NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990.
Evaluation of the gastrointestinal tract requires careful history and physical examination techniques. Though sophisticated laboratory tests or radiographic or endoscopic procedures may be necessary to confirm a diagnosis of intra-abdominal pathology, the initial diagnosis is usually suspected from the history and reinforced by physical examination. Most important, therapeutic decisions for intra-abdominal inflammatory processes are based mainly on findings that can be elicited only by careful physical examination. Thus, though physical examination of the abdomen is difficult, it is a skill that must be mastered for proper management of these patients.
History
Table 80.1 lists symptoms of gastrointestinal disease. Pain is the most common complaint related to abdominal problems. Important points to cover with the patient are the location and duration of the pain, any change in its location or intensity, any known precipitating factors, and any associated symptoms (fever, chills, nausea, vomiting, or change in bowel habits). One must also inquire as to associated abdominal findings such as bloody stools, melena, or abdominal distention.
Once the examiner has a clear idea of the present illness, he or she should inquire as to previous such episodes of illness or similar illnesses. A brief history of previous illnesses, acute or chronic, may be helpful, and a review of all previous operations, medications, and allergies is imperative.
Physical Examination
Table 80.2 presents the sequence of steps for examining the gastrointestinal system. No special instruments are required for examination of the abdomen. Good lighting and a stethoscope are all that is needed. Common abnormalities that may be disclosed during the examination are listed in Table 80.3.
For convenience, the abdomen is divided into quadrants (Figure 80.1) and areas (Figure 80.2). The umbilicus is the central point of the abdomen dividing right from left, upper from lower. Masses found on inspection or palpation, or tenderness found on palpation, are described according to the quadrant in which they are found. For example, the swollen gallbladder of acute cholecystitis may cause a tender mass in the right upper quadrant. It is thus important to relate the quadrants of the abdomen to the underlying organs (Figure 80.3).
Inspection
The patient is placed supine on an examining table or bed. It is helpful to place a small pillow beneath the knees to relax the abdominal musculature. The head should rest comfortably on a small pillow. The patient's arms should rest comfortably at the sides. Drapes should be placed over the breasts and groins just below the inguinal regions to preserve modesty. The examiner stands on the patient's right.
The general contour of the abdomen is examined for any abnormalities. Notice is made as to whether the abdomen is distended or scaphoid, whether there is any bulging in the flanks, and whether the umbilicus is inverted or everted. The skin of the abdominal wall is examined carefully for hemangiomas or the dilated veins of a caput Medusa, both indicative of severe liver disease. The skin should also be examined carefully for scars, correlating these with previous operations.
Each quadrant of the abdomen is next carefully inspected for any visible masses. The abdominal wall is inspected carefully during respiration for any asymmetry of motion. Any such asymmetry may well be due to muscular rigidity from underlying inflammation.
All surgical scars are carefully inspected for bulges, which may indicate herniation. The patient should be asked to cough to check again for herniation. Similarly, one should inspect the inguinal and femoral regions for herniation during normal respiration and during cough.
Auscultation
In abdominal examination auscultation is performed before palpation, as palpation may alter the bowel sounds. Starting in the right upper quadrant, the examiner listens over the liver for rubs or bruits and over the free abdominal wall for bowel sounds. One moves next to the left upper quadrant, again listening for bowel sounds and then over the spleen to detect rubs or bruits. One should next auscultate in the periumbilical regions for aortic or renal bruits and for bowel sounds and then in the left and right lower quadrants for bowel sounds or iliac bruits. If, during the course of auscultation, no bowel sounds are detected, one should auscultate in the periumbilical region for 3 full minutes before determining that bowel sounds are absent. Important points to note on bowel sounds are the pitch, intensity, and duration of the sounds. Any bruits noted should be carefully localized to the loudest point as this relates to the origin of the bruit.
Palpation
Palpation of the abdomen involves using the flat of the hand and fingers, not the fingertips (Figure 80.4) to detect palpable organs, abnormal masses, or tenderness. Again, an orderly approach is necessary to prevent oversights. One should begin in the right upper quadrant with palpation of the liver. The flat of the right hand is placed on the abdominal wall with the fingertips pointing toward the right shoulder. The fingertips should be 2 to 3 cm below the costal margin (Figure 80.5). The patient is asked to inspire deeply, bringing the liver edge down to the fingertips. One should note the consistency of the liver and whether there is tenderness. It should be noted whether the edge of the liver is sharp, blunted, or nodular. The examiner's hand may be moved along the liver edge, outlining the size of the liver. An alternative method of palpating the liver is to hook the fingers around the costal margin and have the patient inspire deeply to bring the liver edge down (Figure 80.6). This technique is particularly effective in patients with normal liver size.
After the liver is examined, one palpates the right upper quadrant for masses or tenderness. Again, one uses the flat of the hand and fingers for palpation. If any mass is noted, it often is helpful to outline the mass by using two-handed palpation. The left hand is used to push down on the right hand and thus overcome the abdominal musculature and examine the mass (Figure 80.7). If no mass is noted, one moves on to the left upper quadrant. Again, one palpates carefully for masses or tenderness in the left upper quadrant. An attempt should be made at palpation of the spleen in the same fashion as the liver. The normal spleen will be palpable in only the thinnest of individuals. If the spleen is not palpable in the supine position, the patient is turned to the right lateral position. The examiner stands on the patient's right and palpates with the right hand while using the left hand to exert pressure on the patient's left flank (Figure 80.8). This pushes the spleen anteriorly and often makes it palpable.
One next moves to the periumbilical region, again palpating for mass or tenderness. One should be particularly cognizant of the aortic bifurcation being at the umbilicus so that an aortic aneurysm will commonly present as a pulsatile mass at or just above the umbilicus. The umbilicus itself should be carefully palpated for detection of herniation or lymphadenopathy.
The left lower quadrant and flank are next palpated. The lower pole of the left kidney may be palpable in thin individuals as a firm, rounded, smooth mass in the left flank. The sigmoid colon may be palpable as a tubular structure low in the left lower quadrant. Note should be made of any tenderness or abnormal masses in the left lower quadrant. Attention is next directed to the right lower quadrant and flank. As on the left, the lower pole of the right kidney may be palpable in the right flank. The cecum may be palpable in thin individuals as a fluctuant, poorly defined mass low in the right lower quadrant. Again, note must be made of any abnormal mass or tenderness.
Special attention is next directed to incisional scars. The patient is asked to cough or perform a Valsalva maneuver as the scars are palpated to check for any incisional herniation. Similarly, the inguinal and femoral regions are palpated during cough or Valsalva for detection of hernia.
Percussion
Percussion of the abdomen is performed to check liver size, spleen size, and any abnormal gas collections. The size of the liver is estimated by determining the span of liver dullness by percussion. This is performed by percussing just below the breast in the midclavicular line. A resonant note should be obtained because of the underlying air (Figure 80.9). Percussion then proceeds caudally from the dome of the liver until dullness is noted. Percussion is then continued caudally until resonance returns, indicating that the examiner has reached the hepatic flexure of the colon at the hepatic edge (Figure 80.10). A normal liver span is 10 to 12 cm. If dullness is absent over the liver, this may be a sign of intra-abdominal gas, as might occur with a perforated viscus.
Using a similar technique, percussion can be used to outline the size of the spleen. Percussing in the midaxillary line, the normal splenic dullness can be detected from the ninth to the eleventh intercostal space. If the dullness encompasses a larger area, splenomegaly is usually present. Percussion is next performed in the right upper quadrant to check for gas within the hepatic flexure, in the left upper quadrant to check for gas in the stomach or the splenic flexure, in the left lower quadrant to check for gas in the sigmoid, in the right lower quadrant to check for gas in the cecum. Percussion in the periumbilical region should delineate the presence of gas within small bowel loops. Any mass that has been noted on inspection or palpation of the abdomen should also be carefully percussed at this time to determine if there is gas within that mass. This would be indicative of the mass either being a distended loop of bowel or of free intraperitoneal air.
Ascites should be searched for carefully, especially if the patient has bulging flanks or a protuberant abdomen. The most informative examination for the presence or absence of ascites is a search for shifting dullness. This is performed by beginning in the flank with percussion and proceeding anteriorly until the note changes from dull to tympanitic, indicating that bowel loops have been reached. This area is marked with a pen and then the patient is rotated toward that flank to allow fluid to shift anteriorly. The examination is then repeated. Where the note changes from dullness to tympany is again marked. A change from the previous mark indicates free intra-abdominal fluid (Figure 80.11).
Another test that is helpful in identifying ascites is the presence of a fluid wave. The patient or an assistant indents the anterior abdominal wall in the midline; the examiner places the flat of the hand against one flank and then taps gently on the other flank with a finger. If significant ascites is present, a fluid wave should be transmitted from the tapping finger to the receptive hand (Figure 80.12).
Rectal Examination
The patient is next asked to turn to the left lateral decubitus position with the right hip and knee fully flexed and the left hip and knee slightly flexed. The gluteal region should be at the edge of the examining table. The anal area is then carefully examined for any skin lesions, scars, fistula tracts, or external hemorrhoids. The gloved right index finger is then well lubricated and inserted anally. Resistance at the anal ring is usually due to spasm caused by nervousness and may be overcome by asking the patient to strain as the finger is inserted. The anal wall is carefully palpated, taking note of any hypertrophic apaillae, inflamed crypts, strictures, and for sphincter tone. The fingertip then palpates the rectum to check for any rectal mass and for the condition of the prostate.
Inguinal Region
Examination of the inguinal region is best performed by having the patient stand erect facing the examiner who is seated on a stool. The examiner should inspect the inguinal region for evidence of abnormal protrusions or masses along the course of the spermatic cord into the scrotum (Figure 80.13). If a suspicious mass is detected on inspection, the patient should be asked to cough to see if any additional impulse occurs. He should be asked to attempt to reduce the mass himself if that is possible.
If no mass is evident, the examiner should palpate the inguinal regions. This is best done by inserting the index finger along the spermatic cord inverting the scrotal skin to the pubic tubercle and then sweeping laterally to identify the external ring (Figure 80.14). The subject is then instructed to cough, and if an indirect inguinal hernia is present, the examiner should detect an impulse as the sac proceeds along the inguinal canal to exit at the external ring. If a general bulge is detected in the medial inguinal region, differentiation between direct and indirect inguinal hernia occasionally can be made on physical examination by pressing directly over the internal ring and thereby arresting descent of the indirect hernia (Figure 80.15). If the subject then coughs again and the same protrusion occurs with the internal ring occluded, one can assume that the hernia is a direct hernia through the lower abdominal wall.
One must keep in mind the possibility of femoral hernias in this region. They exit through the femoral canal and present as a bulge below the inguinal ligament. Occasionally a femoral hernia loops cephalad over the inguinal ligament, presenting as a direct or indirect inguinal hernia. Palpation over the femoral canal should confirm the femoral origination of the hernia.
Figures
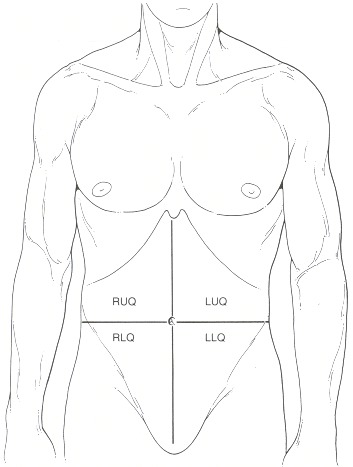
Figure 80.1
The abdominal quadrants; right upper, right lower, left upper, and left lower.
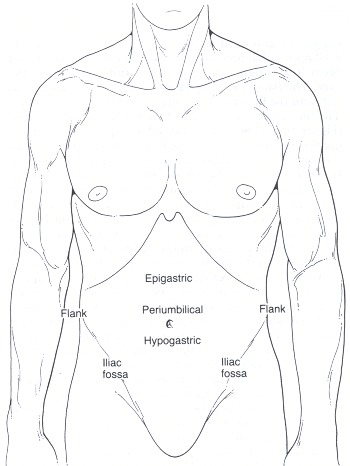
Figure 80.2
The abdominal areas.
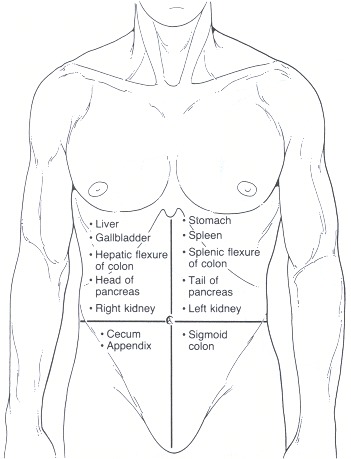
Figure 80.3
Topographic anatomy of the abdomen.
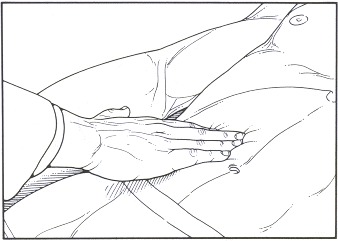
Figure 80.4
Palpation of the abdomen. The flat of the hand and fingers are used for palpation, not the fingertips.
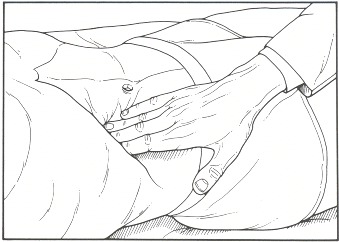
Figure 80.5
Palpation of the liver. The patient inspires deeply, bringing the liver edge to the examiner's fingertips.

Figure 80.6
Alternative method for palpation of the liver. The fingers are hooked around the costal margin. The patient inspires deeply, bringing the liver edge to the fingertips.
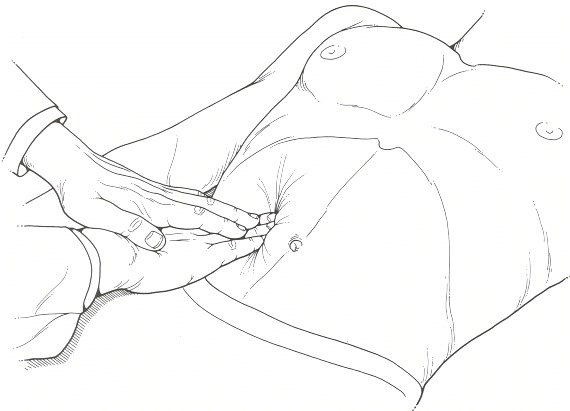
Figure 80.7
Two handed palpation. The left hand is used to push down on the right hand, and thus examine any mass.

Figure 80.8
Palpation of the spleen. The left hand exerts pressure against the left lower rib cage, pushing the spleen anteriorly to be palpated by the right hand.

Figure 80.9
(A) Percussion of liver dullness. (B) Point of highest dullness; the dome of the liver.
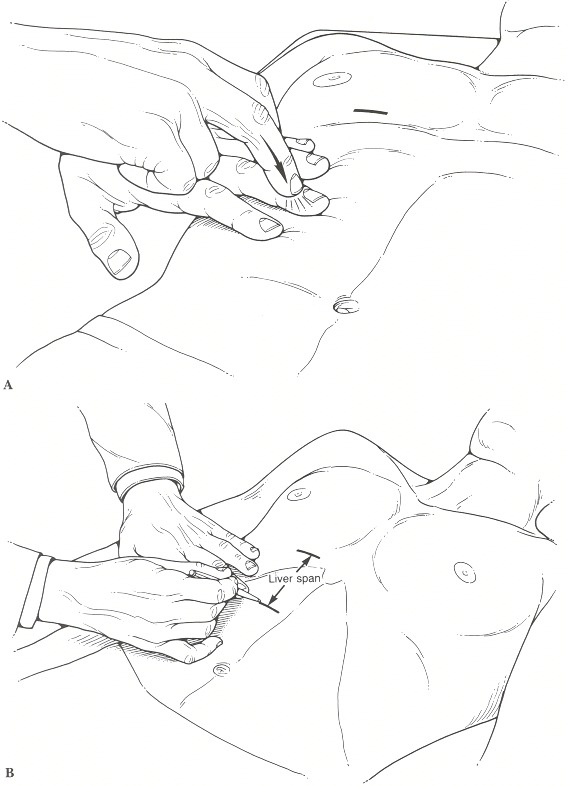
Figure 80.10
(A) Percussion of the liver at the liver edge. (B) Return of resonance marks liver span.
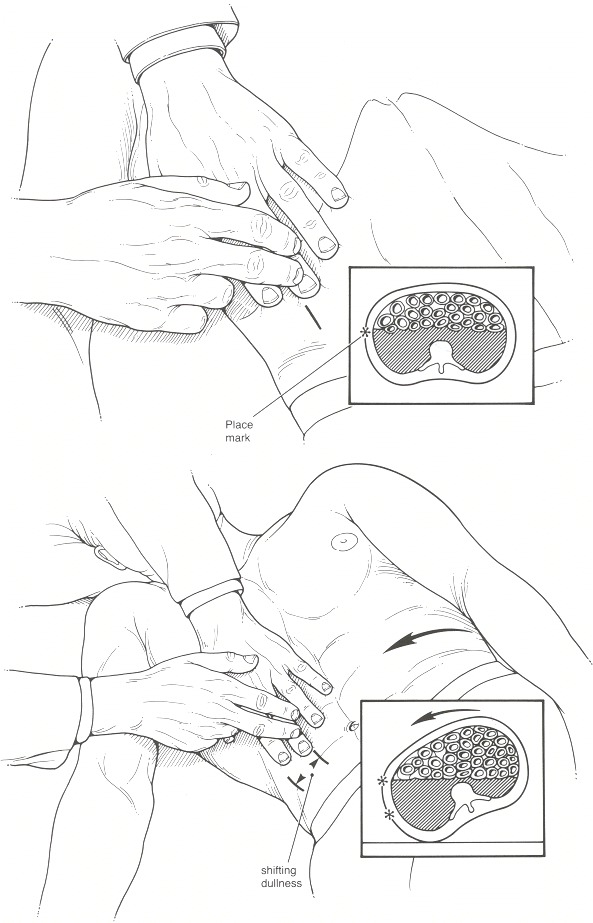
Figure 80.11
Percussion of shifting dullness. See text for explanation.
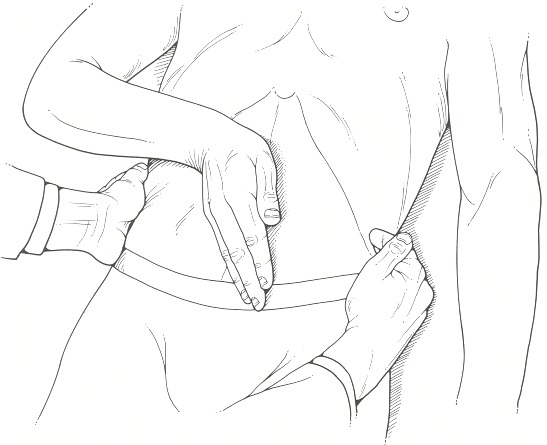
Figure 80.12
Percussion of fluid wave. See text for explanation.
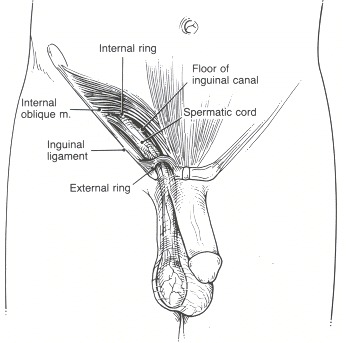
Figure 80.13
Normal inguinal anatomy.
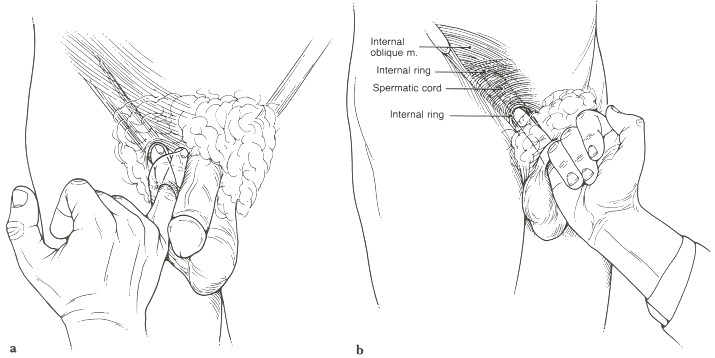
Figure 80.14
Palpation of the inguinal region, (a) The examiner inverts scrotal skin to palpate the inguinal canal. (b) With the finger in the internal ring and inguinal canal, the patient is asked to cough, to check for herniation.
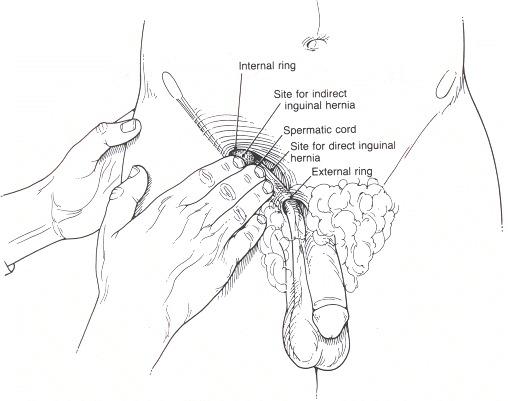
Figure 80.15
Direct compression of the inguinal region to determine site of herniation.
Tables
Table 80.2Sequence of Examination of the Gastrointestinal System
| Step | Position | Chapter |
|---|---|---|
| Inspection | Supine, head and knees supported | 93 |
| Auscultation | Supine, head and knees supported | 93 |
| Palpation | Supine, head and knees supported | 93 |
| Percussion | Supine, head and knees supported | 93 |
| Check for ascites | Supine, may need to roll patient for shifting dullness | 93 |
| Rectal examination | Left lateral decubitus | 97 |
| Inguinal examination | Standing | 96 |
Table 80.3Common Abnormalities of Abdominal Examination
| Anatomical structure | Abnormality | Common condition | Chapter |
|---|---|---|---|
| Umbilicus | Mass or protrusion | Hernia Sister Mary Joseph's node | 93 |
| Prominent veins | Portal hypertension | 93 | |
| Stomach | Mass in left upper quadrant | Gastric carcinoma Gastric outlet obstruction | 93 |
| Pancreas | Mass in right upper quadrant | Pancreatic carcinoma Pancreatic pseudocyst | 93 |
| Gallbladder | Mass in right upper quadrant | Cholecystitis | 93 |
| Carcinoma of gallbladder Hydrops of gallbladder | |||
| Tenderness and guarding in right upper quadrant | Acute cholecystitis | 93 | |
| Small intestine | Decreased bowel sounds | Ileus | 93 |
| Increased bowel sounds | Obstruction | 93 | |
| Colon | Abdominal mass | Carcinoma | 93 |
| Liver | Increased size | Hepatitis Metastatic carcinoma Cirrhosis | 95 |
| Decreased size | Cirrhosis | 95 | |
| Nodularity | Metastatic carcinoma Cirrhosis | 95 | |
| Spleen | Increased size | Acute viral infections Portal hypertension Hemolytic anemia | 93 |
| Peritoneal space | Presence of ascites | Portal hypertension Metastatic carcinoma Congestive heart failure | 93 |
| Anus and rectum | Anal mass | Hemorrhoid Anal carcinoma | 97 |
| Anal inflammatory lesion | Fissure Fistula | 97 | |
| Rectal mass | Rectal carcinoma Benign rectal ulcer | 97 | |
| Inguinal canal | Reducible mass | Direct hernia Indirect hernia Femoral hernia | 96 |