NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Institute of Medicine (US) Forum on Medical and Public Health Preparedness for Catastrophic Events. Dispensing Medical Countermeasures for Public Health Emergencies: Workshop Summary. Washington (DC): National Academies Press (US); 2008.
Under the current system, the dispensing of medical countermeasures at the local level is the final step in a complex and interactive process starting with federal, state, and local public health programs. For the system to work effectively, participants must understand the urgent nature of the public health threats, such as anthrax. For example, anthrax produces spores that enter the body through the lungs, mouth, or skin. After the initiation of symptoms, death can occur as quickly as two or three days, with a high percentage of mortality among those infected, said Dr. Sid Baccam of Innovative Emergency Management. Consequently, anthrax exposure requires prophylaxis by oral antibiotics promptly after exposure, optimally within 48 hours, and before symptoms arise. Once someone becomes symptomatic, he or she must be treated because if the individual becomes ill and does not receive timely treatment, the fatality rate approaches 100 percent. Even with supportive care in the hospital, symptomatic inhalational anthrax cases are approximately 50 to 75 percent fatal (CDC, 2003; Inglesby et al., 1999). Therefore, due to the significant risk, standard public health procedures call for erring on the side of prudence and administering antibiotics to everyone who might have been exposed, even before symptoms are apparent.
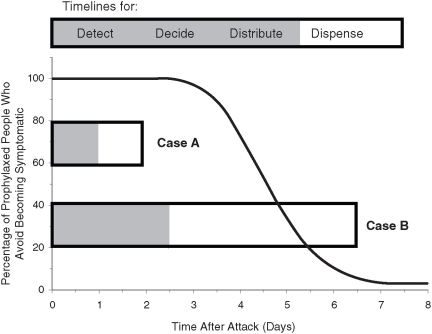
The short time window for preventing illness after anthrax exposure compels the public health system to respond as swiftly as possible to deliver post-exposure prophylaxis (PEP). As described by Baccam, optimal management of the health effects from a bioterrorist attack includes rapid action, progressing in stages known as the four “Ds”: detect, decide, distribute, and dispense. The ability to rapidly detect an anthrax exposure, decide on deployment of the SNS, distribute countermeasures to state and local health authorities, and dispense to affected populations within 48 hours of the decision to do so requires herculean efforts.
In the anthrax scenario, the federal government is responsible for procuring and stockpiling the antibiotics (among other countermeasures), according to legislation requiring CDC to establish SNSs of medical countermeasures throughout the country. Once the attack is detected and the decision is made to transfer stockpiled antibiotics to the states, state governments distribute antibiotics within their borders to pre-designated sites established primarily by local governments as “points of dispensing” (PODs). Most local governments, their partners, or other organizations expect to dispense the majority of countermeasures from PODs to large groups of people. Each locally designated POD, in other words, receives its countermeasures from state authorities, which in turn have received them from the SNS (CDC, 2008).
This workshop focused on the final step in the process: medical countermeasure dispensing from PODs and via alternative mechanisms to their populations. Public health planners have used PODs as the major framework for planning countermeasures dispensing, yet PODs pose some of the greatest challenges, including their location, design, operations, capacity, workforce, and a host of other factors.
Dispensing Medical Countermeasures: Time Considerations
The foremost problems arise from delays in starting and completing the initial dispensing of prophylaxis. Speaker Baccam illustrated that even short delays have striking effects on morbidity and mortality, according to various models (Baccam and Boechler, 2007). At the local level, where dispensing occurs, the degree of morbidity and mortality is impacted by at least three factors: (1) the time of onset of a post-exposure prophylaxis campaign (i.e., the time to deliver the initial pill), (2) the capability in completing the campaign (i.e., the time to deliver the last pill), and (3) the capacity of nearby hospitals to treat symptomatic patients. Symptomatic people need to be treated in hospitals. A community with limited hospital bed capacity will be completely overwhelmed with a high caseload and thereby experience greater mortality.
The three local factors were modeled by Baccam in hypothetical scenarios shown in Figure 1. In Case A, which is the most effective case, the prophylaxis campaign starts on Day 1 and is completed by Day 2. In Case B, the campaign starts on Day 2.5 and is less efficient, taking 4 days to complete. The unmarked black line in Figure 1 illustrates the time frame over which infected people, if there is no prophylaxis campaign, will progress from the incubation period to becoming symptomatic. In the absence of PEP, all infected people become symptomatic (Inglesby et al., 1999). In Case A, 100 percent of infected people are still in the incubation stage when they receive prophylaxis; they are prevented from becoming symptomatic and thus do not need hospital care. In Case B, nearly 100 percent of infected people are still in the incubation period when the campaign is started, but they become symptomatic due to the inefficiency of the PEP campaign. This lack of efficiency is, in other words, linked to how many people are served by the PODs and other methods over a set period of time, that is, the throughput. The consequence of delays in starting the PEP campaign—and the longer duration of initiation of the PEP campaign in Case B—is that more than 50 percent of infected persons become symptomatic and thus need hospital care, noted Baccam. Whether their lives will be saved depends on the community’s hospital capacity and availability of treatment. The end result of these two hypothetical scenarios is that a delay of a mere 1–2 days in start-up time has profound effects on the efficacy of the campaign, with up to 50 percent more morbidity and mortality in the hypothetical cases depicted here (see also Baccam and Boechler, 2007). However, degeneration of the hospital capability is not fully represented in its impact.
Another speaker, Dr. Nathaniel Hupert of Weill Cornell Medical College, discussed the relationship between the expected surge in hospital admissions after an anthrax attack and the tactics used in POD-based antibiotic dispensing campaigns. His model, the Regional Hospital Caseload Calculator, uses two factors to determine outcomes: the delay until starting dispensing (or “time to first pill”) and the duration of the campaign once started (or “time to last pill”). Within the first week after an anthrax attack, shortening the “time to last pill” can be expected to decrease hospitalizations by 2 to 6 percent for each day saved. Using the Caseload Calculator in conjunction with another Cornell model, the Bioterrorism and Epidemic Outbreak Response Model, he calculated that achieving these reductions in hospitalization may require up to a 33 percent increase in POD throughput, which will have important human resource implications for preparedness planning.
POD Models
Cities Readiness Initiative
The focus of the federal efforts to dispense medical countermeasures has been through the Strategic National Stockpile, as described by Burel. “12-hour push packs” are in place near major population centers. One of CDC’s core functions related to stockpiling is to advance the CRI.4 As recently as 2003, there were few PODs and no alternative dispensing sites, which are crucial to enhancing dispensing capacity. The goal of the CRI is to provide, in concert with responsible jurisdictions, mass prophylaxis to 100 percent of an exposed or potentially exposed population within 48 hours of the decision to do so. Today, the CRI has extended its reach to 72 locations covering 57 percent of the U.S. population, Burel said. Those cities have already designated 3,500 PODs. The CRI is strengthening POD infrastructure with state and local partners through technical assistance, including training, electronic mailing lists (listservs), management practices, education of the public via satellite broadcasts, and advice on security to enforce public safety around PODs. The CRI is experimenting with POD structures of many types, including “pull” and “push” mechanisms. Pull mechanisms require the general public to come pick up the countermeasure from open PODs, e.g., drive-through clinics or clinics established at schools, where as push mechanisms involve state and local officials pushing the countermeasures out to entities that are then responsible for delivering the countermeasure to specific populations. For example “push” mechanisms through which countermeasures are delivered to residences through social services, such as Meals on Wheels and home health care, or using the U.S. Postal Service to deliver countermeasures to individual residences. Several of these concepts, including pull and push mechanisms are discussed in greater detail in the next section.
Medical and Nonmedical PODs
In addition to the time of initiation and the duration of the campaign, there are a host of other features for localities to consider in the design and operation of their PODs, as discussed by a number of speakers including Baccam, Burel, and Hupert. One is the location of the POD. Localities are expected to position their PODs at accessible sites (typically sites used for voting), such as high schools, large auditoriums, or elementary schools, in ways that best serve the local community. Another key question is who staffs a POD and how many PODs and staff will be required. There are two types of POD designs, medical and nonmedical. A medical POD would mostly be staffed by medical personnel who would primarily be responsible for dispensing medication and conducting medical exams and triage procedures to determine whether cases are in the incubation stage or in need of hospitalization. In contrast, a nonmedical POD would be staffed by trained but nonmedical personnel, who would dispense medication and triage as appropriate, but would not conduct individualized medical assessments.
The medical POD structure is similar to the way that medicines are dispensed in the absence of an emergency, using trained medical professionals to interact with and assess individual patients. Although this model is consistent with current standards of care, medical PODs have several drawbacks, including the need for a large number of medical staff during a time when they will be needed to handle an expected surge of ill patients. Simulations, as well as an actual exercise in Texas, have estimated that a medical POD has a typical throughput of approximately 500 patients per hour, a rate that is likely too slow to prevent mass casualties. In a target city of one million, approximately 6,000 staff (including nearly 2,000 medical personnel) would be needed to complete a medical POD system in two days.
A nonmedical POD system, on the other hand, provides care using a population approach; no individual medical examinations or assessments are conducted. During an emergency, it was noted that the situational standards of care would likely be altered and it may not be possible to screen every individual based on standards of care that are in place during nonemergency situations. As described by Baccam and other speakers, the value of the nonmedical POD is its increased efficiency. A nonmedical POD can dispense countermeasures to an estimated 2,000 patients per hour, and would need approximately 1,400 staff (including nearly 50 medical personnel) in order to complete mass prophylaxis for a city of one million. Thus nonmedical PODs were described by many workshop participants, including Michael Robbins of the Chicago Department of Public Health, as the preferred approach because they can deliver countermeasures even though every person is not seen by a health professional. Nonmedical PODs can optimally dispense countermeasures at a rate that is approximately four times greater than that of medical PODs, while requiring only approximately one fourth the total number of staff and much fewer medical personnel. Moreover, as mentioned above, using nonmedical staff at PODs would allow medical personnel to attend to those who are already symptomatic. A city could also use a range of public service announcements to divert symptomatic people away from PODs and into hospitals, thereby reducing the need for triage at the POD.
However, staffing challenges for nonmedical PODs remain. As speaker Mary Steiner of the Oklahoma City–County Health Department pointed out, even volunteers who have confirmed their willingness to staff a nonmedical POD may not be sufficiently reliable. In her experience from running emergency preparedness exercises, as few as 25 percent of volunteers may actually show up when called. This may suggest the need to staff nonmedical PODs using paid, nonmedical personnel from the public or private sector, such as nonessential state and local employees, Steiner said. Nonmedical PODs need not be uniformly designed across all communities, but should be designed to meet the required throughput and in congruent with larger strategic distribution plans. These are generally state responsibilities, with the POD responsibility resting with local jurisdictions. Coordination and compatibility of the plans are vital to ensure successful operations. Various options can be used to streamline their operations. These types of PODs are oriented toward a “pull” mechanism, a type of dispensing where the exposed and potentially exposed population comes to the POD to pick up medication.
On the other hand, a “push” mechanism refers to a type of dispensing where countermeasures are delivered to individuals at their residence or current location. As discussed by several speakers including Stephanie Dulin of CDC, several communities are implementing push mechanisms by using the U.S. Postal Service to deliver (dispense) a small supply of medical countermeasures to every residence within hours of an attack (Box 2). Postal carriers would deliver a package of medicine, such as a 10-day supply of antibiotics in the case of anthrax prophylaxis, to individual households (not businesses). This method would be part of a layered strategy to take pressure off of open PODs, while also buying significant time to dispense the remainder of the doses through any number of other dispensing mechanisms. This method can reach large numbers of people quickly, allow residents to shelter in place if there are environmental risks, and can be carried out by experts in home delivery (e.g., postal carriers). In fact, a pilot test of the U.S. Postal Service model has shown that approximately 55,000 housing units can be reached within nine hours from the start of deliveries by 48 postal carriers (Box 2). However, state and local health officials still have concerns regarding the feasibility of the U.S. Postal Service plan—for example with regard to the impact of personal protective equipment on postal carrier effectiveness and the feasibility of obtaining necessary security details.5
In the event of an anthrax attack, most communities plan to dispense enough antibiotics to a person or family to provide coverage for the first 10 days after an incident, thereby buying time for a second wave of dispensing. A quick-strike capability could be conducted through traditional pull mechanisms such as PODs, through push mechanisms such as the U.S. Postal Service (Box 2), or by allowing pre-positioning of a MedKit (a personal antibiotic cache which could contain a few days’ supply of countermeasures) in individual homes. Dispensing of continued countermeasures would be accomplished through other sources (including pull mechanisms). In the case of anthrax, continued countermeasure dispensing would be needed to ensure that the remainder of the necessary 60-day course of prophylaxis was administered to the at-risk populations. One single innovation is unlikely to fit all communities. Multiple options, including PODs of many types, are needed to spur innovation at the community level, Baccam said.
In summary, a number of different dispensing modalities were discussed at the workshop (Box 3).
Additional Challenges
Many challenges were discussed throughout the workshop. As will be summarized in greater detail below, David Henry of the National Governors Association, Scott Mugno of FedEx Express, and others highlighted the need to provide liability protection for those who dispense medications, and to ensure that skilled staff, whether medical or non-medical, are staffing the PODs. Other significant challenges include recruiting and retaining enough personnel or volunteers to meet POD staffing requirements and coordinating across and within the private and public sectors, including law enforcement. Local planners encounter similar obstacles, said Christopher Hoff of Illinois’ Kane County Health Department. He underscored the problem of fragmented, disorganized social support systems for vulnerable populations at the local level, not to mention at the state and federal levels. Fragmentation is compounded when serving local groups with special needs, including the elderly, individuals with mental illness, and children. Local staff service providers are already heavily tasked; they suffer from high turnover rates and reduced funding (whether from federal, state, tribal, or local coffers), all of which present obstacles to an organized system of countermeasure dispensing. Hoff envisioned pull mechanisms for able-bodied individuals and push mechanisms for special needs populations. In summary, the integration of federal, state, tribal, and local efforts to distribute and dispense medical countermeasures is essential.
The most difficult issues arise at the local level, according to many workshop participants. Summarizing the discussion, Lisa Koonin of CDC highlighted the major gaps and challenges to be considered (Box 4). The main challenge is that few communities have existing mechanisms to comprehensively dispense countermeasures. Helping them to develop new programs or adapt existing ones is integral to the success of the entire public health undertaking. As suggested by Eva Lee of the Georgia Institute of Technology, conducting preparedness exercises and publishing evaluation results could provide both a starting point and an incentive for improvement. The most important measure of success, expressed by several presenters, is in terms of lives saved. The next section of this workshop summary is devoted to near-term solutions to deal with the challenges in dispensing countermeasures.
Footnotes
- 4
For more information about the CRI, visit http://www
.bt.cdc.gov/CRI/. - 5
Text in the prepublication version was modified to reflect state and local concerns more accurately.
Figures
Boxes
BOX 2 U.S. Postal Service Plan
Recognizing that points of dispensing may not be able to reach the entire at-risk population within 48 hours, a new federally sponsored program was designed to provide a “quick strike.” Initiated in 2004, the program is conducted by the U.S. Postal Service (USPS) using postal carriers to dispense to residences a short-term supply of medical countermeasures. The program was developed and later pilot tested under the auspices of the Centers for Disease Control and Prevention’s (CDC’s) Cities Readiness Initiative.
The main features of the USPS program are:
- Outfitting postal carriers and other volunteers with personal protective equipment, including respirators, protective gloves, and disposable clothing;
- Providing USPS employee volunteers and their families appropriate counseling, training, and prophylaxis prior to onset of dispensing a ;
- Ensuring that postal carriers have security escorts;
- Initiating the program through tactical planning within the USPS and with federal, state, and local governments;
- Accomplishing direct delivery/dispensing of countermeasures within 12 hours of the decision to start the program; and
- Conducting drills that allow for real-world adjustments to improve efficiency and effectiveness.
Drills were conducted in 2006 and 2007 across two to three ZIP Codes in three cities: Seattle, Boston, and Philadelphia. Postal carriers dispensed mock antibiotics to approximately 22,000, 36,000, and 55,000 housing units in the three drills. In these operational drills, dispensing of medications took only 6–9 hours, although the postal carriers did not wear personal protective equipment. The success of these drills provided evidence that the system could work.
- a
This bullet was expanded after release of the prepublication version to reflect additional features of the program.
BOX 3 Potential Dispensing Modalities
Points of dispensing (PODs): The PODs concept was initially developed to address the smallpox threat and is the public health-preferred method of providing vaccine prophylaxis at designated dispensing locations for persons who are currently healthy, but may have been “exposed.” The role of the PODs has been extended to dispense oral antibiotics.
Home delivery by the U.S. Postal Service (USPS) or other groups: Home delivery of antibiotics by the USPS was conceptualized as a way to increase the speed of dispensing self-administered medical countermeasures and to reduce the population surge at PODs. With this modality, mail carriers with security escorts deliver antibiotics directly to homes. Other novel dispensing methods may exist, such as utilizing newspaper delivery carriers.
Pre-deployment of community-based caches of medications: Pre-deployment of antibiotics to community-based caches might include houses of worship, schools, large employers, or fraternal organizations. This option may include the development of retail PODs (operated by retail businesses to provide medical countermeasures to their employees and the public) or closed PODs (operated by organizations to provide medical countermeasures to their employees and their family members).
Pre-positioning to first responders: Pre-event dispensing to first responders could mean that critical personnel and/or volunteers would be issued antibiotics after being identified and trained.
Pre-positioning of medications in households: Pre-event placement of caches of antibiotics or other medical countermeasures (MedKits) in households are to be reserved for use during a declared public health emergency. A pilot study was conducted in St. Louis to test the feasibility of MedKits in households. While some consider the study a success, further studies are needed to ensure safety and prevent misuse before implementing a wide scale MedKit program. The provision of MedKits is currently under discussion with the Food and Drug Administration.
BOX 4Potential Gaps and Challenges in Current Methods of Dispensing Countermeasures
Workforce: Staffing requirements for points of dispensing (PODs) mandate a large number of personnel.
High-touch activity: Each person who receives medications from PODs must have several interactions with POD staff, which takes time.
Need for volunteer training: Volunteers would need training prior to an event, as well as guidance during an event.
Need for medical surveillance for volunteers: Assurance is needed that volunteers remain healthy during POD operations.
Security needs: Crowds must be controlled to maintain order around and within POD facilities.
Patient tracking/registries: Systems are needed to account for all persons served at PODs.
Rapid time frame: Optimally PODs would dispense countermeasures to a large population within 48 hours of the decision to initiate dispensing.
Lack of coordination among agencies in community: Often communication and coordination are lacking within various sectors of the community.
Lack of framework: A framework to engage private-sector templates and tools is not available to guide private-sector engagement.
Liability issues: Private-sector volunteers and entities would need protection against liability to participate in the care of others.
Leadership: In some jurisdictions bioterrorism preparedness is not a top priority and therefore no one is assigned to lead activities if an event occurs.