NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Molecular Imaging and Contrast Agent Database (MICAD) [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2004-2013.
| Chemical name: | Gadoxetate |
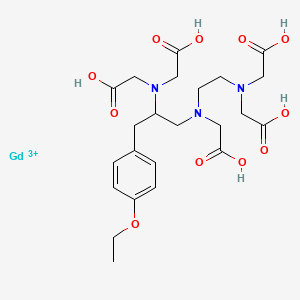
|
| Abbreviated name: | Gd-EOB-DTPA | |
| Synonym: | Eovist®, Primovist™, gadoxetic acid, gadolinium-ethoxybenzyl-diethylenetriaminepentaacetic acid, disodium S-[4-(4-ethoxybenzyl)-3,6,9-tris[(carboxy-KO)methyl]-3,6,9-triazaundecandioato) (5-)-K3N3,N6,N9,K2O1,O11]gadolinite (2-), gadolinium ethoxybenzyl-DTPA, gadoxate disodium | |
| Agent Category: | Compound | |
| Target: | Hepatocyte, liver, biliary tract | |
| Target Category: | Uptake by the hepatocytes | |
| Method of detection: | Magnetic resonance Imaging (MRI) | |
| Source of signal/contrast: | Gadolinium (Gd) | |
| Activation: | No | |
| Studies: |
| Click on the above structure for additional information in PubChem. |
Background
[PubMed]
Gadoxetate (Gd-EOB-DTPA) is a paramagnetic contrast agent developed for tissue contrast enhancement in hepatobiliary magnetic resonance imaging (MRI) (1-3).
Conventional paramagnetic contrast agents are generally metal chelates with unpaired electrons, and they work by shortening both the t1 and t2 relaxation times of surrounding water protons to produce a signal-enhancing effect (4, 5). At normal clinical doses of 0.1−0.2 mmol/kg, the t1 effect tends to dominate. Current agents are water-soluble compounds that distribute in the extracellular fluid and do not cross the intact blood−brain barrier (BBB). They are often used to enhance signals of central nervous system tissues that lack a BBB (e.g., pituitary gland), extraaxial tumors (e.g., meningiomas), and areas of BBB breakdown (e.g., tumor margins). These contrast agents can also be used in a similar nontargeted manner to enhance contrast between pathologies and surrounding normal areas in other organs (4-6).
Gadolinium(III) (Gd3+), a lanthanide metal ion with seven unpaired electrons, has been shown to be very effective at enhancing proton relaxation because of its high magnetic moment and very labile water coordination (5, 7-9). Gadopentetate dimeglumine (Gd-DTPA) was the first intravenous MRI contrast agent used clinically, and a number of similar Gd chelates or Gd-based contrast agents (GBCAs) have since been developed in an effort to further improve clinical efficacy, patient safety, and patient tolerance. The major chemical differences among these Gd chelates are the presence or absence of overall charge, ionic or nonionic, and their ligand frameworks (linear or macrocyclic). They are all non-targeted MRI contrast agents that are used in clinical practice.
Introduction of the lipophilic moiety, ethoxybenzyl, into the Gd chelate Gd-DTPA yielded Gd-EOB-DTPA (1). On i.v. administration, Gd-EOB-DTPA is taken up by both the liver and kidney and excreted into the urine and bile (10, 11). The uptake of Gd-EOB-DTPA by the hepatocytes allows differentiation between the healthy tissue and liver tumor because the tumorous liver tissue accumulates little Gd-EOB-DTPA (10, 12). This specific uptake mechanism is not entirely known because of evidence that the human organic anionic-transporter protein (OATP) is not involved (13). Excretion of Gd-EOB-DTPA in the bile may also permit visualization of both the gall bladder and the bile ducts. Gd-EOB-DTPA is highly soluble in water and exhibits low protein binding. Gd-EOB-DTPA is not commercially available in the United States, but it was approved as a MRI liver contrast agent in Sweden (3). In this formulation (0.25-mmol/ml injection), Gd-EOB-DTPA has an osmolality of 688 mOsm/kg H20 (at 37 ºC), viscosity of 1.19 mPa.s (at 37 ºC), and pH 7.0 (14).
Both renal and extra-renal toxicities have been reported following the clinical use of gadolinium in patients with underlying kidney disease (15-17). In 2007, the US FDA requested manufacturers of all GBCAs to add new warnings about exposure to GBCAs increases the risk for nephrogenic systemic fibrosis (NSF) in patients with advanced kidney disease.
Synthesis
[PubMed]
Schmitt-Willich et al. (2) described a detailed synthesis of Gd-EOB-DTPA by a method that started with the commercially available Nα-benzyloxy-carbonyl-L-tyrosine methyl ester (Z-Tyr-OMe). Two different approaches to prepare the chiral triamine as a key intermediate were developed. For a small-scale synthesis, the protected amino acid Z-Tyr-OMe was O-alkylated at the phenolic function with ethyl iodide in dimethylformamide to yield O-ethyl-Nα-benzyloxycarbonyl-L-tyrosine methyl ester. This was converted to N-(2-aminoethyl)Nα-benzyloxycarbonyl-O-ethyl-L-tyrosinamide hydrochloride. This was then converted into N-(2-aminoethyl)-O-benzyloxycarbonyl-O-ethyl-L-tyrosinamide by aminolysis with an excess of ethylenediamine and followed by catalytic hydrogenation. This was reduced with concentrated diborane/tetrahydrofuran to S-1-(4-ethoxybenzyl)-3-azapentane-1,5-diamine trihydrochloride. For large-scale preparation, instead of aminolysis of tyrosine methyl ester, the ester was reduced to the corresponding alcohol using sodium borohydride in methanol. The obtained chiral triamine from either approach was then converted in two steps into the nonstoichiometric sodium salt (S-EOB-DTPA sodium salt). The complexation of EOB-DTPA with Gd(III) was conducted by adding gadolinium oxide (Gd2O3) to the ligand in water at 80 ºC for 1 h to produce the Gd-EOB-DTPA. The solution was filtered through a 0.2-μm filter, and the pH was adjusted to 7.0 using 1 N sodium hydroxide. The solution was added at 50ºC to ethanol. The mixture was then heated under reflux for 2 h. Precipitation from water/ethanol (85%) yielded a final product with a purity >98% determined by high-performance liquid chromatography (HPLC). Complex formation of pure S-EOB-DTPA with Gd(III) generated a second chiral center. Chiral HPLC found two diastereomers in a ratio of ~65:35.
In Vitro Studies: Testing in Cells and Tissues
[PubMed]
Schuhmann-Giampieri et al. (1) measured the relaxivity of Gd-EOB-DTPA at 0.47 T (20 MHz) at 39 ºC. The t1 relaxivity values of Gd-EOB-DTPA were 5.30 ± 0.33, 8.64 ± 0.47, and 11.2 ± 0.60 liter/mmol·sec in water, plasma, and blood, respectively. It is reported that Gd-EOB-DTPA has a thermodynamic stability of log K = 23.46 (14, 18). In comparison, the value of log K for Gd-DTPA is 22.2.
Muhler et al. (11) studied the acute toxicity of Gd-EOB-DTPA (0.3 mmol/kg) in an in vitro perfused rat liver model and found no significant change in the functional parameters, enzymes, or potassium release in the liver. Pascolo et al. (13) studied the hepatic uptake mechanism of Gd-EOB-DTPA in basolateral rat hepatocyte plasma membrane vesicles (bLPMV). Gd-EOB-DTPA entered bLPMV via a linear, concentration-dependent mechanism through up to 1.5 mM of substrate. Using Xenopus laevis oocytes injected with cRNA that encoded for the human OATP and measuring the OATP transport of Gd-EOB-DTPA, the author suggested that OATP was not involved in the transport of Gd-EOB-DTPA. van Montfoort et al. (19) demonstrated saturable uptake of Gd-EOB-DTPA by the first member (Oatp1) of the polyspecific organic anion transporting polypeptides (Oatps) isolated from the rat liver. The study indicated that Gd-EOB-DTPA was a low-affinity substrate of the rat liver Oatp1.
Lewin et al. (20) evaluated the suitability of Gd-EOB-DTPA as a nonviral vector for gene therapy of hepatocellular carcinoma. Cells suspensions (107 cells) of cultured rat hepatocytes and the hepatoma cells HepG2 and Huh7 were incubated with 25 μmol Gd-EOB-DTPA at 37 ºC for 15−90 min. Gd-EOB-DTPA was specifically taken up by normal rat hepatocytes but not by hepatoma cells. Incubating the cells with plasmids that contain the lacZ reporter gene and polyethyleneimine-Gd-EOB-DTPA resulted in a few transfected cells. The study suggested that the Gd-EOB-DTPA polycation conjugates could serve as transfer vectors of interest for gene-targeting imagery at the early stage of hepatocarcinogenesis. However, the transfer efficiency of the studied conjugate was low and required improvement.
Animal Studies
Rodents
[PubMed]
Muhler and Weinmann (18) used radioactive 153Gd-EOB-DTPA to study the biodistribution and excretion of Gd-EOB-DTPA after repeated i.v. administration to rats. A dose of 50 μmol/kg of 153Gd-EOB-DTPA (a specific activity of 12.3 MBq/mmol(0.33 mCi)/mmol) was administered daily to each rat for 5 days. The injected dose was rapidly cleared from the body. Radioactivity primarily accumulated in the liver and kidneys. Approximately 81.9-82.7% of the injected dose (ID) was excreted in the feces and 17.5−18.2%ID was excreted in the urine within the first 3 days after the last dose. After 21 days, radioactivity was detected only in the kidneys, bone, stomach, and testes. The values (n = 5) were 0.409 ± 0.177, 0.239 ± 0.052, 0.037 ± 0.008 , and 0.033 ± 0.007%ID, respectively. Approximately 0.002 ± 0.177% ID was detected in the whole body. Using 153Gd-EOB-DTPA, Schumann-Giampieri et al. (10, 21) found non-linear pharmacokinetics for Gd-EOB-DTPA after a single i.v. bolus dose of 0.05-0.5 mmol/kg in rats. The total plasma clearance (CL) was 44.5 ± 4.87 (0.05 mmol/kg) to 24.8 ± 2.84 (0.5 mmol/kg) ml/min.kg (n = 10). Plasma binding was 10.3 ± 1.4%. Vmax was 4.34 ± 0.58 μmol/min.kg for the 0.5-mmol/kg dose.
Schuhmann-Glampieri et al. (1) found that the acute i.v. tolerance (LD50) of Gd-EOB-DTPA was 10 mmol/kg in mice and rats. In rat subacute toxicity studies, all rats survived after i.v. doses of 2.5 mmol/kg four times/week for 4 weeks. Vacuolization was observed in the proximal tubuli of the kidneys, an osmotic nephrosis phenomenon that was observed with many other ionic and nonionic contrast agents. The biodistribution studies (0.25 mmol/kg Gd-EOB-DTPA) showed that the renal elimination (n = 5) was 30.5 ± 4.72% ID, and the extrarenal elimination was 62.7 ± 10.9% ID on day 7 after administration. Biliary excretion at 3 h after i.v. administration of 0.05, 0.1, 0.2, 0.5, and 1.5 mmol/kg was 80.3 ± 3.92, 68.9 ± 4.28, 63.4 ± 3.83, 53.1 ± 3.15, and 32.5 ± 5.6%, respectively. This excretion was inhibited by coadministration of sulfobromophthalein ( transported by the organic anion transporter polypeptide system into the hepatocyte). In the rat MRI (2 T) imaging study, the liver signal intensity increased 100% after 10 min. The implanted Novikoff hepatoma was clearly delineated from the normal liver tissue. In a biliary excretion and pharmacokinetics study, Schuhmann-Giampieri et al. (22) showed that the total amount of Gd-EOB-DTPA that underwent biliary excretion 0−90 min after injection was 39.5 ± 11.8% ID. The maximum excretion rate was 9.2 μmol/min per kg for the iinfustion rate of 50 μmol/min per kg. The amount of Gd-EOB-DTPA recovered in bile after the intraduodenal application of 0.1 mmol/kg was 4.61 ± 1.05% ID.
In a comparison study, Van Beers et al. (23) compared the enhancement pattern of rat hepatocellular carcinomas (HCCs) by Gd-EOB-DTPA (0.06 mmol/kg) with 99mTc-iminodiacetic acid (99mTc-IDA; 3−22.2 MBq (0.08-0.6 mCi)). With Gd-EOB-DTPA t1-weighted spin-echo MRI (200 MHz), the peak liver enhancement (relative intensity (RIpost) − RIpre /RIpre × 100) was 127% at 5 min and the peak tumor enhancement was 66% at 5 min. In comparison, the mean 99mTc-IDA radioactivity uptake was 215% ID/100 g in the liver and 95% ID/100 g in the tumor at 5 min after administration. The study concluded that the enhancement pattern of HCCs with Gd-EOB-DTPA was different from that of 99mTc-IDA.
Other Non-Primate Mammals
[PubMed]
In a pharmacokinetics study, Schuhmann-Giampieri, et al. (10, 21) injected bolus doses of 0.03 and 0.25 mm/kg 153Gd-EOB-DTPA into 5 female beagle dogs and found nonlinear pharmacokinetics. The CL was 18.2 ± 3.27 (at the 0.03 mmol/kg dose) to 12.2 ml/min per kg (0.25 mmol/kg), and the renal CL (CLR) was 3.74 ± 1.00 (0.03-mmol/kg) to 3.88 ± 0.71 ml/min per kg (0.25 mmol/kg). Vmax was 2.40 ± 0.98 μmol/min per kg at the 0.25 mmol/kg dose. After 7 days, the urinary excretion was 27.1 ± 2.08 (0.03 mmol/kg) to 40.9 ± 2.35%ID (0.25 mmol/kg). The % ID fecal excretion was 70.1 ± 3.25 to 57.0 ± 2.48 for the low dose and high doses, respectively.
Benness et al. (24, 25) studied the hepatic kinetics and MRI (1.5 T) of Gd-EOB-DTPA in dogs. After bolus injection, there was a rapid increase and exponential decline of plasma Gd-EOB-DTPA concentration. Rapid accumulation of Gd-EOB-DTPA in the liver was demonstrated by very early positive enhancement. The study showed that a hepatic transport maximum of 0.09−0.15 μmol/min per kg was achieved with bolus doses (12.5−200 μmol/kg) followed by infusion (0.4−6.4 μmol/kg). Maximum t1 signal enhancement was achieved with blood concentration of 0.02−0.03 μmol/ml and a liver concentration of 1−2 μmol/ml.
Non-Human Primates
[PubMed]
Schuhmann-Glampieri et al. (1) studied the elimination and biodistribution of Gd-EOB-DTPA (0.25-mmol/kg) in two female cynomolgus monkeys. Seven days after administration, the percent injected dose values in the major organs were 0.28−0.52 (liver), 0.03−0.14 (kidneys), 0.04−0.12 (spleen), and 0.16−0.61 (GI tract). Approximately 47.8−63.2% ID was excreted in the urine, and 32.2-34.0% ID was excreted in the feces. In another study, Shuhmann-Giampieri et al. (10, 21) reported a CL of 2.93 ± 1.06 ml/min per kg and a CLR of 1.01 ± 0.26 ml/min per kg after a single i.v. dose of 0.25 mmol/kg in 5 female cynomolgus monkeys. Vmax was 0.81 ± 0.66 μmol/min.kg for the 0.25-mmol/kg dose.. After 7 days, the renal, fecal, and total body recovery values were 44.0 ± 14.1, 32.1 ± 6.41, and 76.0 ± 11.6% ID, respectively. Plasma binding was 17.5 ± 1.0%.
Human Studies
[PubMed]
Schuhmann-Giampieri et al. (26) studied the pharmacokinetics of Gd-EOB-DTPA in 23 healthy young male volunteers. Single doses of 0.2, 0.35, and 0.5 mmol/kg (in 0.25 mol/liter) were administered as a 10-min infusion into each volunteer. Serum concentrations declined rapidly and then the decline slowed and appeared to be log-linear. The major pharmacokinetic parameters (ranges for 0.2 mmol/kg to 0.5 mmol/kg) were calculated to be 1.86 ± 0.20 to 3.12 ± 0.78 h (serum t½), 2.01 ± 0.18 to 2.21 ± 0.31 h (urine t½), 0.55 ± 0.03 to 0.38 ± 0.05 liter/kg (Vdss), 2.72 ± 0.18 to 2.13 ± 0.16 ml/min per kg (total serum CL), and 1.18 ± 0.23 to 1.25 ± 0.11 ml/min per kg (CLR). The 6-day cumulative renal excretion was 43.6 ± 8.6 to 59.1 ± 5.6% ID. The 6-day cumulative extrarenal excretion in the feces was 36.8 ± 8.5 to 27.1 ± 8.1% ID. The urinary excretion was rapid and independent of the dose, CLR was ~100 ml/min which indicated that glomerular filtration was the main pathway of renal elimination. Gd-EOB-DTPA was generally well tolerated with no serious adverse events.
In a phase I clinical evaluation of Gd-EOB-DTPA as a hepatobiliary MRI agent, Hamm et al. (27) studied 60 healthy male volunteers. The doses ranged from 10 to 100 μmol/kg. In the tolerance and safety studies of 44 volunteers, Gd-EOB-DTPA was generally well tolerated. The biexponential decay of serum Gd concentrations could be described with a two-compartment model. Practically independent of dose, the compound was completely eliminated in urine and feces in nearly equal amounts. Reverse-phase HPLC analysis of urine samples 2 hours after injection showed no conversion of Gd-EOB-DTPA to a new compound. MRI imaging (1.5 T) of 16 volunteers showed homogeneous enhancement of liver parenchyma immediately after injection. Peak liver signal intensity was observed at 20 min after injection. This was followed by plateau-like enhancement over 2 h. Bollow et al. (28) reported that the common bile duct showed intense signal enhancement that began 5-16 min after injection and persisted for 120−360 min. Gallbladder contrasting was achieved in all 16 volunteers. The dosage for hyperintense visualization of intrahepatic duct was 10 μmol/kg.
Reimer et al. (29) reported the results of a phase II clinical evaluation of Gd-EOB-DTPA. A randomized double-blind trial was performed in 33 patients with focal solid liver lesions. Three different doses (12.5, 25, and 50 μmol/kg) were studied with MRI (1.0 T). All doses increased liver signal intensity and lesion-liver C/N ratios ([mean signal intensity of lesion –mean signal intensity of liver]/standard deviation of background noise). The lowest dose (12.5 μmol/kg) was sufficient to enhance the detection of focal liver lesions. Depending on the imaging techniques, the lesion-liver C/N ratios (n = 10) for liver metastases ranged from 6.4 ± 3.9 to 16.0 ± 9.2 (eight techniques) at 20 min after injection. At 45 min, the C/N ratios were 10.7 ± 4.0 to 14.9 ± 9.2 (four techniques). No significant changes in vital signs, clinical laboratory test results, or urinalysis were observed. In the multicenter phase III efficacy and safety clinical trial, Bluemke, et al. (30) studied 172 patients with liver lesions from 12 medical centers. All patients received 25 μmol/kg of Gd-EOB-DTPA as an i.v. bolus injection (2 ml/sec). MRI was performed by 1.5-T systems to obtain both t1-weighted and t2-weighted images. For the total number of lesions that were correctly detected and classified as benign or malignant by three blinded readers, the ranges of sensitivity for precontrast MRI (t1-weighted and t2-weighted, t1-weighted), postcontrast MRI (t1-weighted and t2-weighted, t1-weighted), combined pre- and postcontrast MRI, and helical CT were 49.1−63.8, 59.0−72.8, 65.9−70.0, and 60.0−68.4%, respectively. Overall, there were 28 adverse events in 17 (10.0%) of 169 patients. Only one event was classified as definitely related to the contrast agent. All events were mild or moderate in intensity.
References
- 1.
- Schuhmann-Giampieri G. , Schmitt-Willich H. , Press W.R. , Negishi C. , Weinmann H.J. , Speck U. Preclinical evaluation of Gd-EOB-DTPA as a contrast agent in MR imaging of the hepatobiliary system. Radiology. 1992; 183 (1):59–64. [PubMed: 1549695]
- 2.
- Schmitt-Willich H. , Brehm M. , Ewers C.L. , Michl G. , Muller-Fahrnow A. , Petrov O. , Platzek J. , Raduchel B. , Sulzle D. Synthesis and Physicochemical Characterization of a New Gadolinium Chelate: The Liver-Specific Magnetic Resonance Imaging Contrast Agent Gd-EOB-DTPA. Inorg Chem. 1999; 38 (6):1134–1144. [PubMed: 11670895]
- 3.
- Gadoxate disodium: gadolinium EOB DTPA, gadoxetic acid, Gd-EOB-DTPA. Drugs R D. 2004; 5 (4):227–30. [PubMed: 15230630]
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Gadobenate.[Molecular Imaging and Contrast...]Review Gadobenate.Cheng KT. Molecular Imaging and Contrast Agent Database (MICAD). 2004
- Review Gadobutrol.[Molecular Imaging and Contrast...]Review Gadobutrol.Cheng KT. Molecular Imaging and Contrast Agent Database (MICAD). 2004
- Review Gadoversetamide: Gd-DTPA-BMEA.[Molecular Imaging and Contrast...]Review Gadoversetamide: Gd-DTPA-BMEA.Cheng KT. Molecular Imaging and Contrast Agent Database (MICAD). 2004
- Review Gadoteridol : Gd-HP-DO3A.[Molecular Imaging and Contrast...]Review Gadoteridol : Gd-HP-DO3A.Cheng KT. Molecular Imaging and Contrast Agent Database (MICAD). 2004
- Gadolinium Magnetic Resonance Imaging.[StatPearls. 2024]Gadolinium Magnetic Resonance Imaging.Ibrahim MA, Hazhirkarzar B, Dublin AB. StatPearls. 2024 Jan
- Gadoxetate - Molecular Imaging and Contrast Agent Database (MICAD)Gadoxetate - Molecular Imaging and Contrast Agent Database (MICAD)
Your browsing activity is empty.
Activity recording is turned off.
See more...

 In vitro
In vitro