Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
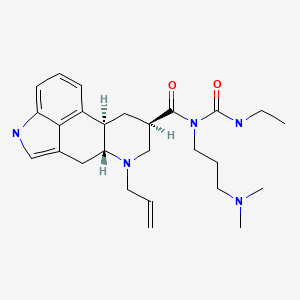
CASRN: 81409-90-7
Drug Levels and Effects
Summary of Use during Lactation
Cabergoline is usually not used during breastfeeding because it suppresses lactation. The U.S. Food and Drug Administration considers cabergoline to be not indicated to suppress lactation because the similar drug bromocriptine has caused hypertension, stroke, seizures and psychosis when used for this purpose. However, two systematic reviews found that cabergoline was generally well tolerated for use in suppressing lactation, but dizziness, headache, nausea and vomiting occur occasionally.[1-3] A retrospective study of 225 women who received cabergoline postpartum had a maximum decrease in systolic blood pressure of 10.88 mm Hg at 20 to 24 hours after the dose.[4] Serious reactions are uncommon, but include thromboembolic and neurologic events. Psychiatric symptoms have occurred rarely. Some experts recommend cabergoline as a safer alternative to bromocriptine for lactation suppression, but others do not.[5-9] The disadvantage of cabergoline is that it has a half-life of about 68 hours, which means that any adverse effects might persist for a prolonged period of time. Women treated with cabergoline for pituitary adenomas who become pregnant can breastfed their infants with no apparent risk of recurrence. A treatment scheme has been reported for mothers with hypergalactia that uses low doses of cabergoline to decrease milk supply.[10] Decreased milk synthesis may occur by 2 days after drug administration.[11]
Drug Levels
Maternal Levels. Relevant published information was not found as of the revision date.
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
A woman with acromegaly was treated with lanreotide Autogel 120 mg monthly, cabergoline 2 mg weekly and pegvisomant 80 mg weekly. She breastfed (extent not stated) her infant and they were followed for 12 years. Her child had normal growth and development.[12]
Effects on Lactation and Breastmilk
Seventeen women who did not wish to breastfeed received a placebo or a single oral dose of cabergoline 400 mcg or 600 mcg on day 2 or 3 postpartum. Use of other lactation suppressing measures (e.g., breast binding, lack of nipple stimulation) was not mentioned. Blood samples were taken periodically over the next 96 hours. In the 7 women who received 400 mcg, plasma prolactin levels were decreased at 24 and 48 hours, but 4 developed breast engorgement. In the 5 women who received 600 mcg, plasma prolactin levels were decreased by 12 hours and persisted up to 96 hours and none developed breast engorgement. Some women had minor decreases in blood pressure, but no other adverse effects were reported.[13]
Thirty-two women who did not wish to breastfeed were given placebo or cabergoline 400, 600 or 800 mcg within 24 hours after delivery in a double-blind trial. Use of other lactation suppressing measures (e.g., breast binding, lack of nipple stimulation) was not mentioned. Lactation was prevented in 4 of 8 women who received the 400 mcg dose and all women who received the 600 or 800 mcg dose. Only 1 of 8 women receiving placebo had cessation of lactation by day 14 postpartum. Serum prolactin levels collected on days 2, 3 and 4 of treatment were decreased significantly in all women who received cabergoline, but the decreases were not statistically different among the various doses.[14]
A prospective, randomized, double-blinded study compared the effects of a single dose of cabergoline 0.5, 0.75 or 1 mg in 40 women each and to 20 women who received a placebo. The drug was given in the first 24 hours postpartum and use of other lactation suppressing measures (e.g., breast binding, lack of nipple stimulation) was not mentioned. The adequacy of lactation suppression on day 14 postpartum was dose-related, with excellent results in 18 patients who receive 0.5 mg, 28 who received 0.75 mg and 36 who received 1 mg. Serum prolactin levels collected during 13 days of treatment were decreased significantly in all women who received cabergoline, but the decreases were not statistically different among the various doses. Adverse effects included occasional dizziness and headache between days 1 and 3 after the dose.[15]
In a single-blind trial, 36 women were given either a single oral dose of cabergoline 1 mg or oral bromocriptine 2.5 mg twice daily for 14 days, starting about 50 hours after cesarean section. Use of other lactation suppressing measures (e.g., breast binding, lack of nipple stimulation) was not mentioned. Another 13 women who were breastfeeding after cesarean section served as controls. Both cabergoline and bromocriptine suppressed baseline serum prolactin by about 90% compared to baseline and control women within 3 days; this persisted at least through day 7, but somewhat rebounded by day 14. Suppression of lactation as measured by milk secretion, tenderness, and engorgement was equal between the 2 treatment groups. Lactation suppression was complete in 17 of 18 women who received cabergoline and 16 of 18 women who received bromocriptine, although the response was more rapid with cabergoline. Adverse events from cabergoline were fewer in number than with bromocriptine and consisted of occasional headache lasting 2 days, dizziness, and vomiting.[16]
A well-designed and evaluated double-blind study compared oral cabergoline 1 mg in a single dose (n = 136) to oral bromocriptine 2.5 mg twice daily for 14 days (n = 136) in women within 27 hours postpartum. Some women in each group (cabergoline n = 18; bromocriptine n = 16) received an ergot alkaloid or oral contraceptive postpartum. Symptoms of milk production and engorgement were recorded by the women and serum prolactin levels were measured on 3 occasions during the first 2 to 3 weeks postpartum. Cabergoline was at least as effective as bromocriptine, with complete success in 78% of cabergoline patients and 69% of bromocriptine patients. The rate of rebound lactation was much higher in bromocriptine patients (24%) than in cabergoline patients (5%). Serum prolactin was suppressed in both groups, but rebound was more common with bromocriptine on days 15 and 21. Adverse effects were numerically, but not statistically less frequent in cabergoline patients, with the most frequent being dizziness, headache, nausea and epigastric pain.[17]
Cabergoline was evaluated for lactation suppression in a prospective, but nonrandomized, unblinded trial. Women who were within 24 hours postpartum were given a single 1 mg dose (n = 54); those who were beyond 24 hours were given 0.25 mg twice daily for 2 days (n = 46). Only composite results were given for the entire group of 100 women. Mean serum prolactin dropped from 181.4 mcg/L (range 153 to 213 mcg/L) on the first day to 12.5 mcg/L (range 0.9 to 37 mcg/L) on day 4, and 18.2 mcg/L (range 2 to 36.2 mcg/L) on day 14 after the dose. Lactation was completely inhibited in 92% of women; 8 women required a second doses of 1 mg to inhibit lactation. Twenty-six percent of women had side effects such as dizziness, headache, nausea and abdominal pain. In 4% of women, side effects were severe enough to require symptomatic treatment.[13,18]
In a prospective, nonrandomized, unblinded trial, 43 women who underwent a second trimester abortion were given cabergoline 1 mg orally to suppress lactation. A single dose was effective in 88% of women.[19]
A randomized, nonblinded trial compared cabergoline 0.5 mg (n = 80) and 1 mg (n = 80) orally in a single dose given at an unstated time in the early postpartum period. The 1 mg dose was more effective in suppressing lactation than the 0.5 mg dose. Headache and nausea were the most common adverse effects.[20]
A follow-up survey was conducted on 91 women who became pregnant after treatment with cabergoline for hyperprolactinemia from pituitary adenomas. Eighty-eight patients breastfed their infants, 35 for less than 2 months and 56 for 2 to 6 months. No patients were restarted on cabergoline after pregnancy. At 3 and 12 months after pregnancy, serum prolactin was slightly higher than prepregnancy levels, but by 60 months postpartum, prolactin levels were lower than prepregnancy levels. Mothers who nursed for more than 2 months had lower serum prolactin at 60 months after cessation of breastfeeding than those who breastfed for less than 2 months. The authors concluded that breastfeeding does not increase the risk of recurrence of hyperprolactinemia.[21]
A woman with severe breast engorgement with nipple cracking and bleeding was started on ibuprofen and cabergoline 0.125 mg daily for 2 days in addition to cold dressing applications. By day 6 postpartum, her breasts softened, the nipple crack receded and the pain decreased. She was able to begin breastfeeding her infant on day 6 and was mostly breastfeeding her infant by day 13 postpartum.[22]
Sixty-seven women with HIV infections were given a single dose of 1 mg of cabergoline within 48 hours postpartum to prevent lactation. Complete or partial suppression of lactation occurred in 98% of women on day 14 and 67% had serum prolactin levels below 25 mcg/L, which is the threshold necessary for galactopoiesis. Ninety-six percent of women were satisfied with cabergoline’s effect on lactation.[23]
A pregnant woman was found to have a nonfunctioning pituitary adenoma. She had a somewhat elevated serum prolactin of 467 mcg/L. Cabergoline 0.25 mg twice weekly was started in the second trimester of pregnancy and continued for 2 weeks postpartum. At 3.5 weeks postpartum her serum prolactin was 16 mcg/L and she produced only drops of milk for the first 8 weeks postpartum. Using an electric breast pump, her milk supply increased to over 800 mL daily by 21 weeks postpartum. At 30.5 weeks postpartum, her serum prolactin was 27 mcg/L.[24]
A woman nursing a 3-month-old infant was diagnosed with ductal carcinoma of the left breast. She was given cabergoline (presumably 1 mg) to stop lactation prior to an 18F-FDG PET/CT scan to delineate the extent of the lesion. The scan performed 2 days after the dose of cabergoline showed no lactation-related radionuclide uptake.[11]
A double-blind, randomized, placebo-controlled study of a single dose of cabergoline 1 mg orally was conducted in women who underwent uterine evacuation for a second-trimester abortion or fetal death. The dose was given within 4 hours of the procedure or fetal expulsion. On post-procedure days 1 to 14, breast symptoms (engorgement, breast tenderness, leaking milk and requiring pharmacologic pain relief) were less in those who received cabergoline than those who received placebo. In a subset of participants, serum prolactin level on day 4 was 6.5 ng/mL for those who received cabergoline compared with 18 ng/ mL receiving placebo; the difference was statistically significant. Hot flushes were significantly less frequent in the cabergoline group on day 4.[3]
A randomized, prospective, but nonmasked study compared cabergoline 1 mg (in one dose or 0.25 mg twice daily for 2 days; n = 45) to pyridoxine 200 mg 3 times daily for 7 days (n = 43) in suppressing lactation in postpartum women who did not wish to breastfeed. Treatment was initiated approximately 24 hours after delivery. Based on patient self-assessment, cabergoline was more effective than pyridoxine for suppressing lactation (78% vs 35%) and in reducing engorgement and pain (89% vs 67%) at day 7. The frequency of milk leakage was lower with cabergoline group after 7 and 14 days compared to pyridoxine (9% vs 42% and 11% vs 31%, , respectively). Headache and constipation were the most commonly reported adverse effects, occurring more frequently in cabergoline patients (15% vs 2%).[25]
In a small preliminary study, women wishing to stop lactation at 1 month postpartum were given cabergoline 500 mg daily for 7 days. The degree of mammary duct dilation was compared before and after treatment in these women and in women who slowly decreased breastfeeding to stop lactation. More mothers who received cabergoline had a reduction in mammary duct dilation on ultrasound than women who did not.[26]
Alternate Drugs to Consider
(Hyperprolactinemia) Bromocriptine
References
- 1.
- Harris K, Murphy KE, Horn D, et al. Safety of cabergoline for postpartum lactation inhibition or suppression: A systematic review. J Obstet Gynaecol Can 2020;42:308-315.e20. [PubMed: 31285168]
- 2.
- Yang Y, Boucoiran I, Tulloch KJ, Poliquin V. Is cabergoline safe and effective for postpartum lactation inhibition? A systematic review. Int J Womens Health 2020;12:159-70. [PMC free article: PMC7069562] [PubMed: 32210637]
- 3.
- Henkel A, Johnson SA, Reeves MF, et al. Cabergoline for lactation inhibition after second-trimester abortion or pregnancy loss: A randomized controlled trial. Obstet Gynecol 2023;141:1115-23. [PubMed: 37486652]
- 4.
- Humphrey S, Baechler M, Schiff M, Hitti J. Cabergoline for postpartum lactation suppression: Effect on blood pressure and pulse. Int J Gynaecol Obstet 2022;159:776-82. [PubMed: 35304744]
- 5.
- Anon. Inhibiting the onset of lactation: Is cabergoline an alternative to bromocriptine? Prescrire Int 2015;24:276-7. [PubMed: 26688910]
- 6.
- Marcellin L, Chantry AA. [Breast-feeding (part II): Lactation inhibition--Guidelines for clinical practice]. J Gynecol Obstet Biol Reprod (Paris) 2015;44:1080-3. [PubMed: 26527027]
- 7.
- Snellen M, Power J, Blankley G, Galbally M. Pharmacological lactation suppression with D2 receptor agonists and risk of postpartum psychosis: A systematic review. Aust N Z J Obstet Gynaecol 2016;56:336-40. [PubMed: 27297803]
- 8.
- Tulloch KJ, Dodin P, Tremblay-Racine F, et al. Cabergoline: A review of its use in the inhibition of lactation for women living with HIV. J Int AIDS Soc 2019;22:e25322. [PMC free article: PMC6558502] [PubMed: 31183987]
- 9.
- Fachi MM, de Deus Bueno L, de Oliveira DC, et al. Efficacy and safety in the treatment of hyperprolactinemia: A systematic review and network meta-analysis. J Clin Pharm Ther 2021;46:1549-56. [PubMed: 34137053]
- 10.
- Johnson HM, Eglash A, Mitchell KB, et al. ABM Clinical Protocol #32: Management of hyperlactation. Breastfeed Med 2020;15:129-34. [PubMed: 32031417]
- 11.
- Kuroda H, Yoshizako T, Yamamoto N, et al. A case of breast cancer: Suppression of lactation-related FDG uptake 2 days after cabergoline administration. Acta Radiol Open 2023;12:20584601231174611. [PMC free article: PMC10164254] [PubMed: 37163201]
- 12.
- Popescu AD, Carsote M, Valea A, et al. Approach of acromegaly during pregnancy. Diagnostics (Basel) 2022;12:2669. [PMC free article: PMC9689290] [PubMed: 36359512]
- 13.
- Melis GB, Gambacciani M, Paoletti AM, et al. Dose-related prolactin inhibitory effect of the new long-acting dopamine receptor agonist cabergoline in normal cycling, puerperal, and hyperprolactinemic women. J Clin Endocrinol Metab 1987;65:541-5. [PubMed: 3624413]
- 14.
- Melis GB, Mais V, Paoletti AM, et al. Prevention of puerperal lactation by a single oral administration of the new prolactin-inhibiting drug, cabergoline. Obstet Gynecol 1988;71:311-4. [PubMed: 3279351]
- 15.
- Caballero-Gordo A, López-Nazareno N, Calderay M, et al. Oral cabergoline. Single-dose inhibition of puerperal lactation. J Reprod Med 1991;36:717-21. [PubMed: 1683403]
- 16.
- Giorda G, de Vincentiis S, Motta T, et al. Cabergoline versus bromocriptine in suppression of lactation after cesarean delivery. Gynecol Obstet Invest 1991;31:93-6. [PubMed: 2037265]
- 17.
- European Multicentre Study Group for Cabergoline in Lactation Inhibition. Single dose cabergoline versus bromocriptine in inhibition of puerperal lactation: Randomised, double blind, multicentre study. BMJ 1991;302:1367-71. [PMC free article: PMC1670075] [PubMed: 1676318]
- 18.
- Bracco PL, Armentano G, Pellegrini A, et al. [Cabergoline in the inhibition of lactogenesis and suppression of lactopoiesis]. Minerva Ginecol 1997;49:469-73. [PubMed: 9463181]
- 19.
- Pavlista D, Calda P, Zivny J. [Arrest of lactation after 2nd trimester abortion with a single dose of cabergoline in comparison with 10-day administration of teguride]. Ceska Gynekol 2003;68:46-50. [PubMed: 12708116]
- 20.
- Bravo-Topete EG, Mendoza-Hernandez F, Cejudo-Alvarez J, Briones-Garduno C. [Cabergoline for inhibition of lactation]. Cir Cir 2004;72:5-9. [PubMed: 15087045]
- 21.
- Auriemma RS, Perone Y, Di Sarno A, et al. Results of a single-center observational 10-year survey study on recurrence of hyperprolactinemia after pregnancy and lactation. J Clin Endocrinol Metab 2013;98:372-9. [PubMed: 23162092]
- 22.
- Coban A, Bayraktar S, Yıldız N, et al. A case study of early postpartum excessive breast engorgement: Is it related to feedback inhibition of lactation? J Hum Lact 2021;37:414-8. [PubMed: 33030995]
- 23.
- Boucoiran I, Roy M, Poliquin V, et al. Evaluation of cabergoline for lactation inhibition in women living with HIV. Int J STD AIDS 2021;32:654-61. [PubMed: 33612017]
- 24.
- Bartell GS. Lactogenesis II onset following prolonged delay in a mother with a nonfunctioning macroadenoma treated with cabergoline: A case study in persistence. Clin Lact (Amarillo) 2021;12:22-9. doi:10.1891/clinlact-d-20-00014 [CrossRef]
- 25.
- Dayan-Schwartz A, Yefet E, Manal Massalha, et al. The efficiency of cabergoline versus pyridoxine for lactation inhibition - a randomized controlled trial. Am J Obstet Gynecol 2023. [PubMed: 37827268]
- 26.
Substance Identification
Substance Name
Cabergoline
CAS Registry Number
81409-90-7
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Cabergoline. A review of its pharmacological properties and therapeutic potential in the treatment of hyperprolactinaemia and inhibition of lactation.[Drugs. 1995]Review Cabergoline. A review of its pharmacological properties and therapeutic potential in the treatment of hyperprolactinaemia and inhibition of lactation.Rains CP, Bryson HM, Fitton A. Drugs. 1995 Feb; 49(2):255-79.
- Review Methylergonovine.[Drugs and Lactation Database (...]Review Methylergonovine.. Drugs and Lactation Database (LactMed®). 2006
- Review Is Cabergoline Safe and Effective for Postpartum Lactation Inhibition? A Systematic Review.[Int J Womens Health. 2020]Review Is Cabergoline Safe and Effective for Postpartum Lactation Inhibition? A Systematic Review.Yang Y, Boucoiran I, Tulloch KJ, Poliquin V. Int J Womens Health. 2020; 12:159-170. Epub 2020 Mar 9.
- Review Safety of Cabergoline for Postpartum Lactation Inhibition or Suppression: A Systematic Review.[J Obstet Gynaecol Can. 2020]Review Safety of Cabergoline for Postpartum Lactation Inhibition or Suppression: A Systematic Review.Harris K, Murphy KE, Horn D, MacGilivray J, Yudin MH. J Obstet Gynaecol Can. 2020 Mar; 42(3):308-315.e20. Epub 2019 Jul 6.
- Inhibitory effect of cabergoline on the development of estrogen-induced prolactin-secreting adenomas of the pituitary.[Eur J Pharmacol. 1988]Inhibitory effect of cabergoline on the development of estrogen-induced prolactin-secreting adenomas of the pituitary.Dall'Ara A, Lima L, Cocchi D, Di Salle E, Cancio E, Devesa J, Müller EE. Eur J Pharmacol. 1988 Jun 22; 151(1):97-102.
- Cabergoline - Drugs and Lactation Database (LactMed®)Cabergoline - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
