sessions (min NR) | 8 | Primary care | Yes | Dietitian | |
| Morgan, 2011272 (SHED-IT) | IG1 | Web-based intervention | Tech | Total: 3 Core: 3 Support: 0 | 1 × information session (75-min) plus web-based self-monitoring program | 1 | Home (web-based) | NR | Research staff | ||
| Nakade, 2012274 (SCOP) | IG1 | Individual and group counseling | Mixed | X | Total: 12 Core: 12 Support: 0 | 5 × individual sessions (30 min) 5 × group sessions (20 min) | 5 | Community health center | NR | Dietitian and exercise instructors | |
| Nanchahal, 2012275 (CAMWEL) | IG1 | Individual counseling | Individual | X | Total: 9 Core: 9 Support: 0 | 14 × individual sessions (30 min) | 14 | Primary care | No | Research staff | |
| Narayan, 1998276 | IG1 | Group counseling (Pima Action) | Group | X | Total: 12 Core: 12 Support: 0 | 52 × group sessions (min NR) Optional home visits | 52 | NR | NR | Research staff and dietitian | |
| Nicklas, 2014277 (Balance after Baby) | IG1 | Web-based intervention plus telephone counseling | Tech | Total: 12 Core: 12 Support: 0 | 12-18 × web-based module sessions (min NR) 24 × phone/email sessions (min NR) | 36 | Home (web-based) | No | Registered dietitian | ||
| Nilsen, 2011327 | IG1 | Group counseling | Group | X | Total: 18 Core: 5 Support: 13 | 1 × individual sessions (30 mins) 7 × group sessions (300 mins) | 3 × individual consults with PCP @ NR mins | 10 | Research clinic | Yes | Physician, nurse, dietician, physio-therapist, and ergonomist |
| O’Brien, 2017321 (PREVENT-DM) | IG1 | Group counseling | Group | X | Total: 12 Core: 12 Support: 0 | 24 × group sessions (90 mins) | 24 | Community health center | No | Community health workers | |
| Ockene, 2012278 (LLDPP) | IG1 | Group and individual counseling | Mixed | X | Total: 12 Core: 12 Support: 0 | 1 × individual session (60 min) 2 × individual sessions (30 min) 1 × group session (90 min) 12 × group sessions (60 min) | 16 | Home and senior community center | No | Community intervent-ionist | |
| Pacanowski, 2015279 | IG1 | Web-based self-monitoring (Caloric Titration Method) | Tech | Total: 12 Core: 12 Support: 0 | 1 × educational presentation (min NR) plus daily self-weighing and monitoring via website | 1 | Home (web-based) | NR | NA | ||
| Parikh, 2010280 (HEED) | IG1 | Peer-led group counseling | Group | X | Total: 2.5 Core: 2.5 Support: 0 | 8 × group sessions (90 min) | 8 | Community | No | Community leaders and peers | |
| Patrick, 2011281 | IG1 | Web-based intervention | Tech | Total: 12 Core: 12 Support: 0 | 52 × web sessions and tailored feedback (min NR) | 52 | Home (web-based) | NR | NA | ||
| Penn, 2009283 (EDIPS-Newcastle) | IG1 | Individual counseling | Individual | X | Total: 60 Core: 60 Support: 0 | 23 × individual sessions (30 min) Optional group sessions (# of sessions and min NR) | 7 | NR | No | Dietitian and physio-therapist | |
| Phelan, 2017330 | IG1 | Web-based self-monitoring and feedback plus in-person group counseling | Mixed | X | Total: 12 Core: 12 Support: 0 | 12 × group sessions (60 mins) 4 × text messages/week 52 × weekly web sessions | 12 | WIC clinic and home | No | Dietitians, WIC program staff, study intervent-ionists | |
| Puhkala, 2015286 | IG1 | Individual and telephone counseling (LIFE) | Individual + Phone | X | Total: 12 Core: 12 Support: 0 | 5 × individual sessions (60 min) 7 × phone sessions (30 min) | 13 | NR | No | Nutritionist and physio-therapist | |
| Rock, 2007289 | IG1 | Referral and free access to Jenny Craig | Individual | X | Total:12 Core:12 Support: 0 | 52 × individual sessions (min NR) | 52 | Community | NR | Dietitian and Jenny Craig consultants | |
| Rock, 2015288 (ENERGY) | IG1 | Group counseling with telephone and email support | Mixed | X | Total: 24 Core: 6 Support: 18 | 20 × group sessions (60 min) plus 14- 16 calls or emails | 6 × group sessions (60 min) plus 24-38 calls or emails | 42 | Research clinic | NR | Dietitian, psychologist, and exercise physiologist |
| Rodriguez-Cristobal, 2017329 (IMOAP) | IG1 | Group counseling | Group | X | Total: 24 Core: 6 Support: 18 | 4 × PCP visits (min NR) 12 × group sessions (60 mins) | 4 × PCP visits (min NR) 20 × group sessions (60 mins) | 32 | Primary care | No | Research nurse |
| Rosas, 2015290 (VAFO) | IG1 | DPP-based group and individual counseling (case management) | Mixed | X | Total: 24 Core: 12 Support: 12 | 12 × group sessions (120 min) 4 × individual sessions (30 min) | 3 × group sessions (120 min) 1 × individual session (30 min) | 18 | Community health center | NR | Research staff |
| IG2 | DPP-based group and individual counseling (case management + community health worker support) | Mixed | X | Total: 24 Core:12 Support: 12 | 12 × group sessions (120 min) 4 × individual sessions (30 min) 5 × CHW home visits (min NR) | 3 × group sessions (120 min) 1 × individual session (30 min) 2 × CHW home visits (min NR) | 23 | Community health center, home | No | Research staff & community health workers | |
| Ross, 2012291 (PROACTIVE) | IG1 | Individual counseling (Motivational interviewing) | Individual | X | Total: 24 Core: 6 Support: 18 | 15 × individual sessions (60 min) | 6 × individual sessions (60 min) (months 7-12) 12 × individual sessions (30-60 min) (months 12-24) | 21 | Primary care | NR | Health educator |
| Shapiro, 2012293 (Text4Diet) | IG1 | Text messages | Tech | Total: 12 Core: 12 Support: 0 | 4 × text messages/day | 0 | Home (text-based) | NR | NA | ||
| Silva, 2009295 | IG1 | Group counseling | Group | X | Total: 12 Core: 12 Support: 0 | 30 × group sessions (120 min) | 30 | University | NR | Exercise physiologist, nutritionist, dietitian, and psychologist | |
| Stevens, 1993300 (TOHP I) | IG1 | Group counseling | Group | X | Total: 18 Core: 4 Support: 14 | 1 × individual session (min NR) 14 × weekly group sessions (90 min) | 15 × monthly group sessions with optional individual check-ins (min NR) | 23 | NR | No | Registered dietitian and psychologist or exercise psychologist |
| Stevens, 2001301 (TOHP II) | IG1 | Group counseling | Group | X | Total: 36 Core: 4 Support: 32 | 1 × individual session (min NR) 14 × weekly group sessions (90 min) | 6 × biweekly group sessions (90 min) (months 5-17) 3-6 × “Minimodules”/refresher courses consisting of up to 6 sessions each (min NR) Participant-initiated individual counseling | 27 | NR | No | Dietitian and health educator |
| Svetkey, 2015302 (CITY) | IG1 | Group counseling, telephone support, and self-monitoring through smartphone (personal coach) | Mixed | X | Total: 24 Core: 24 Support: 0 | 6 × weekly group sessions (120 min) 22 × monthly calls (20 min) | 16 | NR | NR | Research staff | |
| IG2 | Smartphone-based self-monitoring | Tech | Total: 24 Core: 24 Support: 0 | NR × smartphone app prompts | 0 | Home (smartphone-based) | No | NA | |||
| Thomas, 2017322 | IG1 | Weight Watchers Online plus activity tracker | Tech | Total: 12 Core: 12 Support: 0 | Access to Weight Watchers online plus activity tracker | 0 | Home (web-based) | No | NA | ||
| IG2 | Weight Watchers Online | Tech | Total: 12 Core: 12 Support: 0 | Access to Weight Watchers online | 0 | Home (web-based) | No | NA | |||
| Tsai, 2010305 | IG1 | Primary care-based individual counseling | Individual | X | Total: 12 Core: 12 Support: 0 | 4 × brief PCP sessions (2-3 min) 8 × individual sessions with MA (15-20 min) | 12 | Primary care | Yes | Medical assistant and PCP | |
| Tuomilehto, 2001306 (Finnish DPS) | IG1 | Individual counseling plus optional PA and group sessions | Individual | X | Total: 48 Core: 12 Support: 36 | 7 × individual sessions (30-60 min) Optional supervised exercise sessions 2x per week Optional group sessions, expert lessons, phone calls | 12 × individual counseling sessions (every 3 months) (30-60 min) Optional supervised exercise sessions 2x per week Optional group sessions, expert lessons, phone calls | 7 | Research center | No | Nutritionist |
| van Wier, 2011308 (ALIFE@ WORK) | IG1 | Web-based intervention | Tech | Total: 6 Core: 6 Support: 0 | 10 × web-based sessions plus followup emails w/counselors | 10 | Home (web-based) | NR | Dietitian and physical activity scientists | ||
| IG2 | Workbook- and telephone-based counseling | Phone | Total: 6 Core: 6 Support: 0 | 10 workbook modules plus followup phone calls w/counselors | 10 | Home (print- and telephone-based) | No | Dietitian and physical activity scientists | |||
| von Gruenigen, 2012310 (SUCCEED) | IG1 | Group and individual counseling | Mixed | X | Total: 12 Core: 12 Support: 0 | 16 × group sessions (60 mins) (months 1-6) 3 × PCP sessions (min NR) (months 1-12) Print, telephone, and email support (months 7-12) | 19 | NR | Yes | Psychologist, registered dietitian, physical therapist, PCP | |
| Wadden, 2011206 (POWER-UP) | IG1 | Individual counseling | Individual | X | Total: 24 Core: 24 Support: 0 | 8 × individual sessions with PCP (5-7 min) 24 × individual sessions with lifestyle coach (10-15 min) | 16 | Primary care | Yes | Medical assistant and PCP | |
| Whelton, 1998326 (TONE) | IG1 | Group and individual counseling | Mixed | X | Total: 28 Core: 7 Support: 21 | Intensive phase: 12 × group sessions (3 per month; min NR) 4 × monthly individual sessions (min NR) Extended phase: 6 × biweekly group sessions (min NR) | Maintenance phase: 21 × monthly group sessions (min NR) | 22 | University research center | No | Nutritionists, exercise counselors |
| Wing, 1998314 | IG1 | Group counseling (diet and PA focus) | Group | X | Total: 24 Core: 12 Support: 12 | 39 × group sessions (min NR) | Two 6-week refresher courses | 39 | NR | NR | Behavior therapist, registered dietitian, exercise physiologist |
| IG2 | Group counseling (diet focus) | Group | X | Total: 24 Core: 12 Support: 12 | 39 × group sessions (min NR) | Two 6-week refresher courses | 39 | NR | No | Behavior therapist, registered dietitian | |
| IG3 | Group counseling (PA focus) | Group | X | Total: 24 Core: 12 Support: 0 | 39 × group sessions (min NR) | Two 6-week refresher courses | 39 | NR | No | Behavior therapist, exercise physiologist | |
| Wylie-Rosett, 2001315 | IG1 | Computer-based program plus individual and group counseling | Mixed | X | Total: 12 Core: 12 Support: 0 | 21 × computer sessions (30 min) 6 × group sessions (min NR) 18 × phone/face-to-face sessions (min NR) | 45 | Home (web-based) and research center | NR | Dietitian and cognitive behavioral therapist | |
| IG2 | Computer-based intervention | Tech | Total: 12 Core: 12 Support: 0 | 21 × computer sessions (30 min) | 21 | Home (web-based) | NR | NA | |||
| Yeh, 2016316 | IG1 | DPP-based group counseling | Group | X | Total: 12 Core: 6 Support: 6 | 12 × biweekly group sessions (90-120 min) | 6 × followup group sessions (90-120 min) | 18 | Community | No | Lifestyle coach |
Abbreviations: 10TT = Ten Top Tips; ADAPT = Activity, Diet and Blood Pressure Trial; CAMWEL = Camden Weight Loss; CHARMS = Community Health and Risk-reduction for Metabolic Syndrome; CHW = community health worker; CITY = Cell Phone Intervention for You; DAMES = Daughters And Mothers Against Breast Cancer; DEPLOY = Diabetes Education & Prevention with a Lifestyle Intervention offered at the YMCA; DPP = Diabetes Prevention Program; DPS = Diabetes Prevention Study; EDIPS = European Diabetes Prevention Study; E-LITE = Evaluation of Lifestyle Interventions to Treat Elevated Cardiometabolic Risk in Primary Care; ENERGY = Exercise and Nutrition to Enhance Recovery and Good Health for You; FFIT = Football Fans in Training; FU = followup; HEED = Project Help Educate to Eliminate Diabetes; HELP PD = Healthy Partnerships to Prevent Diabetes; HOT = Hypertension Optimal Treatment; IG = intervention group; IMOAP = Group motivational intervention in overweight/obese patients in primary prevention of cardiovascular disease in the primary healthcare area; LLDPP = Lawrence Latino Diabetes Prevention Project; min = minutes; mos = months; NA = not applicable; NHS = National Health Service (UK); NR = not reported; ORBIT = Obesity Reduction Black Intervention; PA = physical activity; PCP = primary care provider; PODOSA = Prevention of Diabetes and Obesity in South Asians; POWER = Practice Based Opportunities for Weight Reduction; POWER-UP = Practice-based Opportunities for Weight Reduction at the University of Pennsylvania; PREDIAS = Prevention of Diabetes Self-Management Program; PROACTIVE = Prevention and Reduction of Obesity through Active Learning; PREVENT-DM = The Promotora Effectiveness Versus Metformin Trial; REACH = Reasonable Eating and Activity to Change Health; PROOF = Prevention of Knee Osteoarthritis in Overweight Females; RAPID-YDPP = Reaching Out to Prevent Increases in Diabetes - YMCA model for Diabetes Prevention Program; REACH = Reasonable Eating and Activity to Change Health; SCOP = Saku Control Obesity Program; SHED-IT = Self-Help, Exercise, and Diet using Information Technology; SLIM = Study on lifestyle-intervention and impaired glucose tolerance Maastricht; SMART = Social Mobile Approaches to Reduce weighT; SUCCEED = Survivors of Uterine Cancer Empowered by Exercise and Healthy Diet; Tech = technology-based; TOHP = Trials of Hypertension Prevention Phase; TONE = Group motivational intervention in overweight/obese patients in primary prevention of cardiovascular disease in the primary healthcare area; VAFO = Vivamos Activos Fair Oaks; WOMAN = Women on the Move through Activity and Nutrition; YMCA = The Young Men’s Christian Association; WRAP = Weight-loss programme referrals for adults in primary care
Table 5Behavior-Based Weight Loss Intervention Components
| Author, year | Arm | Main mode of int delivery | In-person contact | Group sess | Individual sess | Tech | DPP-based | Commercial program | MI | PA sess | Weight loss goal set | Addressed barriers | Addressed pros and cons | Active use of self-monitoring | Involved spouse or family |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ackermann, 2008214 | IG1 | Group | X | X | X | X | X | X | X | ||||||
| Ackermann, 2015215 | IG1 | Group | X | X | X | X | X | ||||||||
| Ahern, 2017323 | IG1 | Group | X | X | X | ||||||||||
| IG2 | Group | X | X | X | |||||||||||
| Anderson, 2014217 | IG1 | Individual + Phone | X | X | X | X | X | X | |||||||
| Appel, 2011219 | IG1 | Mixed | X | X | X | X | X | X | X | X | X | ||||
| IG2 | Phone with tech support | X | X | X | X | X | |||||||||
| Aveyard, 2016221 | IG1 | Group | X | X | X | X | X | X | X | ||||||
| Beeken, 2017318 | IG1 | Individual | X | X | X | ||||||||||
| Bennett, 2012224 | IG1 | Phone with tech support | X | X | X | X | X | X | |||||||
| Bhopal, 2014225 | IG1 | Individual | X | X | X | X | X | X | |||||||
| Burke, 2005228 | IG1 | Mixed | X | X | X | X | X | X | |||||||
| Cadmus-Bertram, 2016229 | IG1 | Phone with tech support | X | X | X | ||||||||||
| Chirionos, 2016230 | IG1 | Group | X | X | X | X | X | ||||||||
| Christian, 2011231 | IG1 | Tech | X | X | X | X | X | X | X | X | |||||
| Cohen, 1991232 | IG1 | Individual | X | X | X | ||||||||||
| de Vos, 2015234 | IG1 | Individual | X | X | X | X | X | X | X | X | |||||
| Demark-Wahnefried, 2014235 | IG1 | X | X | X | X | X | |||||||||
| IG2 | X | X | X | X | X | ||||||||||
| Eaton, 2016237 | IG1 | Individual + Phone | X | X | X | X | X | X | |||||||
| Fischer, 2016319 | IG1 | Tech | X | X | X | X | X | ||||||||
| Fitzgibbon, 2010240 | IG1 | Mixed | X | X | X | X | X | X | X | X | X | ||||
| Godino, 2016242 | IG1 | Tech | X | X | X | X | |||||||||
| Greaves, 2015243 | IG1 | Group | X | X | X | X | X | X | X | ||||||
| Haapala, 2009245 | IG1 | Tech | X | X | X | ||||||||||
| Hunt, 2014249 | IG1 | Group | X | X | X | X | X | X | |||||||
| Huseinovic, 2016250 | IG1 | Phone | X | X | X | X | |||||||||
| Jakicic, 2011251 | IG1 | Mixed | X | X | X | X | X | ||||||||
| IG2 | Mixed | X | X | X | X | X | |||||||||
| Jansson, 2013252 | IG1 | Individual + Phone | X | X | X | X | |||||||||
| Jebb, 2011253 | IG1 | Group | X | X | X | X | X | X | X | ||||||
| Jeffery, 1993254 | IG1 | Group | X | X | X | X | |||||||||
| IG2 | Group | X | X | X | X | ||||||||||
| IG3 | Group | X | X | X | X | ||||||||||
| IG4 | Group | X | X | X | X | ||||||||||
| Jenkins, 2017320 | IG1 | Phone | X | X | X | X | |||||||||
| IG2 | Phone | X | X | X | X | ||||||||||
| IG3 | Phone | X | |||||||||||||
| Jolly, 2011255 | IG1 | Group | X | X | X | X | X | X | X | ||||||
| IG2 | Group | X | X | X | X | X | X | X | |||||||
| IG3 | Group | X | X | X | X | X | X | X | |||||||
| IG4 | Group | X | X | X | X | X | X | X | |||||||
| IG5 | Individual | X | X | X | X | X | X | ||||||||
| IG6 | Individual | X | X | X | X | X | X | ||||||||
| IG7 | Group | X | X | X | X | X | X | X | X | X | |||||
| Jones, 1999256 | IG1 | Mixed | X | X | X | X | |||||||||
| Kanke, 2015257 | IG1 | Individual | X | X | X | X | X | X | |||||||
| Katula, 2011258 | IG1 | Mixed | X | X | X | X | X | X | X | ||||||
| Knowler, 2002205 | IG1 | Individual | X | X | X | X | X | X | X | X | X | ||||
| Kuller, 2012261 | IG1 | Group | X | X | X | X | X | ||||||||
| Kulzer, 2009262 | IG1 | Group | X | X | X | X | X | X | |||||||
| Kumanyika, 2012328 | IG1 | Individual | X | X | X | X | X | X | X | ||||||
| Little, 2016264 | IG1 | Tech | X | X | X | X | X | X | |||||||
| IG2 | Tech | X | X | X | X | X | X | ||||||||
| Logue, 2005324 | IG1 | Individual+Phone | X | X | X | X | X | ||||||||
| Luley, 2014265 | IG1 | Phone with tech support | X | X | |||||||||||
| IG2 | Tech | X | X | ||||||||||||
| Ma, 2013266 | IG1 | Group | X | X | X | X | X | X | X | X | |||||
| IG2 | Tech | X | X | X | X | X | X | X | |||||||
| Marrero, 2016267 | IG1 | Group | X | X | X | X | X | ||||||||
| Martin, 2008269 | IG1 | Individual | X | X | X | X | |||||||||
| Mensink, 2003325 | IG1 | Individual | X | X | X | X | X | ||||||||
| Mitsui, 2008270 | IG1 | Group | X | X | X | ||||||||||
| Moore, 2003271 | IG1 | Individual | X | X | X | ||||||||||
| Morgan, 2011272 | IG1 | Tech | X | X | X | X | X | X | |||||||
| Nakade, 2012274 | IG1 | Mixed | X | X | X | X | X | X | X | X | |||||
| Nanchahal, 2012275 | IG1 | Individual | X | X | X | X | X | X | |||||||
| Narayan, 1998276 | IG1 | Group | X | X | X | ||||||||||
| Nicklas, 2014277 | IG1 | Tech | X | X | X | X | X | ||||||||
| Nilsen, 2011327 | IG1 | Group | X | X | X | X | X | X | |||||||
| O’Brien, 2017321 | IG1 | Group | X | X | X | X | X | X | X | ||||||
| Ockene, 2012278 | IG1 | Mixed | X | X | X | X | X | X | X | ||||||
| Pacanowski, 2015279 | IG1 | Tech | X | X | X | X | |||||||||
| Parikh, 2010280 | IG1 | Group | X | X | X | X | |||||||||
| Patrick, 2011281 | IG1 | Tech | X | X | X | X | X | ||||||||
| Penn, 2009283 | IG1 | Individual | X | X | X | X | X | X | X | X | |||||
| Phelan, 2017330 | IG1 | Mixed | X | X | X | X | X | X | X | X | |||||
| Puhkala, 2015286 | IG1 | Individual + Phone | X | X | X | X | X | ||||||||
| Rock, 2007289 | IG1 | Individual | X | X | X | X | X | X | X | ||||||
| Rock, 2015288 | IG1 | Mixed | X | X | X | X | X | X | X | ||||||
| Rodriguez-Cristobal, 2017329 | IG1 | Group | X | X | X | X | |||||||||
| Rosas, 2015290 | IG1 | Mixed | X | X | X | X | X | X | X | X | X | ||||
| IG2 | Mixed | X | X | X | X | X | X | X | X | X | |||||
| Ross, 2012291 | IG1 | Individual | X | X | X | X | X | X | X | ||||||
| Shapiro, 2012293 | IG1 | Tech | X | X | X | X | X | ||||||||
| Silva, 2009295 | IG1 | Group | X | X | X | X | X | ||||||||
| Stevens, 1993300 | IG1 | Group | X | X | X | X | X | X | X | X | |||||
| Stevens, 2001301 | IG1 | Group | X | X | X | X | X | X | X | X | |||||
| Svetkey, 2015302 | IG1 | Mixed | X | X | X | X | X | X | X | X | X | ||||
| IG2 | Tech | X | X | X | X | X | X | ||||||||
| Thomas, 2017322 | IG1 | Tech | X | X | X | X | |||||||||
| IG2 | Tech | X | X | X | X | ||||||||||
| Tsai, 2010305 | IG1 | Individual | X | X | X | ||||||||||
| Tuomilehto, 2001306 | IG1 | Individual | X | X | X | X | X | X | X | ||||||
| van Wier, 2011308 | IG1 | Tech | X | X | X | X | X | ||||||||
| IG2 | Phone | X | X | X | X | ||||||||||
| von Gruenigen, 2012310 | IG1 | Mixed | X | X | X | X | X | X | X | ||||||
| Wadden, 2011206 | IG1 | Individual | X | X | X | X | X | X | |||||||
| Whelton, 1998326 | IG1 | Mixed | X | X | X | X | X | X | |||||||
| Wing, 1998314 | IG1 | Group | X | X | X | X | X | X | X | ||||||
| IG2 | Group | X | X | X | X | X | X | ||||||||
| IG3 | Group | X | X | X | X | X | X | X | |||||||
| Wylie-Rosett, 2001315 | IG1 | Mixed | X | X | X | X | X | X | X | X | |||||
| IG2 | Tech | X | X | X | X | X | |||||||||
| Yeh, 2016316 | IG1 | Group | X | X | X | X | X | X |
Abbreviations: DPP = Diabetes Prevention Program; IG = intervention group; int=intervention; MI = motivational interviewing; PA = physical activity; sess=session;Tech = technology-based
Table 6Behavior-Based Weight Loss Maintenance Intervention Characteristics (k=9, 15 intervention arms)
| Author, year (Study name) | Arm | Brief description | Main mode of delivery | In-person support | Duration (mos) | Weight loss phase components | Maintenance components | Total # of sessions in first 12 mos | Setting | PCP involved? | Provider |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cussler, 2008233 (HW4L) | IG1 | Web-based monitoring and support | Tech | 12 | Weekly group meetings (150 min/session) for 4 months Required weight loss to enter maintenance: None | 2 × website orientation sessions (60 min) and ongoing online support groups | 2 | NR | No | NR | |
| Pekkarinen, 2015282 | IG1 | Group counseling | Group | X | 12 | Week 2-11 included VLCDD followed by a 2-week refeeding phase. 15 weekly group sessions (1.5 hours) during 17-week weight loss phase. Required weight loss to enter maintenance: None | 12 × group sessions (90 min) | 12 | Outpatient obesity research clinic | NR | Nutritionist, nurse, and physiotherapist |
| Perri, 1988284 | IG1 | Group counseling plus social influence and increased physical activity | Group | X | 12 | Weekly 2-hour weekly group sessions for 20 weeks. Required weight loss to enter maintenance: None | 26 × group sessions (120 min) | 26 | NR | Yes | Clinical psychologist paired with physician or nurse practitioner |
| IG2 | Group counseling plus increased physical activity | Group | X | 12 | Weekly 2-hour weekly group sessions for 20 weeks. Required weight loss to enter maintenance: None | 26 × group sessions (120 min) | 26 | NR | Yes | Clinical psychologist paired with physician or nurse practitioner | |
| IG3 | Group counseling plus social influence program | Group | X | 12 | Weekly 2-hour weekly group sessions for 20 weeks. Required weight loss to enter maintenance: None | 26 × group sessions (120 min) | 26 | NR | Yes | Clinical psychologist paired with physician or nurse practitioner | |
| IG4 | Group counseling | Group | X | 12 | Weekly 2-hour weekly group sessions for 20 weeks. Required weight loss to enter maintenance: None | 26 × group sessions (120 min) | 26 | NR | Yes | Clinical psychologist paired with physician or nurse practitioner | |
| Sherwood, 2013294 (Keep It Off) | IG1 | Telephone-based counseling | Phone | No WL intervention given. Required weight loss to enter maintenance: ≥10% WL in past year | 10 × telephone calls (20 min) 14 × telephone calls (15 min) | 24 | Home | NR | NR | ||
| Simpson, 2015296 (WILMA) | IG1 | Individual counseling | Individual + Phone | X | 12 | No WL intervention given. Required weight loss to enter maintenance: ≥5% WL in past year | 6 × individual MI sessions (60 min) 9 × telephone counseling sessions (20 min) | 15 | NR | NR | Motivational interviewing practitioner |
| IG2 | Individual counseling | Individual + Phone | X | 12 | No WL intervention given. Required weight loss to enter maintenance: ≥5% WL in past year | Two individual sessions (length NR) followed by 2 phone sessions (~20 minutes) (about 6 months apart). | 4 | NR | NR | Motivational interviewing practitioner | |
| Svetkey, 2008303 (WLM) | IG1 | Individual and telephone counseling | Individual + Phone | X | 60 | Weekly group sessions (1.5-2 hours) over approximately 6 months (20 total). Required weight loss to enter maintenance: ≥4 kg during WL phase | Maintenance, phase 1: 23 × phone sessions (5-15 min) 7 × individual sessions (45-60 min) Maintenance, phase 2: Continued contact group only: 4 × group sessions (min NR) 26 × phone sessions (5-15 min) | 12 | NR | No | Research interventionist |
| IG2 | Web-based monitoring | Tech | 30 | Weekly group sessions (1.5-2 hours) over approximately 6 months (20 total). Required weight loss to enter maintenance: ≥4 kg during WL phase | No sessions. Web-based monitoring only. | 0 | NR | No | NA | ||
| Voils, 2017309 | IG1 | Group and individual counseling | Mixed | X | 10 | Biweekly group meetings for 16 weeks (8 sessions total). Required weight loss to enter maintenance: ≥4 kg during WL phase | 3 × group sessions (min NR) 8 × individual phone sessions (min NR) | 11 | University campus & home | No | Registered dietitian |
| Wing, 2006313 (STOP) | IG1 | Group counseling | Group | X | 18 | No WL intervention given. Required weight loss to enter maintenance: ≥10% WL in past 2 years | 4 × weekly meetings (min NR) 17 × monthly meetings (min NR) | 15 | Hospital clinic | NR | Nutritionist, exercise physiologist, and clinical psychologist |
| IG2 | Web-based intervention | Tech | 18 | No WL intervention given. Required weight loss to enter maintenance: ≥10% WL in past 2 years | 1 × introductory session (min NR) 4 × weekly chat-room meetings (min NR) 17 × monthly chat-room meetings (min NR) | 16 | Internet | NR | Nutritionist, exercise physiologist, and clinical psychologist | ||
| Young, 2017317 | IG1 | Web-based intervention | Tech | 6 | Self-administered weight loss program (DVD, logbooks, and motivational messaging). Required weight loss to enter maintenance: ≥4kg during WL phase | Web-based self-monitoring program (min NA) | 0 | Home (web-based) | NR | Research staff |
Abbreviations: HW4L = Healthy Weight for Life; IG = intervention group; kg = kilograms; min = minute(s); mos = months; NA = not applicable; NR = not reported; PCP = primary care provider; STOP = Study to Prevent Regain; Tech = technology-based; WILMA = Weight Loss Maintenance in Adults; WL = weight loss; WLM = Weight Loss Maintenance
Table 7Behavior-Based Weight Loss Maintenance Intervention Components
| Author, year | Arm | Main mode of int delivery | In-person contact | Group sessions | Individual sessions | Tech-based | DPP-based | Commercial program | MI | PA sessions | Weight loss goal set | Addressed barriers | Addressed pros and cons | Active use of self-monitoring | Involved spouse or family |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cussler, 2008233 | IG1 | Tech | X | X | |||||||||||
| Pekkarinen, 2015282 | IG1 | Group | X | X | X | X | X | X | X | ||||||
| Perri, 1988284 | IG1 | Group | X | X | X | X | X | X | X | ||||||
| IG2 | Group | X | X | X | X | X | |||||||||
| IG3 | Group | X | X | X | X | X | X | ||||||||
| IG4 | Group | X | X | X | X | ||||||||||
| Sherwood, 2013294 | IG1 | Phone | X | X | X | X | |||||||||
| Simpson, 2015296 | IG1 | Individual + Phone | X | X | X | X | X | X | |||||||
| IG2 | Individual + Phone | X | X | X | X | X | |||||||||
| Svetkey, 2008303 | IG1 | Individual + Phone | X | X | X | X | X | X | X | ||||||
| IG2 | Tech | X | X | X | X | X | |||||||||
| Voils, 2017309 | IG1 | Mixed | X | X | X | X | X | X | X | ||||||
| Wing, 2006313 | IG1 | Group | X | X | X | X | X | X | X | ||||||
| IG2 | Tech | X | X | X | X | X | X | X | |||||||
| Young, 2017317 | IG1 | Tech | X | X | X | X |
Abbreviations: DPP = Diabetes Prevention Program; MI = motivational interviewing; PA = physical activity; Tech = technology-based
Table 8Medication-Based Intervention Characteristics (k= 35, 41 arms)
| Drug | Author, year (Study name) | Run-in (weeks) | Duration (mos) | Dosage | Behavioral intervention | Weighing frequency | Adherence |
|---|---|---|---|---|---|---|---|
| Liraglutide | Astrup, 2012220 | 2 | 12 | 3.0mg QD | Prescribed 500 kcal/day deficit diet. Encouraged to maintain or increase physical activity. Advised on diet and physical activity through treatment. Pedometers provided, food diaries collected quarterly for review by dietician. | Weekly during dose escalation (initial 4 weeks) followed by once/month | Adherence: NR Completing study on drug: IG: 70.0% CG: 63.3% |
| Kim, 2013259* | NA | 3.5 | 1.8mg QD | Prescribed 500 kcal/day deficit diet with individualized meal plan. Food diaries kept throughout study. Advised to maintain baseline physical activity. | Weekly over 1st month, then bimonthly | Adherence: NR Completing study on drug: IG: 68.6% CG: 81.8% | |
| Pi-Sunyer, 2015285 le Roux, 2017339 (SCALE Obesity and Prediabetes) | NA | 13 (36 months for individuals with prediabetes) | 3.0mg QD | Prescribed 500 kcal/day deficit diet and advised in increase physical activity to 150 min/week. Counseling on lifestyle modification in individual or group setting. Food diaries assessed every 2 months. | Evaluated every 2 weeks until week 8 and then evaluated every 4 weeks until week 44, then evaluated at weeks 50, 56, 58, 60, 64, 68 and 70; prediabetes subgroup at 160 and 172 weeks | Adherence: NR Completing study on drug: IG: 71.9% CG: 64.4% Completing study on drug (36 months, prediabetes): IG: 52.6% CG:45.0% | |
| Wadden, 2013312† (SCALE Maintenance) | 4-12 | 13 | 3.0mg QD | Prescribed 500 kcal/day deficit diet. Encouraged to exercise 150 min/week with pedometer. 15-20 minute counseling sessions every 4 weeks. | Every week during drug escalation then every 4 weeks. Week 0, 1, 2, 3, 4, 6, 10, 14, 18, 22, 26, 30, 34, 38, 42, 46, 52. | Adherence: NR Completing study on drug: IG: 75.0% CG: 69.5% | |
| Lorcaserin hydrochloride | Farr, 2016238* | 1 | 10mg BID | Weeks 1, 2, and 4 | Adherence: NR Completing study on drug: IG: 70.8% CG: 79.2% | ||
| Fidler, 2011173 (BLOSSOM) | NA | 12 | 10mg BID | Prescribed 600 kcal/day deficit diet. Advised to exercise 30 min/day. Nutritional and physical activity counseling provided monthly. Food diaries used as motivational tools but not formally analyzed. | Weeks 2 and 4 and monthly thereafter through week 52 | Adherence: IG received drug for an average of 257 (SD=139) out of 365 days (CG: 242 [SD=143]). Completing study on drug: IG: 57.2% CG: 52.0% | |
| Martin, 2011268* | 1 | 2 | 10mg BID | Prescribed 600 kcal/day deficit diet by dietician. Prescribed exercise plan to contribute to 600 kcal/day deficit. | Weekly clinic visits | Adherence: NR Completing study on drug: IG: 93.1% CG: 89.3% | |
| Smith, 2010172 (BLOOM) | NA | 12 | 10mg BID | Prescribed 600 kcal/day deficit diet. Encouraged to exercise moderately for 30 min/day. Standard nutritional and physical activity counseling. | 2 & 4 weeks, then on a monthly basis | Adherence: NR Completing study on drug: IG: 55.4% CG: 45.1% | |
| Naltrexone HCL and bupropion HCL | Apovian, 2013218 (COR-11) | NA | 13 | 16/180mg TID | Prescribed 500 kcal/day deficit diet. Advised to increase physical activity. Behavior modification advice every 12 weeks. | Every 4 weeks | Adherence: NR Completing study on drug: IG: 53.7% CG: 53.9% |
| Greenway, 2010244 (COR-1) | NA | 13 | 16/180mg TID | Prescribed 500 kcal/day deficit diet and advised to increase physical activity. | Every 4 weeks | Adherence: NR Completing study on drug: IG: 50.8% CG: 49.9% | |
| Wadden, 2011 (Med)311 (COR-BMOD) | NA | 13 | 16/180mg TID | Prescribed 1,200 kcal/day diet to 1,500 kcal/day diet based on baseline weight and health. Encouraged to increase physical activity to 180 min/week (first 6 months) up to 360 min/week. Received 28 90-min group behavioral counseling sessions. | Every 4 weeks | Adherence: Attended mean 18.7 sessions (SD=6.8) BMOD sessions out of 28 (CG: 17.5 [SD=7.3]). Completing study on drug: IG: 57.9% CG: 58.4% | |
| Orlistat | Acharya, 2006213* | NA | 5 (median) | NR | NR | NR | Adherence: NR Completing study on drug: NA |
| Bakris, 2002222* (Orlistat and Resistant Hypertension) | NA | 12 | 120mg TID | Prescribed 600 kcal/day deficit diet. Encouraged to participate in moderate physical activity. Periodic meetings with dieticians to review food diaries. | 11 visits over 52 weeks | Adherence: NR Completing study on drug: IG: 57.6% CG: 38.4% | |
| Broom, 2002226* (Orlistat UK Study) | NA | 6 | 120mg TID | Prescribed 600 kcal/day deficit diet. Dietary and physical activity advice provided by dietician. | Every 4 weeks | Adherence: NR Completing study on drug: IG: 67.6% CG: 84.5% | |
| Broom, 2002227 (UK Multimorbidity Study) | 2 | 12 | 120mg TID | Prescribed 600 kcal/day deficit diet, reduced additional 300 kcal/day at 6 months. | 12 times over 12 months | Adherence: NR Completing study on drug: IG: 70.2% CG: 60.5% | |
| Davidson, 1999160 | 4 | 12 | 120mg TID | 4 behavioral modifications sessions with dietician. Prescribed 500-800 kcal/day deficit diet using food diaries. Encouraged to exercise 20-30 minutes 3-5 times/week. | 17 times in 1 year (including final) | Adherence: NR Completing study on drug: IG: 68.6% CG: 59.4% | |
| Derosa, 2003236 | 4 | 12 | 120mg TID | Prescribed 1500 kcal/day deficit diet with 30 minutes of bicycle exercise 4 days/week. Behavioral modification sessions with dietician every 3 months with food and exercise dairy assessment. | 2 times (including final) | Adherence: NR Completing study on drug: NR | |
| Finer, 2000239 | 4 | 12 | 120mg TID | Prescribed 600 kcal/day deficit diet (minimum 1200 kcal/day). Reduction of additional 300 kcal/day after 24 weeks. | 15 times over 12 months | Adherence: NR Completing study on drug: IG: 64.0% CG: 57.9% | |
| Hauptman, 2000246 | 4 | 12 | 120mg TID | Year 1 (Weight loss): Dietary guidance from study physician, viewed 4 behavioral modification videos. Prescribed 1200-1500 kcal/day diet. Encouraged brisk walking 20-30 minutes 3-5 days/week. Year 2 (Maintenance): Diet increased by 300 kcal/day. | Every 2 weeks for the first month, every 4 weeks until week 52, and every 8 weeks in the second year. | Adherence: NR Completing study on drug: 12 months: IG1 (360mg): 71.9% IG2 (180mg): 72.3% CG: 57.5% 24 months: IG1 (360mg): 55.7% IG2 (180mg): 56.3% CG: 42.9% | |
| 4 | 24 | 60mg TID | Year 1 (Weight loss): Dietary guidance from study physician, viewed 4 behavioral modification videos. Prescribed 1200-1500 kcal/day diet. Encouraged brisk walking 20-30 minutes 3-5 days/week. Year 2 (Maintenance): Diet increased by 300 kcal/day. | Every 2 weeks for the first month, every 4 weeks until week 52, and every 8 weeks in the second year. | |||
| Hill, 1999247† | 24 | 12 | 120mg TID | Dietary and behavioral counseling for 1 year addressing maintenance of weight loss. Food diaries examined quarterly. | Bi-weekly (month 1), monthly (months 1 to 5) bimonthly (months 6-12) | Adherence: NR Completing study on drug: IG1 (360mg): 69.6% IG2 (180mg): 76.9% CG: 73.4% | |
| 24 | 12 | 60mg TID | Dietary and behavioral counseling for 1 year addressing maintenance of weight loss. Food diaries collected every 3 months. | Bi-weekly (month 1), monthly (months 1 to 5) bimonthly (months 6-12) | |||
| Hong, 2013248* | NA | At least 12 | NR | NA‡ | NA | Adherence: NR Completing study on drug: NA | |
| Krempf, 2003260 | 2 | 18 | 120mg TID | Prescribed tailored weight loss diet with 20% energy reduction with further 10% reductions as needed for weight loss (minimum of 1200 kcal/day). Food diaries collected every 4 months. | 18 over 18 months | Adherence: NR Completing study on drug: IG: 47.1% CG: 44.6% | |
| Lindgarde, 2000263 (Swedish Multimorbidity Study) | 2 | 12 | 120mg TID | Prescribed 600 kcal/day deficit diet, reduced additional 300 kcal/day at 6 months. Encouraged to walk 30 min/day. Monthly dietary counseling, information leaflets, and videotapes provided. | 10 times over 1 year | Adherence: NR Completing study on drug: IG: 83.7% CG: 88.2% | |
| Muls, 2001273* (ObelHyx) | 2 | 6 | 120mg TID | Prescribed 600 kcal/day diet (1200 kcal/day minimum). Dietician assessed dietary compliance at weeks 4, 12, and 24. | Monthly | Adherence: NR Completing study on drug: IG: 87.1% CG: 86.4% | |
| Richelsen, 2007287† | 8 | 36 | 120mg TID | Prescribed 600 kcal/day deficit diet. Advised in increase physical activity. Monthly dietician counseling for 18 months, than every 3 months. Food diaries collected yearly. | Monthly for first 18 months, then 3 month intervals. | Adherence: NR Completing study on drug: NR | |
| Rossner, 2000292 | 4 | 24 | 120mg TID | Year 1: Prescribed 600 kcal/day deficit diet. Monthly advice from dietician with assessment of food diaries. Year 2: Participants who lost ≥3 kg between weeks 40-52 adjusted to 10% energy deficit diet. Advice from dietician every two months. | Every 2 weeks for the first 2 months, monthly from months 3 to 6, then every other month. | Adherence: NR Completing study on drug: 12 months: IG1 (360mg): 74.1% IG2 (180mg): 76.4% CG: 65.0% 24 months: IG1 (360mg): 65.2% IG2 (180mg): 57.9% CG: 56.0% | |
| 4 | 24 | 60mg TID | Year 1: Prescribed 600 kcal/day deficit diet. Monthly advice from dietician with assessment of food diaries. Year 2: Participants who lost ≥3 kg between weeks 40-52 adjusted to 10% energy deficit diet. Advice from dietician every two months. | Every 2 weeks for the first 2 months, monthly from months 3 to 6, then every other month. | |||
| Sjostrom, 1998297 | 4 | 12 | 120mg TID | Prescribed 600 kcal/day deficit diet (minimum 1200 kcal/day). Reduction of additional 300 kcal/day after 24 weeks (minimum 1000 kcal/day). | 15 times | Adherence: NR Completing study on drug: IG: 82.3% CG: 75.8% | |
| Smith, 2011298* | NA | 6 | 120mg TID | Prescribed 500 kcal/day deficit diet. Encouraged to exercise regularly. Received education materials on dietary counseling. | Twice in month 1, then monthly for months 2-6 | Adherence: NR Completing study on drug: IG: 76.9% CG: 66.7% | |
| Smith, 2012299* | NA | 6 | 60mg TID | Attended Weigh-to-Stay program consisting of 3 education sessions (1-2 hours) including information on nutrition from registered dietician, physical activity from physical therapist, and a 30-60 minute private nutrition counseling session with dietician. | Every 4 weeks | Adherence: In ITT population: self-reported med compliance ≤85% each month. >60% of participants reported occasionally consuming less than 3 pills/day (results reported for both CG & IG combined) Completing study on drug: IG: 16.0% CG: 10.0% | |
| Swinburn, 2005304 | 4 | 12 | 120mg TID | Advised by dietician to reduce dietary fat intake to between 25-30% of daily energy intake (about 40 g/day) and get regular moderate-intensity physical activity at least 30 min most days. Food diaries collected at weeks 12 and 52. | 2 clinic visits over 4 weeks (lead-in) and 13 visits over 52 weeks (treatment) | Adherence: NR Completing study on drug: IG: 77.6% CG: 81.1% | |
| Torgerson, 2004161 (XENDOS) | NA | 48 | 120mg TID | Prescribed 800 kcal/day deficit diet (readjusted after 6 months to account for weight loss). Advised to walk at least 1 extra km/day and keep exercise diary. Dietary counseling every 2 weeks for first 6 months, than monthly thereafter. | 16 times over 4 years (4 times 12 months) | Adherence: For ITT population, 93.3% of doses from first dose until termination (CG: 92.8%) Completing study on drug: IG: 51.9% CG: 34.6% | |
| Van Gaal, 1998307* (Orlistat Dose-Ranging Study Group) | 4 | 6 | 120mg TID | Prescribed 600 kcal/day deficit diet (minimum 1200 kcal/day), adjusted if BMI fell below 22 kg/m2 on 2 consecutive visits. Counseling from dietician with food diaries kept 9 times during study period. | Day 15 and 29, and then every 4 weeks (7 times) | Adherence: NR Completing study on drug: IG1 (360 mg): 81.1% IG2 (180 mg): 76.6% CG: 78.4% | |
| 4 | 6 | 60mg TID | Prescribed 600 kcal/day deficit diet (minimum 1200 kcal/day), adjusted if BMI fell below 22 kg/m2 on 2 consecutive visits. Counseling from dietician with food diaries kept 9 times during study period. | Day 15 and 29, and then every 4 weeks (7 times) | |||
| Phentermine-topiramate extended release | Allison, 2012 (EQUIP)216 | NA | 13 | 15/92mg QD | Prescribed 500 kcal/day deficit diet with increased water consumption. Advised in increase physical activity. Received standardized lifestyle counseling based on the LEARN manual. | Monthly | Adherence: NR Completing study on drug: IG: 58.8% CG: 46.9% |
| Aronne, 2013 (EQUATE)168* | NA | 6 | 15/92mg QD | Prescribed 500 kcal/day deficit diet with monitoring by food diaries. Advised to increase physical activity as tolerated. Brief monthly visits to discuss goals, incorporated LEARN manual. | 6 monthly visits | Adherence: NR Completing study on drug: Total for all groups: 65.5% completed a study visits on study drug, NR by arm | |
| NA | 6 | 7.5/46mg QD | 6 monthly visits | ||||
| Gadde, 2011241 (CONQUER/SEQUEL) | NA | 13 (CONQUER) + 12 (SEQUEL) | 15/92mg QD | Advised to follow LEARN guidance with instructions to reduce caloric intake by 500 kcal/day and implement physical activity guidelines. | 13 monthly visits + 12 monthly visits for SEQUEL extension | Adherence: NR Completing study on drug: 13 months: IG1 (15/92mg): 63.8% IG2: 7.5/46mg): 69.1% CG: 56.8% 25 months: IG1 (15/92mg): 24.6 IG2: 7.5/46mg): 25.5% CG: 19.7% | |
| NA | 13 (CONQUER) + 12 (SEQUEL) | 7.5/46mg QD | 13 monthly visits + 12 monthly visits for SEQUEL extension |
- *
Included for harms only
- †
Weight Loss Maintenance study
- ‡
Retrospective data from UK Clinical Practice Research Datalink (CPRD) from 09/1998 to 12/2008
Abbreviations: BID = twice a day; BLOOM = Behavioral Modification and Lorcaserin for Overweight and Obesity Management; BLOSSOM = Behavioral Modification and Lorcaserin Second Study for Obesity Management; BMI = body mass index; CG = control group; COR-1 = Contrave Obesity Research-1; COR-11 = CONTRAVE Obesity Research-II; COR-BMOD = Contrave Obesity Research - Behavior Modification; IG = intervention group; ITT = intention-to-treat; kcal = kilocalorie; km = kilometer; LEARN = Lifestyle, Exercise, Attitude, Relationships, Nutrition; mg = milligram; NA = not applicable; NR = not reported; QD = once a day; ObelHyx = Obesity Linked with Hypercholesterolemia treated with Xenical; SD = standard deviation; TID = three times a day; XENDOS = XENical in the prevention of Diabetes in Obese Subjects
Table 9Results of Behavior-Based Weight Loss and Weight Loss Maintenance Interventions on Health-Related Quality of Life (k=17) (n=7120)
| Author, year (Study name) Quality | FU, mos | IG | IG N | Instrument | IG Mean (SD) BL | IG Mean change (95% CI or SD) | CG N | CG Mean (SD) BL | CG Mean change (95% CI or SD) | Study-reported between-group mean difference (95% CI or SD) |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahern, 2017323 (WRAP) Fair | 12 | IG1 | 504 | EQ5D-3L | 0.793 (0.249) | −0.012 (0.011)* | 197 | 0.786 (0.266) | −0.014 (0.018)* | 0.014 (−0.025 to 0.054); p=0.476 |
| IG2 | 508 | 0.783 (0.249) | 0.009 (0.011)* | 197 | 0.786 (0.266) | −0.014 (0.018)* | 0.029 (−0.011 to 0.069); p=0.150 | |||
| 24 | IG1 | 504 | 0.793 (0.249) | −0.018 (0.011)* | 197 | 0.786 (0.266) | −0.005 (0.018)* | −0.014 (−0.052 to 0.025); p=0.486 | ||
| IG2 | 508 | 0.783 (0.249) | −0.015 (0.012)* | 197 | 0.786 (0.266) | −0.005 (0.018)* | −0.011 (−0.050 to 0.028); p=0.486 | |||
| Appel, 2011219 Rubin, 2013378 (SF-12, EQ-5D) (POWER Hopkins) Good | 24 | IG1 | 100 | SF-12 Mental | 52.16 (9.60) | Mean (SE) −0.50 (0.76) | 88 | 51.06 (8.71) | 0.62 (0.95) | −1.12 (−3.52 to 1.27) |
| SF-12 Physical | 47.06 (8.92) | 2.23 (0.75) | 46.83 (7.95) | −0.29 (0.97) | 2.52 (0.11 to 4.93); p<0.05 | |||||
| EQ-5D VAS | 75.12 (18.95) | 6.14 (1.78) | 73.34 (17.63) | 4.31 (1.77) | 1.83 (−3.07 to 6.74) | |||||
| EQ-5D single index | 0.88 (0.12) | −0.01 (0.01) | 0.87 (0.11) | −0.01 (0.01) | −0.0003 (−0.04 to 0.03) | |||||
| IG2 | 115 | SF-12 Physical | 47.53 (8.42) | 1.16 (0.77) | 46.83(7.95) | −0.29 (0.97) | 1.45 (−0.99 to 3.90) | |||
| SF-12 Mental | 52.53 (7.40) | −1.07 (0.68) | 51.06 (8.71) | 0.62 (0.95) | −1.70 (−3.99 to 0.60) | |||||
| EQ-5D VAS | 76.64 (15.72) | 3.45 (1.53) | 73.34 (17.63) | 4.31 (1.77) | −0.86 (−5.47 to 3.75) | |||||
| EQ-5D single index | 0.88 (0.12) | −0.01 (0.01) | 0.87 (0.11) | −0.01 (0.01) | −0.004 (−0.04 to 0.03) | |||||
| de Vos, 2014234 (PROOF) Fair | 30 | IG1 | 186 | EQ-5D | NR | NR | 180 | NR | NR | NS, NR |
| Demark-Wahnefried, 2014235 (DAMES) Good | 12 | IG1 | 23 | SF-36 Mental | 56.6 (8.2) | −1.9 (−6.0 to 2.2) | 18 | 53.7 (8.5) | 2.4 (−1.0 to 5.8) | p=0.35 |
| IG2 | 23 | 52.1 (11.7) | 0.6 (−3.8 to 5.0) | 18 | 53.7 (8.5) | 2.4 (−1.0 to 5.8) | p=0.46 | |||
| IG1 | 23 | SF-36 Physical | 44.3 (8.3) | 2.2 (−2.1 to 6.5) | 18 | 45.3 (8.5) | 0.9 (−1.4 to 3.2) | p=0.73 | ||
| IG2 | 23 | 44.3 (11.9) | −2.3 (−5.0 to 0.4) | 18 | 45.3 (8.5) | 0.9 (−1.4 to 3.2) | p=0.16 | |||
| Greaves, 2015 (Waist the Waist)243 Fair | 12 | IG1 | 55 | EQ-5D VAS | 77.0 (14.9) | NR | 53 | 76.4 (17.0) | NR | 1.36 (−3.37 to 6.04) |
| Jansson, 2013252 Fair | 12 | IG1 | 45 | SF-36 and EQ-5D | NR | NR | 49 | NR | NR | NS, NR |
| Hunt, 2014249 (FFIT) Good | 12 | IG1 | 316 | SF-36 Mental | 48.9 (10.1) | 1.9 (0.9 to 2.8) | 351 | 48.3 (9.2) | 1.6 (0.8 to 2.4) | 0.50 (−0.62 to 1.62); p=0.3822 |
| SF-36 Physical | 47.0 (7.9) | 2.3 (1.5 to 3.2) | 351 | 47.7 (7.5) | 0.2 (−0.6 to 0.9) | 1.89 (0.89 to 2.90); p=0.0002 | ||||
| Knowler, 2012205† Florez, 2012379 (SF-36 [38 months] & SF-6D [38 months] Ackermann, 2009380 (SF-6D, QWB-SA, SF-6D [12 months], SF-36 [12 months]) (DPP) Good | 12 | IG1 | 1017 | SF-36 Mental | 53.7 (7.6) | −0.70 (8.67) | 1018 | 54.0 (7.4) | −1.16 (8.33) | NR |
| 1017 | SF-36 Physical | 50.6 (6.9) | 1.33 (7.0) | 1018 | 50.4 (7.2) | −0.04 (7.12) | NR | |||
| 38 | IG1 | 1048 | SF-36 Mental | 53.7 (7.6) | NR | 850 | 50.4 (7.2) | NR | 0.29 (0.32) | |
| 1048 | SF-36 Physical | 50.6 (6.9) | NR | 850 | 50.4 (7.2) | NR | 1.57 (0.30); p<0.01 | |||
| 12 | IG1 | 268 | Quality of Well-Being Index (QWB-SA) | 0.7 (0.1) | 0.02 (0.1) | 252 | 0.7 (0.1) | 0.01 (0.1) | NR | |
| 12 | IG1 | 1015 | SF-6D Health utility index | 0.8 (0.1) | 0.0 (0.1) | 1018 | 0.8 (0.1) | −0.01 (0.1) | NR | |
| 38 | IG1 | 1048 | SF-6D Health utility index | 0.8 (0.1) | NR | 850 | 0.8 (0.1) | NR | 0.01 (0.004) p<0.05 | |
| Kulzer, 2009262† (PREDIAS) Fair | 12 | IG1 | 91 | WHO-Five Well-Being Index (WHO-5) | 15.3 (5.1) | 1.4 (3.9) | 91 | 14.3 (4.9) | 0.0 (4.2) | 1.40 (0.22 to 2.58); p=0.101 |
| Nanchahal, 2012275 (CAMWEL) Fair | 12 | IG1 | 103 | EQ-VAS | 47.42 (30.68) | NR | 114 | NR | NR | NS, NR |
| Obesity-related QOL | 48.22 (30.18) | NR | 114 | NR | NR | NS, NR | ||||
| Ockene, 2012278 Fair | 12 | IG1 | 147 | SF-12 | NR | NR | 142 | NR | NR | NR |
| Pekkarinen, 2015282§ Fair | 24 | IG1 | 50 | SF-36 | NR | NR | 38 | NR | NR | NS, NR |
| Rock, 2015288 Demark-Wahnefried, 2015381 (ENERGY) Good | 12 | IG1 | 269 | SF-36 Vitality Subscale | 58.7 (21.35) | NR | 244 | 58.7 | NR | p=0.51 |
| 270 | SF-36 Physical Function Subscale | 80.2 (18.67) | NR | 244 | 79.0 (18.38) | NR | p=0.05 | |||
| 24 | IG1 | 257 | SF-36 Vitality Subscale | 58.7 (21.35) | NR | 248 | 58.7 | NR | p=0.19 | |
| 257 | SF-36 Physical Function Subscale | 80.2 (18.67) | NR | 248 | 79.0 (18.38) | NR | p=0.62 | |||
| Simpson, 2015296§ (WILMA) Fair | 12 | IG1 | 45 | EQ-5D Index score | NA | NA | 51 | NA | NA | OR: 0.85 (0.29 to 2.46)‖ |
| IG2 | 43 | EQ-5D Index score | NA | NA | 51 | NA | NA | OR: 1.39 (0.49 to 3.94)‖ | ||
| von Gruenigen, 2012310 McCarroll, 2014382 (SUCCEED) Fair | 12 | IG1 | 41 | Functional Assessment of Cancer Therapy-General (FACT-G) | NR | NR | 34 | NR | NR | NS, NR |
| Wadden, 2011206† Sarwer, 2013383 (POWER-UP) Good | 12 | IG1 | 131 | IWQOL-Lite (total) | 69.4 (17.5) | NR | 130 | 68.8 (17.5) | NR | NS, NR |
| SF-12 Mental | 48.9 (9.8) | NR | 48.7 (10.5) | NR | NS, NR | |||||
| SF-12 Physical | 43.9 (9.0) | NR | 43.4 (9.5) | NR | NS, NR | |||||
| EQ-5D Index score | 70.4 (18.8) | NR | 67.0 (20.0) | NR | NS, NR | |||||
| Wylie-Rosett, 2001315 Swencionis, 2013384 Fair | 12 | IG1 | 194 | Psychological Well-Being Index | NR | NR | 97 | NR | NR | NS, NR‡ |
| IG2 | 183 | NR | NR | NR | NR | NS, NR‡ |
- *
SE
- †
Included in previous review
- ‡
Results not reported by group, but no significant differences in well-being were found between groups at 12 months (anxiety p=0.53, depression p=0.32, positive well-being p=0.39, self-control p=0.11, general health p=0.38, vitality p=0.35, total well-being p=0.29)
- §
Weight Loss Maintenance study
- ‖
Reported as dichotomized analysis of (those with scores <100 vs. those with scores of 100 due to skewed and bimodal distribution of followup scores
Abbreviations: BL = baseline; CAMWEL = Camden Weight Loss; CG = control group; CI = confidence interval; DAMES = Daughters And Mothers Against Breast Cancer; DPP = Diabetes Prevention Program; EQ-5D = EuroQol Five Dimensions; EQ-VAS = EuroQol Visual Analogue Scale; FFIT = Football Fans in Training; FU = followup; IG = intervention group; IWQOL = Impact of Weight on Quality of Life; mos = months; n = number of participants; NA = not applicable; NR = not reported; NS = not statistically significant; OR = odds ratio; PA = physical activity; POWER-UP = Practice-based Opportunities for Weight Reduction at the University of Pennsylvania; PREDIAS = Prevention of Diabetes Self-Management Program; PROOF = Prevention of Knee Osteoarthritis in Overweight Females; QOL = quality of life; SD = standard deviation; SE = standard error; SF = short form; SUCCEED = Survivors of Uterine Cancer Empowered by Exercise and Healthy Diet; WILMA = Weight Loss Maintenance in Adults; WRAP = Weight-loss programme referrals for adults in primary care
Table 10Results of Medication-Based Weight Loss and Weight Loss Maintenance Interventions on Health-Related Quality of Life (k=10) (n=13145)
| Drug | Author, year (Study name) Quality | FU, mos | IG | IG N | Instrument | IG Mean (SD) BL | IG Mean change (95% CI or SD) | CG N | CG Mean (SD) BL | CG Mean change (95% CI or SD) | Study-reported between-group mean difference (95% CI or SD) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Liraglutide | Astrup, 2012220 Fair | 24 | 3.0mg QD | 98 | IWQOL-Lite (total) | NR | NR | 98 | NR | NR | NR* |
| Pi-Sunyer, 2015285 le Roux, 2017339 (SCALE Obesity and Prediabetes) Fair | 13 | 3.0mg QD | 2437 | IWQOL-Lite (total) | 73.0 (18.2) | 10.6 (13.3) | 1225 | 72.6 (18.2) | 7.7 (2.8) | 3.1 (2.2 to 4.0); p<0.0001 | |
| 13 | 3.0mg QD | 2437 | SF-36 Mental | 53.8 (8.1) | 0.2 (8.1) | 1225 | 54 (7.9) | −0.9 (9.1) | 0.9 (0.3 to 1.5); p=0.003 | ||
| 3.0mg QD | 2437 | SF-36 Physical | 48.2 (8.4) | 3.6 (6.8) | 1225 | 47.7 (8.7) | 2.1 (7.7) | 1.7 (1.2 to 2.2); p<0.001 | |||
| 36† | 3.0mg QD | 1472 | SF-36 Mental | NR | −0.5 (8.7) | 738 | NR | −1.4 (9.2) | 0.8 (−0.1 to 1.6); p=0.08 | ||
| 3.0mg QD | 1472 | SF-36 Physical | NR | 3.1 (7.3) | 738 | NR | 2.6 (7.6) | 0.9 (0.2 to 1.6); p=0.0156 | |||
| Lorcaserin hydrochloride | Fidler, 2011173 (BLOSSOM) Fair | 12 | 10mg BID | 1561 | IWQOL-Lite (total) | 74.7 (16.1) | LSM: 11.8 (10.1) | 1541 | 75.3 (15.6) | LSM: 10.0 (10.1) | p<0.001 |
| Smith, 2010172 (BLOOM) Fair | 12 | 10mg BID | 1538 | IWQOL-Lite (total) | 73.92 (0.41)‡ | 12.4 (0.4)‡ | 1499 | 73.85 (0.42)‡ | 10.7 (0.4)‡ | p<0.001 | |
| Nal-Bup | Apovian, 2013218 (COR-11) Fair | 13 | 16/180mg TID | 702 | IWQOL-Lite (total) | 71.9 (17.1) | LSM: 10.9 (0.5)‡ | 456 | 73.0 (15.9) | 6.4 (0.6)‡ | p<0.001 |
| Greenway, 2010244 (COR-1) Fair | 13 | 16/180mg TID | 471 | IWQOL-Lite (total) | 70.3 (16.5) | LSM: 12.7 (11.6 to 13.8) | 511 | 71.8 (17.2) | LSM: 8.6 (−7.5 to 9.6) | LSM change: p<0.0001 | |
| Wadden, 2011311 (COR-BMOD) Fair | 12 | 16/180mg TID | 482 | IWQOL-Lite (total) | 71.9 (15.4) | LSM: 13.4 (12.3 to 14.5) | 193 | 73.5 (15.6) | LSM: 10.3 (8.6 to 12.0) | p<0.001 | |
| Orlistat | Rossner, 2000292 Fair | 24 | 120mg TID | NR | Global and obesity-specific health state preference | NR | NR | NR | NR | NR | Satisfaction with: Medication: p<0.001 WL: p=0.001 WL program: p=0.002 Overall treatment: p<0.001 Less overweight distress: p<0.05 |
| 60mg TID | NR | NR | NR | NR | NR | NR | Satisfaction with: Medication: p<0.05 WL: NS, NR WL program: NS, NR Overall treatment: p<0.05 Less overweight distress: p<0.05 | ||||
| Swinburn, 2005304 Fair | 12 | 120mg TID | 166 | SF-36 | NR | NR | 167 | NR | NR | NS, NR§ | |
| Phen-Top | Gadde, 2011241 (CONQUER/SEQUEL) Fair | 13 | 15/92mg QD | NR | IWQOL-Lite (total) | NR | NR | NR | NR | NR | NR‖ |
| 7.5/46mg QD | NR | NR | NR | NR | NR | NR | NR | ||||
| 15/92mg QD | NR | SF-36 | NR | NR | NR | NR | NR | NR¶ | |||
| 7.5/46mg QD | NR | NR | NR | NR | NR | NR | NR |
- *
Quality of life improved in all groups at years 1. Total change and statistical significance NR.
- †
Participants with prediabetes at baseline only
- ‡
Standard error
- §
Vitality subscale: Higher scores in IG (p=0.006); all other domains NS
- ‖
Reported to have greater improvements on most QOL measures compared with placebo, data NR
- ¶
Reported to have greater improvements on most QOL measures compared with placebo, data NR
Abbreviations: BID = twice a day; BLOOM = Behavioral Modification and Lorcaserin for Overweight and Obesity Management; BL = baseline; BLOSSOM = Behavioral Modification and Lorcaserin Second Study for Obesity Management; CI = confidence interval; COR-1 = Contrave Obesity Research-1; COR-11 = CONTRAVE Obesity Research-II; COR-BMOD = Contrave Obesity Research - Behavior Modification; IWQOL = Impact of Weight on Quality of Life; LSM = least squares mean; mg = milligram; Nal-Bup = Naltrexone HCL and bupropion HCL; NR = not reported; NS = not statistically significant; Phen-Top = Phentermine-topiramate extended release; QD = once a day; SD = standard deviation; SF = short form; TID = three times a day; WL = weight loss
Table 11Pooled Results of Weight Loss Outcomes for Behavior-Based Weight Loss Interventions
| Outcome | Followup | Mean Difference in Change (95% CI) | Trials, k | n | I2, % |
|---|---|---|---|---|---|
| Weight, kg§ | 12-18 months | −2.39 (−2.86 to −1.93) | 67 | 22065 | 90.0 |
| 24 months | −1.45 (−2.03 to −0.87) | 21 | 7268 | 67.9 | |
| Weight, % change | 12-18 months | −3.10 (−3.51 to −2.68) | 26 | 5734 | 99.5 |
| BMI, kg/m2 | 12-18 months | −1.01 (−1.29 to −0.74) | 40 | 10924 | 92.2 |
| Waist circumference, cm‖ | 12-18 months | −2.51 (−3.15 to −1.87) | 41 | 12180 | 94.6 |
| Outcome | Followup | Risk Ratio (95% CI) | Trials, k | n | I2, % |
| ≥5% weight loss | 12-18 months | 1.94 (1.70 to 2.22) | 38 | 12231 | 67.2 |
| 24 months | 1.51 (1.25 to 1.81) | 13 | 4824 | 63.0 | |
| ≥10% weight loss | 12-18 months | 3.06 (2.41 to 3.88) | 16 | 6975 | 49.0 |
- §
To convert kg to lbs, multiply by 2.205
- ‖
To convert cm to inches, multiply by 0.394
Abbreviations: BMI = body mass index; cm = centimeter(s); CI = confidence interval; kg= kilogram(s); lb(s) = pound(s)
Table 12Results of BehaviorBased Weight Loss Interventions on Incident Diabetes (k=13) (n=4095)
| Author, year (Study name) Quality | FU, mos | IG | IG N | IG FU n (%) | CG N | CG FU n (%) | Study-reported between-group difference |
|---|---|---|---|---|---|---|---|
| Ackermann, 2015215 (RAPID-YDPP) Fair | 12 | IG1 | 220 | 26 (11.8) | 226 | 24 (10.6) | p=0.7 |
| Bhopal, 2014225 (PODOSA) Good | 36 | IG1 | 81 | 12 (15.0) | 82 | 17 (21.0) | OR=0.68 (0.27 to 1.67) p=0.37 |
| Katula, 2011258 (HELP PD) Good | 12 | IG1 | 135 | 2 (1.5) | 138 | 7 (5.1) | p=0.12 |
| Knowler, 2012205* (DPP) Good | 36 | IG1 | 638 | 4.8† | 657 | 11.0† | NR |
| 92 (14.4)‖ | 190 (28.9)‖ | -58% (48% to 66%) NNT=6.9 (5.4 to 9.5) | |||||
| Luley, 2014265 Fair | 12 | IG1 | 58 | 1 (1.7) | 60 | 3 (5.0) | NR |
| IG2 | 60 | 0 (0.0) | 60 | 3 (5.0) | NR | ||
| Ma, 2013266 (E-LITE) Good | 15 | IG1 | 79 | 1 (1.3) | 81 | 1 (1.2) | NR |
| 15 | IG2 | 81 | 0 (0.0) | 81 | 1 (1.2) | NR | |
| Nicklas, 2014277 (Balance after Baby) Fair | 12 | IG1 | 36 | 0 (0.0) | 39 | 3 (7.7) | NS, NR |
| O’Brien, 2017321 (PREVENT-DM) Good | 12 | IG1 | 33 | 0 (0.0) | 30 | 1 (3.3) | NR |
| Parikh, 2010280* (HEED) Fair | 12 | IG1 | 50 | 0.36‡ | 49 | 0.33‡ | NS, NR |
| Penn, 2009283 (EDIPS-Newcastle) Fair | 60 | IG1 | 51 | 32.7 (10.7 to 74.6)§ | 51 | 67.1 (34.2 to 117.5)§ | NR |
| 5 (9.8) | 11 (21.6) | RR=0.45 (0.20 to 1.20) | |||||
| Rock, 2015288 Sedjo, 2016385 (ENERGY) Good | 12 | IG1 | 271 | 0 (0.0) | 245 | 1 (0.4%) | NR |
| Tuomilehto, 2001306* Lindstrom, 2013340 (Finnish DPS) Good | 12 | IG1 | 265 | 5 (1.9) | 257 | 16 (6.2) | NR |
| 24 | 15 (5.7) | 37 (14.4) | NR | ||||
| 36 | 22 (8.3) | 51. (19.8) | NR | ||||
| 48 | 24 (9.1) | 53 (20.6) | NR | ||||
| 60 | 27 (10.2) | 57 (22.2) | NR | ||||
| 72 | 27 (10.2) | 59 (23.0) | HR=0.4 (0.30 to 0.70) p<0.001 | ||||
| 108 | 106 (40.0) | 140 (54.5) | HR=0.61 (0.48 to 0.79) p<0.001 | ||||
| Wing, 1998314 Fair | 24 | IG1 | 32 | 5.0 (15.6) | 29 | 2.0 (6.9) | NR, p=0.079 for 4-group comparison |
| IG2 | 33 | 10.0 (30.3) | 29 | 2.0 (6.9) | |||
| IG3 | 28 | 4.0 (14.3) | 29 | 2.0 (6.9) |
- *
Included in previous review
- †
Cases//100 person-years
- ‡
Cases/person-years
- §
Cases/1000 person-years (95% confidence interval)
- ‖
Cumulative incidence: 38.0% per 100 person-years
Abbreviations: CG = control group; DPP = Diabetes Prevention Program; DPS = Diabetes Prevention Study; EDIPS = European Diabetes Prevention Study; E-LITE = Evaluation of Lifestyle Interventions to Treat Elevated Cardiometabolic Risk in Primary Care; ENERGY = Exercise and Nutrition to Enhance Recovery and Good Health for You; FU = followup; HEED = Project Help Educate to Eliminate Diabetes; HELP PD = Healthy Partnerships to Prevent Diabetes; HR = hazard ratio; IG = intervention group; mos= months; NNT = number needed to treat; NR = not reported; NS = not statistically significant; OR = odds ratio; PA = physical activity; PODOSA = Prevention of Diabetes and Obesity in South Asians; PREVENT-DM = The Promotora Effectiveness Versus Metformin Trial; RAPID-YDPP = Reaching Out to Prevent Increases in Diabetes - YMCA model for Diabetes Prevention Program; RR = risk ratio; YMCA = The Young Men’s Christian Association
Table 13Results of Medication-Based Weight Loss Interventions on Weight Loss (kg), by Drug (k=18) (n=22,972)
| Drug | Author Year | FU, mos | % FU | Dose | IG N | IG Mean (SD) BL | IG Mean change (95% CI) | CG N | CG Mean (SD) BL | CG Mean change (95% CI) | Between-group difference in mean change (95% CI)*; study-reported p-value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Liraglutide | Astrup, 2012220 | 12 | 63.1 | 3.0mg QD | 93 | 97.5 (13.8) | −7.8 (NR) | 98 | 97.3 (12.3) | −2.0 (NR) | −5.80 (−8.00 to −3.70); p<0.0001 |
| Pi-Sunyer, 2015285 le Roux, 2017339 | 13 | 69.4 | 3.0mg QD | 2437 | 106.2 (21.2) | −8.4 (−8.7 to −8.1) | 1225 | 106.2 (21.7) | −2.8 (−3.2 to −2.4) | −5.60 (−6.00 to −5.10); p<0.001 | |
| 36† | 50.0 | 3.0mg QD | 1472 | 107.5 (21.6) | −6.5 (−6.9 to −6.1) | 738 | 107.9 (21.8) | −2.0 (−2.5 to −1.5) | −4.60 (−5.30 to −3.90); p<0.0001 | ||
| Lorcaserin hydrochloride | Fidler, 2011173 | 12 | 55.5 | 10mg BID | 1561 | 100.3 (15.7) | LSM: −5.8 (−6.1 to −5.5) | 1541 | 100.8 (16.2) | LSM: −2.9 (−3.2 to −2.6) | LSM: −2.90 (NR); p<0.001 |
| Smith, 2010172 | 12 | 49.7 | 10mg BID | 1538 | 100.4 (16.0) | −5.8 (−6.2 to −5.4) | 1499 | 99.7 (15.9) | −2.2 (−2.4 to −2.0) | −3.60 (−4.04 to −3.16); p<0.001 | |
| Nal-Bup | Apovian, 2013218 | 13 | 53.8 | 16/180mg TID | 702 | 100.3 (16.6) | LSM: −6.2 (−6.6 to −5.8) | 456 | 99.2 (15.9) | LSM: −1.3 (−1.9 to −0.7) | NR; p<0.001 |
| Greenway, 2010244 | 13 | 59.9 | 16/180mg TID | 471 | 99.7 (15.9) | LSM: −6.1 (−6.7 to −5.5) | 511 | 99.5 (14.3) | LSM: −1.4 (−2.0 to −0.8) | NR; p<0.0001 | |
| Orlistat | Broom, 2002227 | 12 | 65.3 | 120mg TID | 259 | 100.9 (20.5) | −5.8 (−6.8 to −4.8) | 263 | 101.8 (19.8) | −2.3 (−3.1 to −1.5) | −3.50 (−4.79 to −2.21); p<0.0001 |
| Davidson, 1999160 | 12 | 66.3 | 120mg TID | 657 | 100.7 (15.4) | −8.8 (−9.5 to −8.0) | 223 | 100.6 (13.4) | −5.8 (−7.1 to −4.5) | −2.95 (−4.45 to −1.45); p<0.001 | |
| Derosa, 2003236 | 12 | 96.0 | 120mg TID | 25 | 94.2 (9.8) | −8.6 (−9.0 to −8.2) | 23 | 95.3 (10.2) | −7.6 (−7.9 to −7.3) | −1.00 (−1.49 to −0.51); p=NR | |
| Finer, 2000239 | 12 | 61.0 | 120mg TID | 110 | 97.9 (12.9) | LSM: −3.3 (NR) | 108 | 98.4 (15.0) | LSM: −1.3 (NR) | LSM: −1.99 (−3.60 to −0.38); p=0.016 | |
| Hauptman, 2000246 | 12 | 67.2 | 120mg TID | 210 | 100.5 (14.2) | −7.9 (−9.1 to −6.8) | 212 | 101.8 (14.6) | −4.1 (−5.2 to −3.0) | −3.80 (−5.37 to −2.23); p=0.001 | |
| 12 | 60mg TID | 213 | 100.4 (14.6) | −7.1 (−8.1 to −6.0) | 212 | 101.8 (14.6) | −4.1 (−5.2 to −3.0) | −2.94 (−4.46 to −1.42); p=0.001 | |||
| 18 | NR | 120mg TID | 210 | 100.5 (14.2) | −6.2 (−7.4 to −5.0) | 212 | 101.8 (14.6) | −2.9 (−4.0 to −1.8) | −3.29 (−4.94 to −1.64); p=0.001 | ||
| 18 | NR | 60mg TID | 213 | 100.4 (14.6) | −5.8 (−6.8 to −4.8) | 212 | 101.8 (14.6) | −2.9 (−4.0 to −1.8) | −2.85 (−4.36 to −1.34); p=0.001 | ||
| 24 | 51.7 | 120mg TID | 210 | 100.5 (14.2) | −5.0 (−6.5 to −3.6) | 212 | 101.8 (14.6) | −1.6 (−2.9 to −0.4) | −3.37 (−5.25 to −1.49); p=0.001 | ||
| 24 | 60mg TID | 213 | 100.4 (14.6) | −4.5 (−5.7 to −3.3) | 212 | 101.8 (14.6) | −1.6 (−2.9 to −0.4) | −2.81 (−4.51 to −1.11); p=0.001 | |||
| Krempf, 2003260 | 12 | 68.7 | 120mg TID | 346 | 97.0 (16.7) | LSM: −6.3 (−7.3 to −5.3) | 350 | 97.5 (16.8) | LSM: −3.3 (−4.3 to −2.3) | NR; p<0.0001 | |
| 18 | 61.1 | 120mg TID | 346 | 97.0 (16.7) | LSM: −5.3 (−6.3 to −4.3) | 350 | 97.5 (16.8) | LSM: −2.4 (−3.4 to −1.4) | NR; p<0.0001 | ||
| Lindgarde, 2000263 | 12 | 85.9 | 120mg TID | 190 | 96.1 (13.7) | −5.6 (−6.3 to −4.9) | 186 | 95.9 (13.5) | −4.3 (−5.1 to −3.5) | −1.30 (−2.43 to −0.17); p<0.05 | |
| Rossner, 2000292 | 12 | 71.9 | 120mg TID | 242 | 96.7 (13.8) | −9.4 (−10.2 to −8.6) | 237 | 97.7 (14.6) | −6.4 (−7.3 to −5.5) | −3.00 (−4.17 to −1.83); p<0.001 | |
| 12 | 60mg TID | 239 | 99.1 (14.3) | −8.5 (−9.4 to −7.6) | 237 | 97.7 (14.6) | −6.4 (−7.3 to −5.5) | −2.10 (−3.36 to −0.84); p<0.001 | |||
| 24 | 59.7 | 120mg TID | 242 | 96.7 (13.8) | −7.4 (−8.3 to −6.5) | 237 | 97.7 (14.6) | −4.3 (−5.2 to −3.4) | −3.10 (−4.40 to −1.80); p<0.001 | ||
| 24 | 60mg TID | 239 | 99.1 (14.3) | −6.6 (−7.7 to −5.5) | 237 | 97.7 (14.6) | −4.3 (−5.2 to −3.4) | −2.30 (−3.71 to −0.89); p=0.005 | |||
| Sjostrom, 1998297 | 12 | 79.1 | 120mg TID | 343 | 99.1 (NR) | −10.3 (NR) | 340 | 99.8 (NR) | −6.1 (NR) | −4.20 (NR); p<0.001 | |
| Swinburn, 2005304 | 12 | 79.4 | 120mg TID | 170 | 103.3 (17.8) | −4.7 (−5.9 to −3.5) | 169 | 106.9 (17.8) | −0.9 (−1.5 to −0.3) | −3.80 (−5.12 to −2.48); p=0.001 | |
| Torgerson, 2004161 | 12 | 83.1 | 120mg TID | 1640 | 110.4 (16.3) | −10.6 (NR) | 1637 | 110.6 (16.5) | −6.2 (NR) | −4.40 (NR); p<0.001 | |
| 48 | 42.8 | 120mg TID | 1640 | 110.4 (16.3) | −5.8 (NR) | 1637 | 110.6 (16.5) | −3.0 (NR) | LSM: −2.70 (NR); p<0.001 | ||
| Phen-Top | Gadde, 2011241 | 13 | 69.3 | 15/92 mg QD | 981 | 103.0 (17.6) | LSM: −10.2 (−10.8 to −9.7) | 979 | 103.3 (18.1) | LSM: −1.4 (−2.0 to −0.8) | NR; p<0.0001 |
| 13 | 7.5/46 mg QD | 488 | 102.6 (18.2) | LSM: −8.1 (−8.9 to −7.4) | 979 | 103.3 (18.1) | LSM: −1.4 (−2.0 to −0.8) | NR; p<0.0001 |
- *
Study-reported adjusted between group difference in mean change reported if available; otherwise, calculated unadjusted between group difference.
- †
Individuals with prediabetes at baseline only
Abbreviations: BID = twice a day; BL = baseline; CG = control group; CI = confidence interval; cm = centimeters; FU = followup; kg = kilograms; LSM = least squares mean; mg = milligram; mos = months; Nal-Bup = Naltrexone HCL and bupropion HCL; NR = not reported; Phen-Top = Phentermine-topiramate extended release; QD = once a day; SD = standard deviation; TID = three times a day; WC = waist circumference
Table 14Results of Medication-Based Weight Loss Interventions on Waist Circumference (cm), by Drug (k=14) (n=22,227)
| Drug | Author, year | FU, mos | % FU | Dose | IG N | IG Mean (SD) BL | IG Mean change (95% CI) | CG N | CG Mean (SD) BL | CG Mean change (95% CI) | Between-group difference in mean change (95% CI)* |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Liraglutide | Astrup, 2012220 | 12 | 63.1 | 3.0mg QD | 93 | 109.0 (8.3) | −7.8 (NR) | 98 | 108.0 (10.0) | −3.0 (NR) | −4.70 (−7.10 to −2.40); p<0.0001 |
| Pi-Sunyer, 2015285 le Roux, 2017339 | 13 | 69.4 | 3.0mg QD | 2437 | 115.0 (14.4) | −8.2 (−8.5 to −7.9) | 1225 | 114.5 (14.3) | −3.9 (−4.3 to −3.5) | −4.20 (−4.70 to −3.70); p<0.001 | |
| 36† | 50.0 | 3.0mg QD | 1472 | 116.5 (14.4) | −6.9 (−7.3 to −6.5) | 738 | 116.7 (13.9) | −3.4 (−3.9 to −2.9) | −3.50 (−4.20 to −2.80); p<0.0001 | ||
| Lor-Hyd | Fidler, 2011173 | 12 | 55.5 | 10mg BID | 1561 | 108.9 (12.2) | LSM: −6.3 (−6.7 to −5.9) | 1541 | 110.2 (12.5) | LSM: −4.1 (−4.5 to −3.7) | NR; p<0.001 |
| Smith, 2010172 | 12 | 49.7 | 10mg BID | 1538 | 109.6 (12.0) | −6.8 (−7.2 to −6.4) | 1499 | 109.2 (12.0) | −3.9 (−4.3 to −3.5) | −2.90 (−3.45 to −2.35); p<0.001 | |
| Nal-Bup | Apovian, 2013218 | 13 | 53.8 | 16/180mg TID | 702 | 109.0 (11.8) | LSM: −6.7 (−7.3 to −6.1) | 456 | 108.6 (11.8) | LSM: −2.1 (−3.1 to −1.1) | NR; p<0.001 |
| Greenway, 2010244 | 13 | 59.9 | 16/180mg TID | 471 | 108.8 (11.3) | LSM: −6.2 (−7.1 to −5.4) | 511 | 110.0 (12.2) | LSM: −2.5 (−3.3 to −1.6) | NR; p<0.0001 | |
| Wadden, 2011311 | 12 | 51.3 | 16/180mg TID | 482 | 109.3 (11.4) | −10.2 (−10.9 to −9.0) | 193 | 109.0 (11.8) | −7.0 (−8.3 to −5.3) | −3.20 (−4.98 to −1.42); p<0.001 | |
| Orlistat | Broom, 2002227 | 12 | 65.3 | 120mg TID | 259 | 107.8 (15.6) | −6.0 (NR) | 263 | 108.6 (16.4) | −2.6 (NR) | −3.39 (NR); p<0.0001 |
| Derosa, 2003236 | 12 | 96.0 | 120mg TID | 25 | 100.8 (5.3) | −3.0 (−3.4 to −2.6) | 23 | 102.3 (6.2) | −2.4 (−2.6 to −2.2) | −0.60 (−1.02 to −0.18); p=NR | |
| Krempf, 2003260 | 18 | 61.1 | 120mg TID | 346 | 105.6 (14.9) | LSM: −5.3 (−6.7 to −3.9) | 350 | 106.5 (15.0) | LSM: −3.5 (−4.9 to −2.1) | NR; p<0.05 | |
| Lindgarde, 2000263 | 12 | 85.9 | 120mg TID | 190 | 106.0 (10.8) | −4.8 (NR) | 186 | 106.0 (11.0) | −4.1 (NR) | −0.70 (NR); p>0.05 | |
| Rossner, 2000292 | 12 | 71.9 | 120mg TID | 242 | NR | −6.2 (NR) | 237 | NR | −4.7 (NR) | −1.50 (NR); p=NR, NS | |
| 12 | 60mg TID | 239 | NR | −6.0 (NR) | 237 | NR | −4.7 (NR) | −1.30 (NR); p=NR, NS | |||
| 24 | 59.7 | 120mg TID | 242 | NR | −5.1 (NR) | 237 | NR | −3.1 (NR) | −2.00 (NR); p<0.05 | ||
| 24 | 59.7 | 60mg TID | 239 | NR | −4.7 (NR) | 237 | NR | −3.1 (NR) | −1.60 (NR); p=NR | ||
| Swinburn, 2005304 | 12 | 79.4 | 120mg TID | 170 | 112.4 (12.8) | −5.1 (−6.2 to −4.0) | 169 | 114.8 (13.1) | −1.9 (−2.5 to −1.3) | −3.20 (−4.43 to −1.97); p=0.001 | |
| Torgerson, 2004161 | 12 | 83.1 | 120mg TID | 1640 | 115.0 (10.4) | −9.6 (NR) | 1637 | 115.4 (10.4) | −7.0 (NR) | −2.60 (NR); p<0.01 | |
| 48 | 42.8 | 120mg TID | 1640 | 115.0 (10.4) | −6.4 (NR) | 1637 | 115.4 (10.4) | −4.4 (NR) | −2.00 (NR); p<0.01 | ||
| Phen-Top | Allison, 2012216 | 12 | 59.9 | 15/92mg QD | 498 | 120.1 (14.6) | LSM: −10.9 (−11.8 to −10.0) | 498 | 120.5 (13.9) | LSM: −3.1 (−4.0 to −2.2) | NR; p<0.0001 |
| Gadde, 2011241 | 13 | 69.3 | 15/92mg QD | 981 | 113.2 (12.2) | LSM: −9.2 (−9.8 to −8.6) | 979 | 113.4 (12.2) | LSM: −2.4 (−3.0 to −1.8) | NR; p<0.0001 | |
| 13 | 7.5/46mg QD | 488 | 112.6 (12.5) | LSM: −7.6 (−8.4 to −6.9) | 979 | 113.4 (12.2) | LSM: −2.4 (−3.0 to −1.8) | NR; p<0.0001 |
- *
Study-reported adjusted between group difference in mean change reported if available; otherwise, calculated unadjusted between group difference.
- †
Individuals with prediabetes at baseline only
Abbreviations: BID = twice a day; BL = baseline; CG = control group; CI = confidence interval; cm = centimeters; FU = followup; IG = intervention group; Lor-Hyd = Lorcaserin hydrochloride; LSM = least squares mean; mg = milligram; mos = months; QD = once a day; Nal-Bup = Naltrexone HCL and bupropion HCL; NA = not applicable; NR = not reported; NS = not statistically significant; Phen-Top = Phentermine-topiramate extended release; QD = once a day; SD = standard deviation; TID = three times a day;
Table 15Results of Medication-Based Weight Loss and Weight Loss Maintenance Interventions on Incident Diabetes (k=4) (n=9340)
| Drug | Author, year (Study name) Quality | FU, months | Dosage | IG N | IG FU n (%) | CG N | CG FU n (%) | Study-reported between-group difference (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Liraglutide | Pi-Sunyer, 2015285 le Roux, 2017339 (SCALE Obesity and Prediabetes) Fair | 13 | 3.0mg QD | 2437 | 4 (0.16%) | 1225 | 14 (1.1%) | OR: 8.1 (2.6 to 25.3) p<0.001 |
| 36* | 3.0mg QD | 1472 | 26 (1.8%) | 738 | 46 (6.2%) | HR: 0.21 (95% CI: 0.13-0.34, p<0.0001) | ||
| Orlistat | Torgerson, 2004161 (XENDOS) Fair | 48 | 120mg TID | 1640 | 101 (6.2%) | 1637 | 147 (9.0%) | HR: 0.63 (0.46 to 0.87) p=0.0052 |
| Richelsen, 2007287† Fair | 36 | 120mg TID | 153 | 8 (5.2%) | 156 | 17 (10.9%) | p=0.041 | |
| Phen/Top | Gadde, 2011241 (CONQUER/SEQUEL) Fair | 13 | 15/92mg QD | 828 | 14 (1.7%) | 834 | 30 (3.6%) | RR: 0.47 (0.25 to 0.88) p=NR |
| 13 | 7.5/46mg QD | 430 | 12 (2.8%) | 834 | 30 (3.6%) | RR: 0.78 (0.40 to 1.50) p=NR |
- *
36 month outcomes are for individuals with prediabetes at baseline only
- †
Weight loss maintenance trial
Abbreviations: CG = control group; CI = confidence interval; FU = followup; IG = intervention group; HR = hazard ratio; LSM = least squares mean; mg = milligram; mos = months; QD = once a day; Nal-Bup = Naltrexone HCL and bupropion HCL; NR = not reported; OR = odds ratio; Phen-Top = Phentermine-topiramate extended release; RR = risk ratio; TID = three times a day; XENDOS = XENical in the prevention of Diabetes in Obese Subjects
Table 16Percent of Individuals Experiencing at Least One Adverse Event in Studies of Medication-Based Weight Loss and Weight Loss Maintenance (k=16) (n=14,428
| Drug | Author, year | FU, mos | Dosage | IG N | IG FU n (%) | CG N | CG FU n (%) | Study-reported between-group difference |
|---|---|---|---|---|---|---|---|---|
| Liraglutide | Astrup, 2012220 | 12 | 3.0mg QD | 93 | 89 (95.7) | 98 | 87 (88.8) | NR |
| Pi-Sunyer, 2015285 | 13 | 3.0mg QD | 2481 | 1992 (80.3) | 1242 | 786 (63.3) | NR | |
| 36* | 3.0mg QD | 1501 | 1421 (94.7) | 747 | 668 (89.4) | NR | ||
| Wadden, 2013312† | 13 | 3.0mg QD | 212 | 194 (91.5) | 210 | 186 (88.6) | NR | |
| Lorcaserin | Farr, 2016238 | 1 | 10mg BID | 24 | 3 (12.5) | 24 | 1 (4.2) | NR |
| Fidler, 2011173 | 12 | 10mg BID | 1602 | 1323 (82.6) | 1601 | 1205 (75.3) | NR | |
| Nal-Bup | Apovian, 2013218 | 13 | 16/180mg TID | 992 | 852 (85.9) | 492 | 370 (75.2) | NR, NS |
| Greenway, 2010244 | 13 | 16/180mg TID | 573 | 476 (83.1) | 569 | 390 (68.5) | <0.05 | |
| Orlistat | Bakris, 2002222 | 12 | 120mg TID | 276 | 246 (89.0) | 275 | 195 (71.0) | <0.001 |
| Broom, 2002227 | 6 | 120mg TID | 67 | 64 (95.5) | 71 | 61 (85.9) | NR | |
| Krempf, 2003260 | 18 | 120mg TID | 346 | 298 (86.1) | 350 | 253 (72.3) | <0.001 | |
| Muls, 2001273 | 6 | 120mg TID | 147 | 118 (80.0) | 143 | 96 (67.0) | 0.016 | |
| Sjostrom, 1998297 | 12 | 120mg TID | 343 | 322 (94.0) | 340 | 279 (82.0) | NR | |
| Smith, 2011298 | 6 | 60mg TID | 63 | 57 (90.5) | 64 | 52 (81.2) | NR | |
| Swinburn, 2005304 | 12 | 120mg TID | 170 | 161 (94.7) | 169 | 158 (93.5) | NR | |
| Van Gaal, 1998307 | 6 | 120mg TID | 120 | 101 (84.0) | 124 | 86 (69.0) | NR | |
| 6 | 60mg TID | 123 | 102 (83.0) | 124 | 86 (69.0) | NR | ||
| Phen-Top | Allison, 2012216 | 13 | 15/92mg QD | 511 | 432 (84.5) | 513 | 374 (72.9) | NR |
- *
Individuals with prediabetes at baseline only
- †
Weight loss maintenance study
Abbreviations: BID = twice a day; CG = control group; FU = followup; IG = intervention group; mg = milligram; mos = months; QD = once a day; Nal-Bup = Naltrexone HCL and bupropion HCL; NR = not reported; NS = not statistically significant; Phen-Top = Phentermine-topiramate extended release; TID = three times a day
Table 17Percent of Individuals Experiencing at Least One Serious Adverse Event in Studies of Medication-Based Weight Loss and Weight Loss Maintenance (k=25) (n=25,496)
| Drug | Author, year | FU, mos | Dosage | IG N | IG FU n (%) | CG N | CG FU n (%) | Study-reported between-group difference |
|---|---|---|---|---|---|---|---|---|
| Liraglutide | Astrup, 2012220 | 12 | 3.0mg QD | 93 | 7 (7.5) | 98 | 3 (3.1) | NR |
| Pi-Sunyer, 2015285 | 13 | 3.0mg QD | 2481 | 154 (6.2) | 1242 | 62 (5.0) | NR | |
| le Roux, 2017339 | 36* | 3.0mg QD | 1501 | 227 (15.1) | 747 | 96 (12.8) | NR | |
| Wadden, 2013† | 13 | 3.0mg QD | 212 | 9 (4.2) | 210 | 5 (2.4) | NR | |
| Lorcaserin | Fidler, 2011173 | 12 | 10mg BID | 1602 | 49 (3.1) | 1601 | 36 (2.2) | NR |
| Martin, 2011268 | 2 | 10mg BID | 29 | 0 (0.0) | 28 | 0 (0.0) | NR | |
| Smith, 2010172 | 12 | 10 mg BID | 1593 | NR | 1584 | NR | NR‡ | |
| Nal-Bup | Apovian, 2013218 | 13 | 16/180mg TID | 992 | 21 (2.1) | 492 | 7 (1.4) | NR, NS |
| Greenway, 2010244 | 13 | 16/180mg TID | 573 | 9 (1.6) | 569 | 8 (1.4) | NR | |
| Wadden, 2011311 | 12 | 16/180mg TID | 584 | 2 (0.3) | 200 | 0 (0.0) | NR | |
| Orlistat | Bakris, 2002222 | 12 | 120mg TID | 276 | 14 (5.1) | 275 | 15 (5.4) | NR |
| Broom, 2002226 | 6 | 120mg TID | 67 | 4 (6.0) | 71 | 6 (8.4) | NR | |
| Broom, 2002227 | 12 | 120mg TID | 259 | 13 (5.0) | 263 | 17 (6.5) | NR | |
| Derosa, 2003236 | 12 | 120mg TID | 27 | 0 (0.0) | 23 | 0 (0.0) | NR | |
| Finer, 2000239 | 12 | 120mg TID | 23 | 3 (13.0) | 23 | 6 (26.0) | NR | |
| Krempf, 2003260 | 18 | 120mg TID | 346 | 5 (1.4) | 350 | 4 (1.1) | NR | |
| Lindgarde, 2000263 | 12 | 120mg TID | 190 | 19 (10.0) | 186 | 5 (2.7) | NR | |
| Richelsen, 2007287† | 36 | 120mg TID | 153 | 18 (11.8) | 156 | 28 (17.9) | NS, NR | |
| Sjostrom, 1998297 | 12 | 120mg TID | 343 | 25 (7.3) | 340 | 24 (7.0) | NR | |
| Smith, 2011298 | 6 | 60mg TID | 63 | 2 (3.2) | 64 | 1 (1.6) | NR | |
| Swinburn, 2005304 | 12 | 120mg TID | 170 | 16 (9.4) | 169 | 12 (7.1) | NR | |
| Torgerson, 2004161 | 48 | 120mg TID | 1640 | 246 (15.0) | 1637 | 213 (13.0) | NR | |
| Van Gaal, 1998307 | 6 | 120mg TID/60mg TID | 243 | 12 (4.9) | 124 | 2 (1.6) | NR | |
| Phen-Top | Allison, 2012216 | 13 | 15/92mg QD | 511 | 13 (2.5) | 513 | 13 (2.5) | NR |
| Aronne, 2013168 | 6 | 15/92mg QD | 108 | 2 (1.8) | 109 | 0 (0.0) | NR | |
| 6 | 7.5/46mg QD | 106 | 1 (0.9) | 109 | 0 (0.0) | NR | ||
| Gadde, 2011241 | 13 | 15/92mg QD | 994 | 50 (5.0) | 993 | 40 (4.0) | NS, NR | |
| 13 | 7.5/46mg QD | 498 | 15 (3.0) | 993 | 40 (4.0) | NS, NR | ||
| 25 | 15/92mg QD | 295 | 12 (4.1) | 227 | 9 (4.0) | NR | ||
| 25 | 7.5/46mg QD | 153 | 4 (2.6) | 227 | 9 (4.0) | NR |
- *
Participants with prediabetes at baseline only
- †
Weight loss maintenance study
- ‡
Rates of serious adverse events were reported to be similar among the study groups
Abbreviations: BID = twice a day; CG = control group; FU = followup; IG = intervention group; mos = months; QD = once a day; mg = milligram; Nal-Bup = Naltrexone HCL and bupropion HCL; NR = not reported; NS = not statistically significant; Phen-Top = Phentermine-topiramate extended release; TID = three times a day
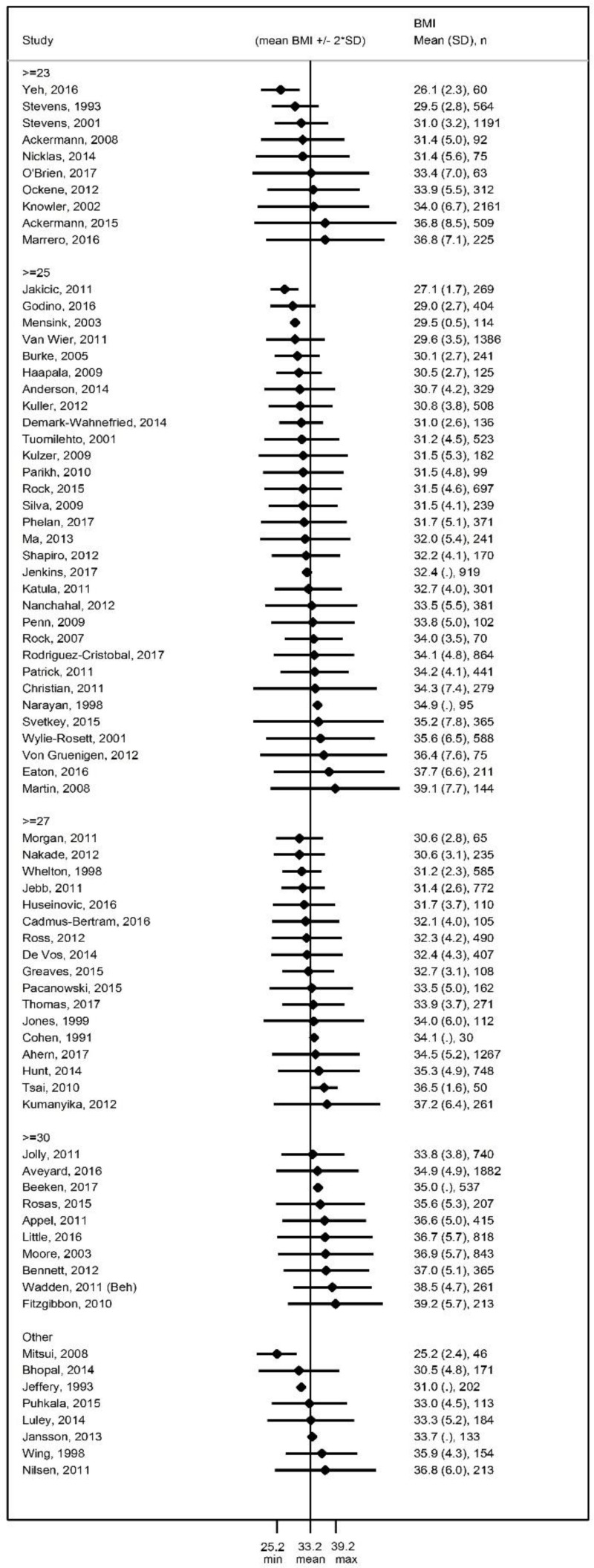
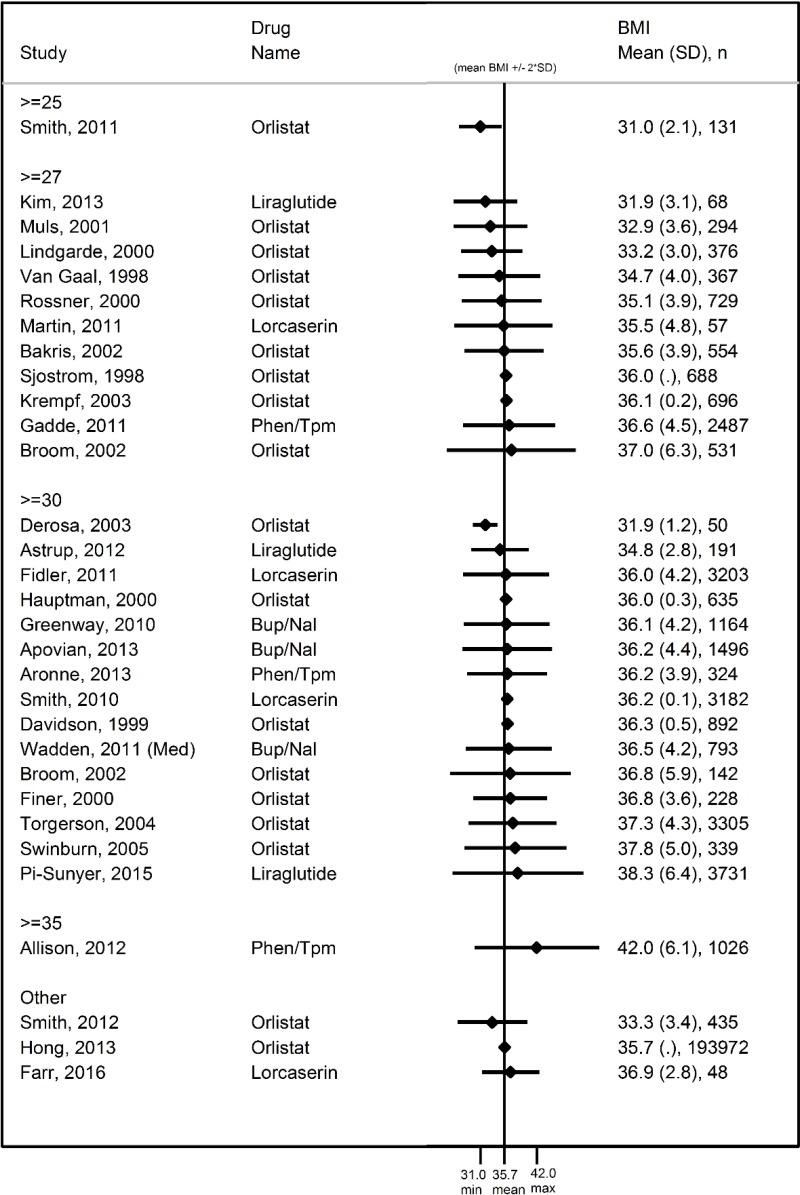
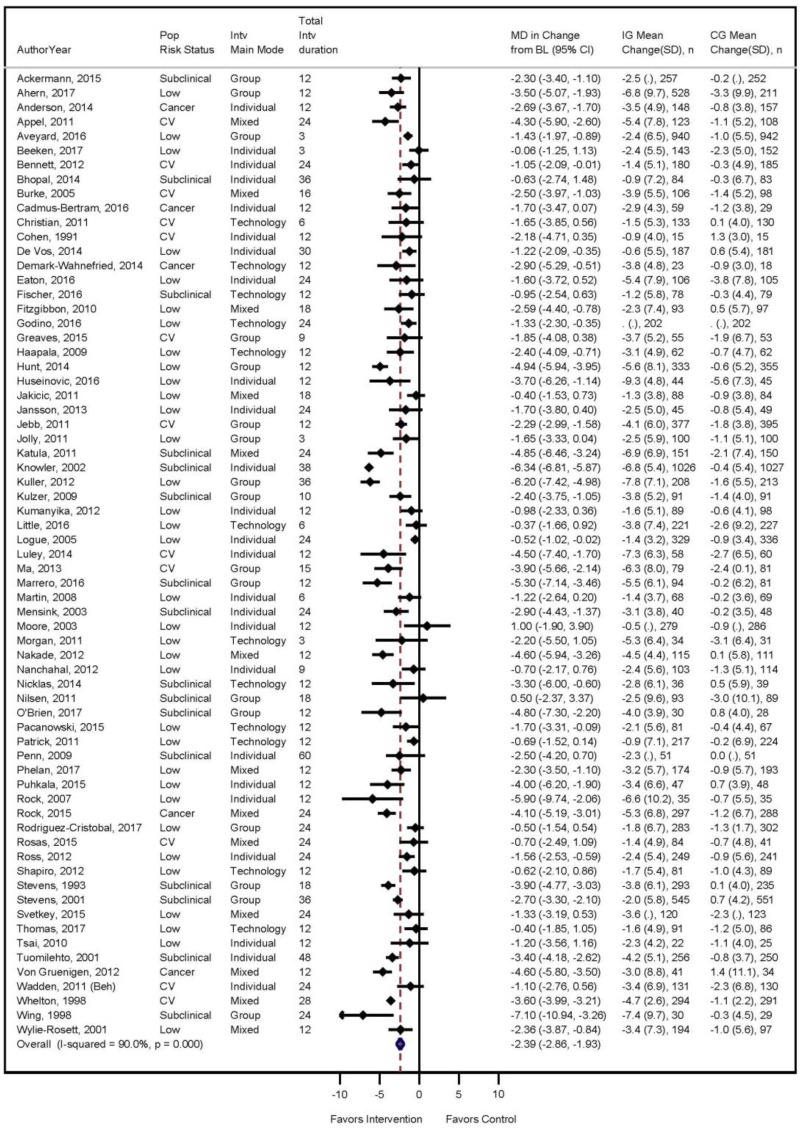
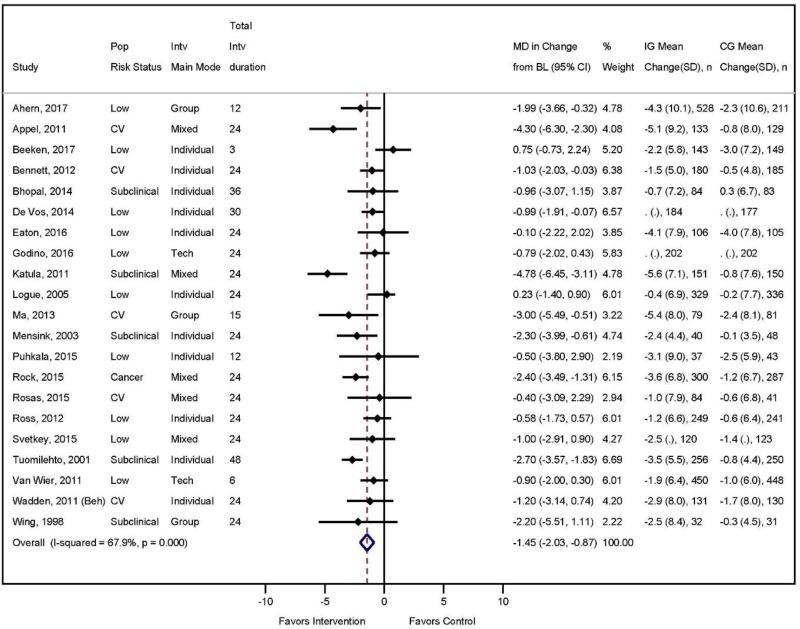
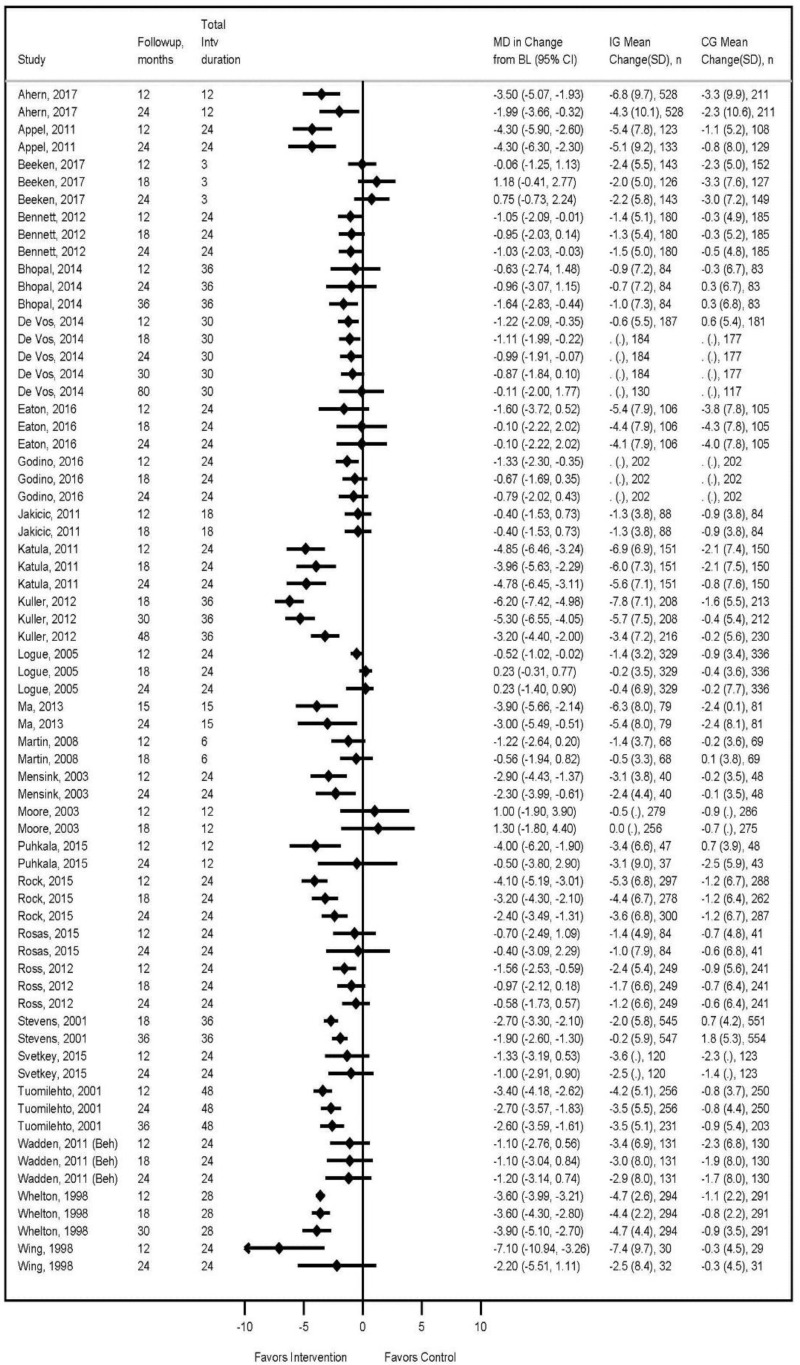
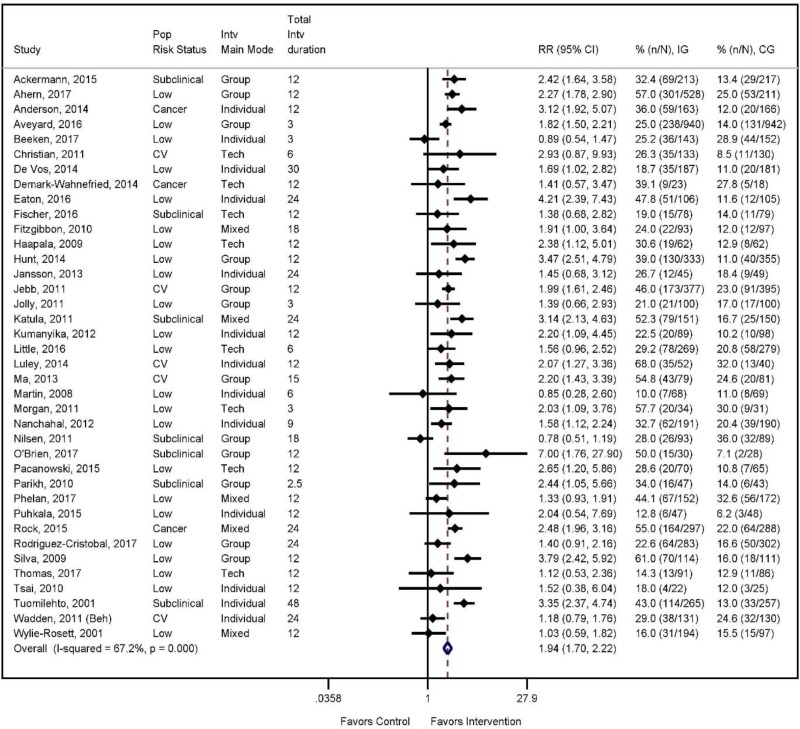

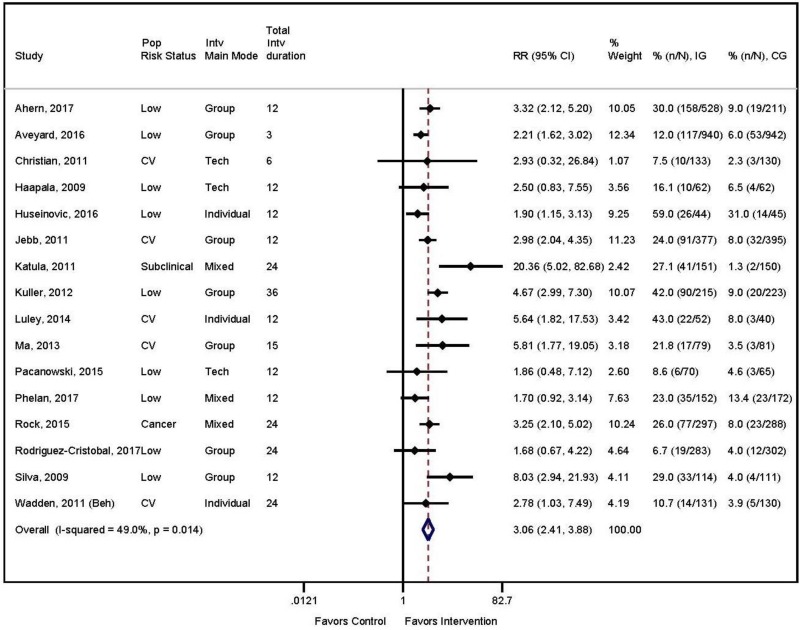
![Click on image to zoom Figure 10 displays a forest plot of the effect of 9 behavior-based weight loss trials (n=3140) on the incidence of diabetes. The pooled rates showed a significant 33% reduction in risk of developing diabetes over 1 to 9 years (pooled RR, 0.67 [95% CI, 0.51 to 0.89]).](/books/NBK532375/bin/ch3f9.jpg)