Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
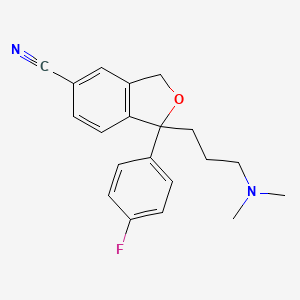
CASRN: 59729-33-8
Drug Levels and Effects
Summary of Use during Lactation
Infants receive citalopram in breastmilk and it is detectable in low levels in the serum of some. The dosage that the infant receives and serum level achieved are probably related to the genetic metabolic capacity of the mother and infant. A few cases of minor behavioral side effects such as drowsiness or fussiness have been reported, but no adverse effects on development have been found in infants followed for up to a year. Infants exposed in utero can have withdrawal effects postpartum despite breastfeeding and continued maternal citalopram use.[1,2] If citalopram is required by the mother, it is not a reason to discontinue breastfeeding. Some experts do not recommend citalopram during nursing,[3] but a safety scoring system finds citalopram to be acceptable during breastfeeding.[4] If the mother was taking citalopram during pregnancy or if other antidepressants have been ineffective, most experts recommend against changing medications during breastfeeding. Otherwise, agents with lower excretion into breastmilk may be preferred, especially while nursing a newborn or preterm infant. Monitor the infant for excess drowsiness, restlessness, irritability, poor feeding and poor weight gain, especially in younger, exclusively breastfed infants and when using combinations of psychotropic drugs.
Mothers taking an SSRI during pregnancy and postpartum may have more difficulty breastfeeding, although this might be a reflection of their disease state.[5] These mothers may need additional breastfeeding support. Breastfed infants exposed to an SSRI during the third trimester of pregnancy have a lower risk of poor neonatal adaptation than formula-fed infants.
Drug Levels
Citalopram is metabolized to 2 metabolites, each having antidepressant activity considered to be 13% that of citalopram.[6]
Maternal Levels. In a pooled analysis of serum levels from published studies and 2 unpublished cases, the authors found that 18 mothers taking an average daily dosage of 29 mg (range 20 to 60 mg) had an average milk citalopram level of 157 mcg/L (range 41 to 451 mcg/L).[6] Using the average dosage and milk level data from this paper, an exclusively breastfed infant would receive an estimated 7.9% of the maternal weight-adjusted dosage of citalopram.
A woman with postpartum depression was given citalopram 20 mg daily for 2 days, then 40 mg daily. After 8 days of therapy, a breastmilk sample contained 98.9 mcg/L of citalopram.[7]
In 9 mothers taking citalopram 20 to 40 mg daily while breastfeeding, trough milk samples were taken immediately before nursing on the morning of day 4, and during week 2 and month 2 postpartum. Citalopram milk trough concentrations standardized to a dosage of 20 mg daily averaged 81.4, 103.4 and 75.9 mcg/L at the 3 sampling times. The authors reported that an exclusively breastfed infant would receive an estimated minimum of 0.3 and 0.2% of the maternal weight-adjusted dosage of citalopram at 2 weeks and 2 months postpartum, respectively.[8] However, these values appear to be the result of a calculation error. Using the milk concentration values above, one can calculate a minimum infant dosage of 4.7 and 3.4% of the weight-adjusted maternal dosage which is consistent with values reported in other studies.
In 10 breastfed (extent not stated) infants (including one pair of twins) aged 3 to 42 weeks whose mothers were taking an average daily dosage of 24 mg (range 20 to 50 mg) of citalopram, the authors calculated that their fully breastfed infants would receive an average of 5.2% (range 2.5 to 9.4%) of the maternal dosage.[9]
A mother was taking oral citalopram 40 mg once daily in the evening. Single milk samples were obtained 16 hours after the dose on days 25, 46 and 53 postpartum. Milk citalopram levels were 280, 230 and 320 mcg/L. These values represent 5.8%, 4.7% and 6.6% of the maternal weight-adjusted dosage.[1]
A nursing mother was taking citalopram 20 mg daily. Foremilk and hindmilk samples taken at 4 weeks postpartum, 11 hours after a dose contained 123 mcg/L and 131 mcg/L, respectively. The samples also contained 25 mcg/L and 31 mcg/L of desmethylcitalopram in foremilk and hindmilk, respectively.[10]
Two women treated with citalopram 5 or 10 mg daily during the third trimester of pregnancy and during breastfeeding provided trough milk samples during the first week postpartum. The citalopram milk levels were 62.6 mcg/L with the 5 mg dose and 95.4 mcg/L with the 10 mg dose. The calculated weight-adjusted percentage of maternal dosages were 18.4% and 13.2%, respectively. These values might be inaccurate because of the timing of milk sample collection.[11]
Random milk samples were obtained from 6 women taking a median dosage of 20 mg (range 10 to 30 mg) of citalopram daily had a median citalopram milk concentration of 111.5 mcg/L (range 41.5 to 260 mcg/L). The authors calculated that this represents a median infant dosage of 16.7 (range 6.2 to 39) mcg/kg daily. No correlation was found between maternal dosage and milk citalopram level.[12]
Infant Levels. In a pooled analysis of 5 mother-infant pairs from published and unpublished cases, the authors found that infants had an average of 7% of their mothers' citalopram plasma levels; 1 of the 5 infants had a plasma level greater than 10% of the mother's plasma level which was defined by the authors as being elevated.[6]
A woman with postpartum depression was given citalopram 20 mg daily for 2 days, then 40 mg daily. Sixteen days later, her breastfed infant had a serum level of 12.7 mcg/L. Because of difficult sleep in the infant, the mother’s dosage was decreased to 20 mg daily. After 1 week at this dosage, the infant’s serum citalopram was 4.5 mcg/L and the infant’s sleep normalized.[7]
The breastfed infants of 9 mothers who took citalopram during pregnancy and postpartum had serum citalopram levels that were 63% of maternal serum levels at delivery. The infants' serum levels fell by 37% by day 2, 61% by day 4, and 90% by week 2, despite exclusive breastfeeding. At 2 months of age, infant citalopram serum levels were about 2% of those of the mother; metabolite serum levels were somewhat higher.[8]
In 10 breastfed (extent not stated) infants aged 3 to 42 weeks whose mothers were taking citalopram in an average daily dosage of 24 mg (range 20 to 50 mg), citalopram was detected in 6 of the infants. The serum drug levels of the 10 infants averaged 0.9% (range 0 to 4.8%) of those of their mothers. Two of the infants with detectable citalopram were twins whose mother was a poor metabolizer of citalopram (CYP2C19*2 mutation). Five infants with the CYP2C19*1/*2 genotype had serum levels that were 3.75 times higher than the other 5 infants with the CYP2C19*1/*1 genotype.[9]
A mother was taking oral citalopram 40 mg once daily at 11 pm. Infant serum levels were measured at 12, 25 and 53 days of age, the first at an unspecified time and the latter two at 3 pm. Infant citalopram serum levels were 2.3, 1.2 and 1.7 mcg/L at these times. The infant serum levels on days 25 and 53 represented 0.9% and 1.8% of the mothers serum levels, respectively.[1]
Effects in Breastfed Infants
The manufacturer states that drowsiness and weight loss in breastfed infants has occurred.
Uneasy sleep that reversed with dosage reduction and partial formula supplementation was probably caused by citalopram in breastmilk in a 5-month-old infant.[7]
A group of 10 infants breastfed (6 exclusive, 3 received some formula beginning at 2 months) from birth to one year during maternal citalopram use had normal body weight and neurological development in all infants compared to 9 control infants whose mothers did not take citalopram.[8]
Three mothers who took an average citalopram dose of 15 mg once daily breastfed their infants exclusively for 4 months and at least 50% during months 5 and 6. Their infants had 6-month weight gains that were normal according to national growth standards.[13]
A study compared adverse reactions in 31 infants breastfed during maternal citalopram use to a control group of 31 breastfed infants whose mothers did not take an antidepressant. There were numerically more adverse events reported in the citalopram group (3 vs 1). However, the study found no statistical difference in the rate of adverse effects between the groups of infants and none of the side effects was serious. One mother reported infant irritability and restlessness after she began citalopram at 2 months postpartum. The side effects subsided after she stopped breastfeeding 2 weeks later.[14]
In 10 breastfed (extent not stated) infants aged 3 to 42 weeks whose mothers were taking citalopram an average of 24 mg daily, no short-term adverse reactions were noted clinically at the time of the study.[9]
A breastfed infant whose mother took citalopram 40 mg daily throughout pregnancy and postpartum had numerous symptoms such as superficial and irregular breathing, apnea, disordered sleep and hypotonia after birth. All symptoms disappeared by 3 weeks of age. Symptoms were judged to likely be withdrawal symptoms rather than side effects of the drug in the breastmilk.[1]
A woman was restarted on citalopram 10 mg daily after having stopped the drug for the last month of pregnancy. Her infant breastfed for 6 months (extent not stated). The infant had no perinatal complications, and the infant's pediatrician noted no neuropsychological abnormalities at 18 months of age.[15]
A woman took citalopram 60 mg and ziprasidone 40 mg daily throughout pregnancy and postpartum. She breastfed extensively, except for occasional formula feedings by others. At 6 months of age, a pediatrician found the infant to be healthy with normal growth and development.[16]
An uncontrolled online survey compiled data on 930 mothers who nursed their infants while taking an antidepressant. Infant drug discontinuation symptoms (e.g., irritability, low body temperature, uncontrollable crying, eating and sleeping disorders) were reported in about 10% of infants. Mothers who took antidepressants only during breastfeeding were much less likely to notice symptoms of drug discontinuation in their infants than those who took the drug in pregnancy and lactation.[17]
A cohort of 247 infants exposed to an antidepressant in utero during the third trimester of pregnancy were assessed for poor neonatal adaptation (PNA). Of the 247 infants, 154 developed PNA. Infants who were exclusively given formula had about 3 times the risk of developing PNA as those who were exclusively or partially breastfed. Fifty-one of the infants were exposed to citalopram in utero.[18]
A case-control study in Israel compared 280 infants of nursing mothers taking long-term psychotropic drugs to the infants of 152 women taking antibiotics. Infant sleepiness at 4 days of age was reported by 1 mother taking citalopram during pregnancy and breastfeeding and by none taking antibiotics. The sleepiness resolved within 24 hours with no developmental effect.[19]
A mother with mixed anxiety-depressive order was taking sertraline and breastfeeding her 9-month-old infant. Because of side effects, sertraline was stopped and citalopram 10 daily was started. After 2 weeks of therapy, she reported signs of bruxism in her infant who was breastfed 5 to 6 times daily, as well as supplementary feedings such as fruits, vegetables, meat, and biscuits. The infant had sporadic, pulsatile, and momentary movements in her jaws, which usually began with movements of the head, especially during sleep. Furthermore, the mother mentioned her child had a habit of biting and clenching her teeth while awake. Pediatric and dental examinations found no abnormalities, but the dentist observed bruxism during the examination. Citalopram was discontinued and bruxism symptoms resolved after 72 hours. The mother resumed breastfeeding with no return of symptoms and the infant had no bruxism symptoms for the next 2 years.[20] Bruxism was probably caused by citalopram in breastmilk.
Effects on Lactation and Breastmilk
The SSRI class of drugs, including citalopram, can cause increased prolactin levels and galactorrhea in nonpregnant, nonnursing patients.[21-25] In a study of cases of hyperprolactinemia and its symptoms (e.g., gynecomastia) reported to a French pharmacovigilance center, fluvoxamine was found to have a 3.9-fold increased risk of causing hyperprolactinemia compared to other drugs.[26] The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
In a small prospective study, 8 primiparous women who were taking a serotonin reuptake inhibitor (SRI; 3 taking fluoxetine and 1 each taking citalopram, duloxetine, escitalopram, paroxetine or sertraline) were compared to 423 mothers who were not taking an SRI. Mothers taking an SRI had an onset of milk secretory activation (lactogenesis II) that was delayed by an average of 16.7 hours compared to controls (85.8 hours postpartum in the SRI-treated mothers and 69.1 h in the untreated mothers), which doubled the risk of delayed feeding behavior in the untreated group. However, the delay in lactogenesis II may not be clinically important, since there was no statistically significant difference between the groups in the percentage of mothers experiencing feeding difficulties after day 4 postpartum.[27]
A case control study compared the rate of predominant breastfeeding at 2 weeks postpartum in mothers who took an SSRI antidepressant throughout pregnancy and at delivery (n = 167) or an SSRI during pregnancy only (n = 117) to a control group of mothers who took no antidepressants (n = 182). Among the two groups who had taken an SSRI, 33 took citalopram, 18 took escitalopram, 63 took fluoxetine, 2 took fluvoxamine, 78 took paroxetine, and 87 took sertraline. Among the women who took an SSRI, the breastfeeding rate at 2 weeks postpartum was 27% to 33% lower than mother who did not take antidepressants, with no statistical difference in breastfeeding rates between the SSRI-exposed groups.[28]
An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge.[29] The antidepressants used by the mothers were not specified.
A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575; citalopram n = 139) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis.[30]
In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned.[31]
Alternate Drugs to Consider
References
- 1.
- Franssen EJ, Meijs V, Ettaher F, et al. Citalopram serum and milk levels in mother and infant during lactation. Ther Drug Monit 2006;28:2-4. [PubMed: 16418683]
- 2.
- Erol S, Ozcan B, Celik IH, et al. Neonatal abstinence syndrome due to prenatally citalopram exposure: A case report. Arch Argent Pediatr 2017;115:e424-e427. [PubMed: 29087127]
- 3.
- Larsen ER, Damkier P, Pedersen LH, et al. Use of psychotropic drugs during pregnancy and breast-feeding. Acta Psychiatr Scand Suppl 2015;445:1-28. [PubMed: 26344706]
- 4.
- Uguz F. A new safety scoring system for the use of psychotropic drugs during lactation. Am J Ther 2021;28:e118-e126. [PubMed: 30601177]
- 5.
- Grzeskowiak LE, Leggett C, Costi L, et al. Impact of serotonin reuptake inhibitor use on breast milk supply in mothers of preterm infants: A retrospective cohort study. Br J Clin Pharmacol 2018;84:1373-9. [PMC free article: PMC5980248] [PubMed: 29522259]
- 6.
- Weissman AM, Levy BT, Hartz AJ, et al. Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. Am J Psychiatry 2004;161:1066-78. [PubMed: 15169695]
- 7.
- Schmidt K, Olesen OV, Jensen PN. Citalopram and breast-feeding: Serum concentration and side effects in the infant. Biol Psychiatry 2000;47:164-5. [PubMed: 10664835]
- 8.
- Heikkinen T, Ekblad U, Kero P, et al. Citalopram in pregnancy and lactation. Clin Pharmacol Ther 2002;72:184-91. [PubMed: 12189365]
- 9.
- Berle JØ, Steen VM, Aamo TO, et al. Breastfeeding during maternal antidepressant treatment with serotonin reuptake inhibitors: Infant exposure, clinical symptoms, and cytochrome P450 genotypes. J Clin Psychiatry 2004;65:1228-34. [PubMed: 15367050]
- 10.
- Weisskopf E, Panchaud A, Nguyen KA, et al. Simultaneous determination of selective serotonin reuptake inhibitors and their main metabolites in human breast milk by liquid chromatography-electrospray mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 2017;1057:101-9. [PubMed: 28511118]
- 11.
- Pogliani L, Baldelli S, Cattaneo D, et al. Selective serotonin reuptake inhibitors passage into human milk of lactating women. J Matern Fetal Neonatal Med 2019;32:3020-5. [PubMed: 29557689]
- 12.
- Schoretsanitis G, Augustin M, Sassmannshausen H, et al. Antidepressants in breast milk; Comparative analysis of excretion ratios. Arch Womens Ment Health 2019;22:383-90. [PubMed: 30116895]
- 13.
- Hendrick V, Smith LM, Hwang S, et al. Weight gain in breastfed infants of mothers taking antidepressant medications. J Clin Psychiatry 2003;64:410-2. [PubMed: 12716242]
- 14.
- Lee A, Woo J, Ito S. Frequency of infant adverse events that are associated with citalopram use during breast-feeding. Am J Obstet Gynecol 2004;190:218-21. [PubMed: 14749663]
- 15.
- Gentile S, Vozzi F. Consecutive exposure to lamotrigine and citalopram during pregnancy. Arch Womens Ment Health 2007;10:299-300. [PubMed: 17763980]
- 16.
- Werremeyer A. Ziprasidone and citalopram use in pregnancy and lactation in a woman with psychotic depression. Am J Psychiatry 2009;166:1298. [PubMed: 19884241]
- 17.
- Hale TW, Kendall-Tackett K, Cong Z, et al. Discontinuation syndrome in newborns whose mothers took antidepressants while pregnant or breastfeeding. Breastfeed Med 2010;5:283-8. [PubMed: 20807106]
- 18.
- Kieviet N, Hoppenbrouwers C, Dolman KM, et al. Risk factors for poor neonatal adaptation after exposure to antidepressants in utero. Acta Paediatr 2015;104:384-91. [PubMed: 25559357]
- 19.
- Kronenfeld N, Ziv Baran, T, Berlin M, et al. Chronic use of psychotropic medications in breastfeeding women: Is it safe? PLoS One 2018;13:e0197196. [PMC free article: PMC5962050] [PubMed: 29782546]
- 20.
- Akbarzadeh F, Behravan G, Modaresi F, Eslamzadeh M. Citalopram-induced sleep bruxism in a breastfed infant: A case report. Front Psychiatry 2023;14:1051346. [PMC free article: PMC9936515] [PubMed: 36816404]
- 21.
- Egberts AC, Meyboom RH, De Koning FH, et al. Non-puerperal lactation associated with antidepressant drug use. Br J Clin Pharmacol 1997;44:277-81. [PMC free article: PMC2042834] [PubMed: 9296322]
- 22.
- González Pablos E, Minguez MartÍn L, Hernández Fernández M, Sanguina Andrés RM. [A clinical case of galactorrhoea after citalopram treatment]. Actas Esp Psiquiatr 2001;29:414. [PubMed: 11730581]
- 23.
- Koch HJ, Zellmer H. Marked mydriasis and neuritis nervi optici associated with galactorrhea following citalopram treatment: A case report and discussion. Case Rep Med 2011;2011:191735. [PMC free article: PMC3160104] [PubMed: 21869891]
- 24.
- Belli H, Vardar MK, Yesilyurt S, et al. Citalopram related euprolactinaemic galactorrhoea: A case report. West Indian Med J 2010;59:100-1. [PubMed: 20931925]
- 25.
- Türkoğlu S. Citalopram-induced galactorrhea in an adolescent. Clin Neuropharmacol 2016;39:331. [PubMed: 27438185]
- 26.
- Trenque T, Herlem E, Auriche P, Drame M. Serotonin reuptake inhibitors and hyperprolactinaemia: A case/non-case study in the French pharmacovigilance database. Drug Saf 2011;34:1161-6. [PubMed: 22077504]
- 27.
- Marshall AM, Nommsen-Rivers LA, Hernandez LL, et al. Serotonin transport and metabolism in the mammary gland modulates secretory activation and involution. J Clin Endocrinol Metab 2010;95:837-46. [PMC free article: PMC2840848] [PubMed: 19965920]
- 28.
- Gorman JR, Kao K, Chambers CD. Breastfeeding among women exposed to antidepressants during pregnancy. J Hum Lact 2012;28:181-8. [PubMed: 22344850]
- 29.
- Venkatesh KK, Castro VM, Perlis RH, Kaimal AJ. Impact of antidepressant treatment during pregnancy on obstetric outcomes among women previously treated for depression: An observational cohort study. J Perinatol 2017;37:1003-9. [PMC free article: PMC10034861] [PubMed: 28682318]
- 30.
- Leggett C, Costi L, Morrison JL, et al. Antidepressant use in late gestation and breastfeeding rates at discharge from hospital. J Hum Lact 2017;33:701-9. [PubMed: 28984528]
- 31.
- Grzeskowiak LE, Saha MR, Nordeng H, et al. Perinatal antidepressant use and breastfeeding outcomes: Findings from the Norwegian Mother, Father and Child Cohort Study. Acta Obstet Gynecol Scand 2022;101:344-54. [PMC free article: PMC9564556] [PubMed: 35170756]
Substance Identification
Substance Name
Citalopram
CAS Registry Number
59729-33-8
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Escitalopram.[Drugs and Lactation Database (...]Review Escitalopram.. Drugs and Lactation Database (LactMed®). 2006
- Review Paroxetine.[Drugs and Lactation Database (...]Review Paroxetine.. Drugs and Lactation Database (LactMed®). 2006
- Review Fluoxetine.[Drugs and Lactation Database (...]Review Fluoxetine.. Drugs and Lactation Database (LactMed®). 2006
- Review Domperidone.[Drugs and Lactation Database (...]Review Domperidone.. Drugs and Lactation Database (LactMed®). 2006
- Review Droperidol.[Drugs and Lactation Database (...]Review Droperidol.. Drugs and Lactation Database (LactMed®). 2006
- Citalopram - Drugs and Lactation Database (LactMed®)Citalopram - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
