NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Wilt TJ, Carlson KF, Goldish GD, et al. Carbohydrate and Lipid Disorders and Relevant Considerations in Persons with Spinal Cord Injury. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Jan. (Evidence Reports/Technology Assessments, No. 163.)
This publication is provided for historical reference only and the information may be out of date.
Cardiovascular diseases1 (CVD). Pathological conditions involving the cardiovascular system including the heart; the blood vessels; or the pericardium.
Operational definition: Prevalence of CVD and diabetes and incidence rate of CVD events. Definitions of CVD events are presented below.
| Variable | Definition |
|---|---|
| Arrhythmia | Any variation from the normal rhythm or rate of the heartbeat |
| Arrhythmia, sinus | Irregularity of the heart rate related to functioning of the sinoatrial node |
| Atrial fibrillation | Disorder of cardiac rhythm characterized by rapid, irregular atrial impulses and ineffective atrial contractions |
| Atrial flutter | Rapid, irregular atrial contractions due to an abnormality of atrial excitation |
| Bradycardia | Excessive slowness in the action of the heart, usually with a heart rate below 60 beats per minute |
| Cardiac complexes, premature | A premature contraction of the heart that is initiated somewhere other than the sinoatrial node |
| Atrial premature complexes | Premature contractions of the heart arising from an ectopic atrial focus |
| Ventricular premature complexes | Premature contractions of the ventricle, the most common of all arrhythmias |
| Heart block | Impairment of conduction in heart excitation. It is often applied specifically to atrioventricular heart block |
| Long QT syndrome | A syndrome characterized by history of syncopal episodes and a long QT interval, sometimes leading to sudden death due to paroxysmal ventricular arrhythmia |
| Sick sinus syndrome | Dysfunction of the sinoatrial node manifested by persistent sinus bradycardia, sinus arrest, sinoatrial exit block, chronic atrial fibrillation and inability of the heart to resume sinus rhythm following cardioversion for atrial fibrillation |
| Tachycardia | Excessive rapidity in the action of the heart, usually with a heart rate above 100 beats per minute |
| Ventricular fibrillation | Turbulent, disorganized electrical activity of the heart in such a way that the recorded electrocardiographic deflections continuously change in shape, magnitude, and direction |
| Heart arrest | Abrupt cessation of cardiac pump function which may be reversible by a prompt intervention but will lead to death in its absence |
| Cardiovascular collapse | A sudden loss of effective blood flow due to cardiac and/or peripheral vascular factors which may reverse spontaneously (e.g., neurocardiogenic syncope; vasovagal syncope) or only with interventions (e.g., cardiac arrest) |
| Congestive heart failure | Defective cardiac filling and/or impaired contraction and emptying, resulting in the heart's inability to pump a sufficient amount of blood to meet the needs of the body tissues or to be able to do so only with an elevated filling pressure |
| Coronary disease | An imbalance between myocardial functional requirements and the capacity of the coronary vessels to supply sufficient blood flow Coronary artery abnormalities
|
| Myocardial infarction | Gross necrosis of the myocardium, as a result of interruption of the blood supply to the area
|
| Pericarditis | Inflammation of the pericardium |
| Stroke | Sudden, nonconvulsive loss of neurological function due to an ischemic or hemorrhagic intracranial vascular event. In general, cerebrovascular accidents are classified by anatomic location in the brain, vascular distribution, etiology, age of the affected individual, and hemorrhagic vs. nonhemorrhagic nature. |
| Hypertension | Persistently high systemic arterial blood pressure. Based on multiple readings, hypertension is currently defined as when systolic blood pressure is consistently greater than 140 mm Hg or when diastolic pressure is consistently 90 mm Hg or more. |
| Death | Irreversible cessation of all biologic functions |
| Cardiovascular mortality | Death from cardiovascular diseases (considered as immediate and underlying cause of death) |
International Classification of Diseases Codes to Identify Outcomes2
| 404 | Hypertensive heart and kidney disease |
| Includes: disease: cardiorenal; cardiovascular renal; any condition classifiable to 402 with any condition classifiable to 403 | |
| Additional code to specify type of heart failure (428.0–428.43), if known | |
| Additional code to identify the stage of chronic kidney disease (585.1–585.6), if known | |
| The following fifth-digit sub-classification is for use with category 404: | |
| 0 without heart failure or chronic kidney disease | |
| 1 with heart failure | |
| 2 with chronic kidney disease | |
| 3 with heart failure and chronic kidney disease | |
| 402 | Hypertensive heart disease |
| Includes: hypertensive: cardiomegaly; cardiopathy; cardiovascular disease; heart (disease) (failure), any condition classifiable to 429.0–429.3, 429.8, 429.9 due to hypertension | |
| Use additional code to specify type of heart failure (428.0–428.43), if known | |
| 427 | Cardiac dysrhythmias |
| 427.0 | Paroxysmal supraventricular tachycardia |
| Paroxysmal tachycardia: atrial [PAT]; atrioventricular [AV]; junctional nodal | |
| 427.1 | Paroxysmal ventricular tachycardia |
| Ventricular tachycardia (paroxysmal) | |
| 427.2 | Paroxysmal tachycardia, unspecified |
| Bouveret-Hoffmann syndrome | |
| Paroxysmal tachycardia | |
| 427.3 | Atrial fibrillation and flutter |
| 427.31 | Atrial fibrillation |
| 427.32 | Atrial flutter |
| 427.5 | Cardiac arrest |
| Cardiorespiratory arrest | |
| 427.6 | Premature beats |
| 427.60 | Premature beats, unspecified |
| Ectopic beats | |
| Extrasystoles | |
| Extrasystolic arrhythmia | |
| Premature contractions or systoles NOS | |
| 427.8 | Other specified cardiac dysrhythmias |
| 427.81 | Sinoatrial node dysfunction |
| Sinus bradycardia: persistent severe | |
| Syndrome: sick sinus; tachycardia-bradycardia | |
| 427.9 | Cardiac dysrhythmia, unspecified |
| Arrhythmia (cardiac) NOS | |
| 428.0 | Congestive heart failure, unspecified |
| Congestive heart disease | |
| Right heart failure (secondary to left heart failure) | |
| 428.1 | Left heart failure |
| Acute edema of lung with heart disease NOS or heart failure | |
| Acute pulmonary edema with heart disease NOS or heart failure | |
| Cardiac asthma | |
| Left ventricular failure | |
| 428.9 | Heart failure, unspecified |
| Cardiac failure NOS | |
| Heart failure NOS | |
| Myocardial failure NOS | |
| Weak heart | |
| 428 | Heart failure |
| Code, if applicable, heart failure due to hypertension first (402.0–402.9, with fifth-digit 1 or 404.0–404.9 with fifth-digit 1 or 3) | |
| 429.2 | Cardiovascular disease, unspecified |
| Arteriosclerotic cardiovascular disease [ASCVD] | |
| Cardiovascular arteriosclerosis | |
| Cardiovascular: degeneration (with mention of arteriosclerosis) disease (with mention of arteriosclerosis) | |
| Sclerosis (with mention of arteriosclerosis) | |
| Additional code to identify presence of arteriosclerosis | |
| 794 | Nonspecific abnormal results of function studies |
| 250 | Diabetes mellitus |
| 250.0 | Diabetes mellitus without mention of complication |
| Diabetes mellitus without mention of complication or manifestation classifiable to 250.1–250.9 | |
| Diabetes (mellitus) NOS | |
| 250.6 | Diabetes with neurological manifestations |
| Additional code to identify manifestation, as: | |
| diabetic: | |
| amyotrophy (358.1) | |
| gastroparalysis (536.3) | |
| gastroparesis (536.3) | |
| mononeuropathy (354.0–355.9) | |
| neurogenic arthropathy (713.5) | |
| peripheral autonomic neuropathy (337.1) | |
| polyneuropathy (357.2) | |
| 250.7 | Diabetes with peripheral circulatory disorders |
| Use additional code to identify manifestation, as: | |
| diabetic: | |
| gangrene (785.4) | |
| peripheral angiopathy (443.81) | |
| 250.8 | Diabetes with other specified manifestations |
| Diabetic hypoglycemia | |
| Hypoglycemic shock | |
| Use additional code to identify manifestation, as: | |
| any associated ulceration (707.10–707.9) | |
| diabetic bone changes (731.8) |
International Classification of Diseases Codes to Identify Outcomes in Individual Studies:
Groah, 2001:3 Cardiovascular disease outcomes defined by ICD/9 codes 390–448 and 745–747:
DISEASES OF THE CIRCULATORY SYSTEM (390–459)
ACUTE RHEUMATIC FEVER (390–392)
CHRONIC RHEUMATIC HEART DISEASE (393–398)
HYPERTENSIVE DISEASE (401–405)
ISCHEMIC HEART DISEASE (410–414)
Includes: that with mention of hypertension
Additional code to identify presence of hypertension (401.0–405.9)
DISEASES OF PULMONARY CIRCULATION (415–417)
OTHER FORMS OF HEART DISEASE (420–429)
CEREBROVASCULAR DISEASE (430–438)
Includes: with mention of hypertension (conditions classifiable to 401–405)
DISEASES OF ARTERIES, ARTERIOLES, AND CAPILLARIES (440–448)
745 Bulbus cordis anomalies and anomalies of cardiac septal closure
746 Other congenital anomalies of heart
747 Other congenital anomalies of circulatory system
McGlinchey-Berroth, 19954 Hospitalization due to myocardial infarction (ICD-9-CM 410.9), diabetes (ICD 250.00 to 250.9), and hypertension (ICD 401.0 to 401.9).
410 Acute myocardial infarction
Includes: cardiac infarction; coronary (artery):embolism; occlusion; rupture; thrombosis; infarction of heart, myocardium, or ventricle; rupture of heart, myocardium, or ventricle;
ST elevation (STEMI) and non-ST elevation (NSTEMI) myocardial infarction; any condition classifiable to 414.1–414.9 specified as acute or with a stated duration of 8 weeks or less
The following fifth-digit subclassification is for use with category 410:
0 episode of care unspecified
1 initial episode of care
The fifth-digit 1 to designate the first episode of care (regardless of facility site) for a newly diagnosed myocardial infarction. The fifth-digit 1 is assigned regardless of the number of times a patient may be transferred during the initial episode of care.
2 subsequent episode of care
The fifth-digit 2 to designate an episode of care following the initial episode when the patient is admitted for further observation, evaluation or treatment for a myocardial infarction that has received initial treatment, but is still less than 8 weeks old.
410. 0 Of anterolateral wall
ST elevation myocardial infarction (STEMI) of anterolateral wall
410. 1 Of other anterior wall
Infarction:
anterior (wall) NOS (with contiguous portion of intraventricular septum)
anteroapical (with contiguous portion of intraventricular septum)
anteroseptal (with contiguous portion of intraventricular septum)
ST elevation myocardial infarction (STEMI) of other anterior wall
410.2 Of inferolateral wall
ST elevation myocardial infarction (STEMI) of inferolateral wall
410.3 Of inferoposterior wall
ST elevation myocardial infarction (STEMI) of inferoposterior wall
410.4 Of other inferior wall
Infarction: diaphragmatic wall NOS (with contiguous portion of intraventricular septum)
inferior (wall) NOS (with contiguous portion of intraventricular septum)
ST elevation myocardial infarction (STEMI) of other inferior wall
410.5 Of other lateral wall
Infarction: apical-lateral; basal-lateral; high lateral; posterolateral
ST elevation myocardial infarction (STEMI) of other lateral wall
410.6 True posterior wall infarction
Infarction: posterobasal; strictly posterior
ST elevation myocardial infarction (STEMI) of true posterior wall
410.7 Subendocardial infarction
Non-ST elevation myocardial infarction (NSTEMI)
Nontransmural infarction
410.8 Of other specified sites
Infarction of: atrium; papillary muscle; septum alone
ST elevation myocardial infarction (STEMI) of other specified sites
410.9 Unspecified site
401 Essential hypertension
Includes: high blood pressure; hyperpiesia; hyperpiesis; hypertension (arterial) (essential) (primary) (systemic); hypertensive vascular: degeneration; disease
DeVivo, 1993:5 Ischemic heart disease (ICD codes 410–414); Non ischemic heart disease (ICD codes 420–429); Cerebrovascular diseases (ICD codes 430–438); Diseases of arteries (ICD codes 440–448)
ISCHEMIC HEART DISEASE (410–414)
Includes:
that with mention of hypertension
Additional code to identify presence of hypertension (401.0–405.9)
410 Acute myocardial infarction
Includes:
cardiac infarction
coronary (artery):
embolism
occlusion
rupture
thrombosis
infarction of heart, myocardium, or ventricle
rupture of heart, myocardium, or ventricle
ST elevation (STEMI) and non-ST elevation (NSTEMI) myocardial infarction
any condition classifiable to 414.1–414.9 specified as acute or with a stated duration of 8 weeks or less
The following fifth-digit subclassification is for use with category 410:
0 episode of care unspecified
Use when the source document does not contain sufficient information for the assignment of fifth-digit 1 or 2.
1 initial episode of care
Use fifth-digit 1 to designate the first episode of care (regardless of facility site) for a newly diagnosed myocardial infarction. The fifth-digit 1 is assigned regardless of the number of times a patient may be transferred during the initial episode of care.
2 subsequent episode of care
Use fifth-digit 2 to designate an episode of care following the initial episode when the patient is admitted for further observation, evaluation or treatment for a myocardial infarction that has received initial treatment, but is still less than 8 weeks old.
411 Other acute and subacute forms of ischemic heart disease
412 Old myocardial infarction; Healed myocardial infarction
Past myocardial infarction diagnosed on ECG [EKG] or other special investigation, but currently presenting no symptoms
413 Angina pectoris
414 Other forms of chronic ischemic heart disease
Excludes:
arteriosclerotic cardiovascular disease [ASCVD] (429.2)
cardiovascular:
arteriosclerosis or sclerosis (429.2)
degeneration or disease (429.2)
OTHER FORMS OF HEART DISEASE (420–429)
420 Acute pericarditis
Includes:
acute:
mediastinopericarditis
myopericarditis
pericardial effusion
pleuropericarditis
pneumopericarditis
Excludes:
acute rheumatic pericarditis (391.0)
postmyocardial infarction syndrome [Dressler's] (411.0)
421 Acute and subacute endocarditis
422 Acute myocarditis
Excludes:
acute rheumatic myocarditis (391.2)
423 Other diseases of pericardium
Excludes:
that specified as rheumatic (393)
424 Other diseases of endocardium
Excludes:
bacterial endocarditis (421.0–421.9)
rheumatic endocarditis (391.1, 394.0–397.9)
syphilitic endocarditis (093.20–093.24)
425 Cardiomyopathy
Includes:
Myocardiopathy
426 Conduction disorders
427 Cardiac dysrhythmias
428 Heart failure
Code, if applicable, heart failure due to hypertension first (402.0–402.9, with fifth-digit 1 or 404.0–404.9 with fifth-digit 1 or 3)
CEREBROVASCULAR DISEASE (430–438)
Includes:
with mention of hypertension (conditions classifiable to 401–405)
Use additional code to identify presence of hypertension
430 Subarachnoid hemorrhage
Meningeal hemorrhage
Ruptured:
berry aneurysm
(congenital) cerebral aneurysm NOS
432 Other and unspecified intracranial hemorrhage
433 Occlusion and stenosis of precerebral arteries
The following fifth-digit subclassification is for use with category 433:
0 without mention of cerebral infarction
1 with cerebral infarction
Includes:
embolism of basilar, carotid, and vertebral arteries
narrowing of basilar, carotid, and vertebral arteries
obstruction of basilar, carotid, and vertebral arteries
thrombosis of basilar, carotid, and vertebral arteries
434 Occlusion of cerebral arteries
The following fifth-digit subclassification is for use with category 434:
0 without mention of cerebral infarction
1 with cerebral infarction
435 Transient cerebral ischemia
Includes:
cerebrovascular insufficiency (acute) with transient focal neurological signs and symptoms
insufficiency of basilar, carotid, and vertebral arteries
spasm of cerebral arteries
436 Acute, but ill-defined, cerebrovascular disease
Apoplexy, apoplectic:
NOS
attack
cerebral
seizure
Cerebral seizure
437 Other and ill-defined cerebrovascular disease
438 Late effects of cerebrovascular disease
Note: This category is to be used to indicate conditions in 430–437 as the cause of late effects. The “late effects” include conditions specified as such, or as sequelae, which may occur at any time after the onset of the causal condition.
DISEASES OF ARTERIES, ARTERIOLES, AND CAPILLARIES (440–448)
440 Atherosclerosis
Includes:
arteriolosclerosis
arteriosclerosis (obliterans) (senile)
arteriosclerotic vascular disease
atheroma
degeneration:
arterial
arteriovascular
vascular
endarteritis deformans or obliterans
senile:
arteritis
endarteritis
Excludes:
atheroembolism (445.01–445.89)
atherosclerosis of bypass graft of the extremities (440.30–440.32)
440.0 Of aorta
440.1 Of renal artery
440.2 Of native arteries of the extremities
440.3 Of bypass graft of the extremities
440.8 Of other specified arteries
440.9 Generalized and unspecified atherosclerosis
Garshick, 2005:6 Diseases of the heart (390–398, 402, 404, 410–14, 420–429); Other diseases of the circulatory system (401, 403, 405, 415–417, 430–38, 440–459); Diseases of the arteries, veins, and pulmonary circulation (415–417,440–459).
DISEASES OF THE CIRCULATORY SYSTEM (390–459)
ACUTE RHEUMATIC FEVER (390–392)
CHRONIC RHEUMATIC HEART DISEASE (393–398)
402 Hypertensive heart disease
403 Hypertensive kidney disease
405 Secondary hypertension
415 Acute pulmonary heart disease
416 Chronic pulmonary heart disease
417 Other diseases of pulmonary circulation
CEREBROVASCULAR DISEASE (430–438)
DISEASES OF ARTERIES, ARTERIOLES, AND CAPILLARIES (440–448)
DISEASES OF VEINS AND LYMPHATICS, AND OTHER DISEASES OF CIRCULATORY SYSTEM (451–459)
Analytical framework for pooled analysis of prevalence of cardiovascular diseases in adults with chronic SCI.
Prevalence was calculated as number of CVD events among total number of SCI patients in the study, standard error and confidence interval for population prevalence were calculated with Wilson estimate as followed:7
SEρ=√ [ρ*(1-ρ)]/[n+4]
95% level C confidence interval ρ±1.96*SEρ
Where p - prevalence, n- sample size
Pooled estimate as a weighted average:8
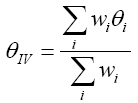
Weights are inverse of variance (standard error):

Standard error of pooled estimate:

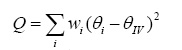
Heterogeneity (between-study variability) measured by:
Assumptions for random effects model: true effect sizes qi have a normal distribution with mean q and variance t2; t2 is the between-study variance
Between study variance:

Where:
wi are the weights from the fixed effect inverse-variance method
Q is the heterogeneity test statistic from before (either from inverse-variance method or Mantel-Haenszel method)
k is the number of studies, and
t2 is set to zero if Q<k-1
Random effect pooled estimate is weighted average:
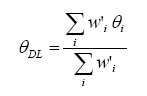
Weights used for the pooled estimate are similar to the inverse-variance, but now incorporate a component for between-study variation:

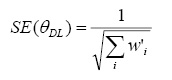
Standard error of pooled estimate
Heterogeneity between studies was quantified using the I-squared statistic.9. Statistical significance was analyzed at the 95% confidence level. All calculations were conducted using STATA software.10
References for Appendix E
- 1.
- National Library of Medicine (U.S.), National Center for Biotechnology Information (U.S.), National Institutes of Health (U.S.). PubMed central: an archive of life science journals. NCBI U.S. National Library of Medicine NIH Dept. of Health and Human Services [Digital archive searchable database]. Available at: http://www
.pubmedcentral.nih.gov/ - 2.
- Centers for Disease Control and Prevention (U.S.) NCfHSUS. ICD-9-CM, international classification of diseases, ninth revision, clinical modification. U.S. Dept. of Health and Human Services Centers for Disease Control and Prevention Health Care Financing Administration.
- 3.
- Groah SL, Weitzenkamp D, Sett P. et al. The relationship between neurological level of injury and symptomatic cardiovascular disease risk in the aging spinal injured. Spinal Cord. 2001 Jun;39(6):310–7. [PubMed: 11438852]
- 4.
- McGlinchey-Berroth R, Morrow L, Ahlquist M. et al. Late-life spinal cord injury and aging with a long term injury: characteristics of two emerging populations. J Spinal Cord Med. 1995 Jul;18(3):183–93. [PubMed: 7552423]
- 5.
- DeVivo MJ, Black KJ, Stover SL. Causes of death during the first 12 years after spinal cord injury. Arch Phys Med Rehabil. 1993 Mar;74(3):248–54. [PubMed: 8439250]
- 6.
- Garshick E, Kelley A, Cohen SA. et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord. 2005 Jul;43(7):408–16. [PMC free article: PMC1298182] [PubMed: 15711609]
- 7.
- Moore DS, McCabe GP. Introduction to the practice of statistics. 4th ed. New York: W.H. Freeman and Co.; 2003.
- 8.
- Der Simonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986 Sep;7(3):177–88. [PubMed: 3802833]
- 9.
- Higgins JP, Thompson SG, Deeks JJ. et al. Measuring inconsistency in meta-analyses. BMJ. 2003 Sep 6;327(7414):557–60. [PMC free article: PMC192859] [PubMed: 12958120]
- 10.
- Egger M, Smith GD, Altman DG. Systematic Reviews in Health Care. London: NetLibrary, Inc. BMJ Books; 2001.