This publication is provided for historical reference only and the information may be out of date.
Review of Current Medical and Scientific
Research Related to Disability and Chronic Fatigue Syndrome
AED Conference Center
Washington, DC
November 15, 2001
I. Introductions/Participants
Bernard J. Arseneau, DO, MPH, Chief Psychiatrist, Office of Disability, SSA.
Michael B. Brimacombe, PhD, Associate Professor, UMDNJ.
Lynn H. Gerber, MD, Chief, Rehabilitation Medicine Department, DHHS, NIH.
Marian James, PhD, Task Order Officer, AHRQ.
James F. Jones, MD, Professor of Pediatrics, University of Colorado School of Medicine, CDC.
Carolyn Kiefer, Policy Analyst, Office of Disability, SSA.
Gudrun Lange, PhD, Associate Professor, Clinical Neuropsychologist, UMDNJ.
Cindy Levine, MD, co-Principal Investigator, MetaWorks.
Paul H. Levine, MD, Clinical Professor of Medicine, GWU Medical Center.
Veronica Ludensky, BA, Research Assistant, MetaWorks.
Robert J. MacBride, MD, Medical Director, Disability Management, Prudential Group Insurance.
Benjamin H. Natelson, MD, Professor, Department of Neurosciences, UMDNJ.
Susan Ross, MD, FRCPC, EPC Director, President, MetaWorks.
Paul J. Scott, Policy Analyst, Office of Disability, SSA.
Frank Schuster, MD, Medical Officer - Musculoskeletal Branch, Office of Disability, SSA.
Norma C. Ware, PhD, Associate Professor, Harvard Medical School.
by phone:
Nelson Gantz, MD, co-Principal Investigator, MCP Hahnemann School of Medicine.
II. Social Security Administration (SSA) Comments on Current Policy (C. Kiefer)
The current state of the Disability Law has a sequential evaluation process in the SSA, which consists of five steps/questions:
- Are you doing work activity?
- Do you have a severe impairment? (symptoms, decrease in ability to function must be shown).
If no, then do not proceed with other steps. - Listings - no listings level with CFS.
- Functional capabilities (physical and mental activities, past employment must be investigated).
- Can you do anything else? (unskilled sedentary work).
Longitudinal record is very important in the determination of the disability; it must be shown that the impairment has lasted for at least 12 months.
Currently the SSA uses the ruling SSR 99-2p to guide the decisions about the disability status of patients with CFS. The SSA hopes to use this project and its conclusions to identify items that need to be revised to make the ruling more useful and helpful.
III. Introduction of MetaWorks (C. Levine)
Introduction of the MetaWorks team. Presentations of a brief history and description of MetaWorks Inc, the process it uses during systematic literature reviews and its goals for this project.
IV. Discussion of Causal Pathway (S. Ross)
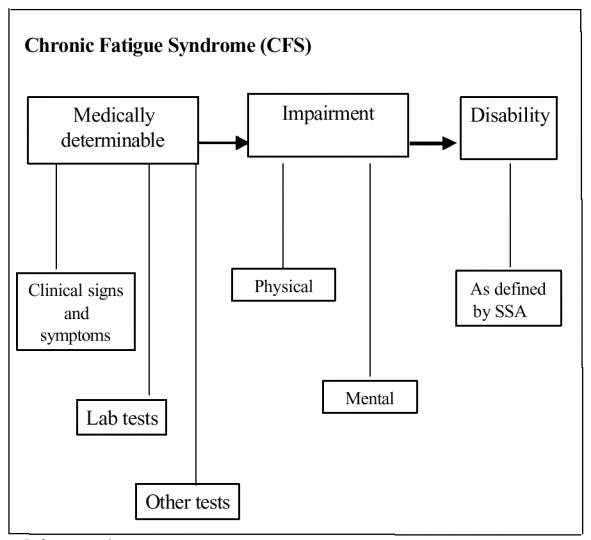
A Causal Pathway prepared especially for the purposes of this project was discussed, see Attachment A. All of the events described in this pathway take place within the CFS universe, i.e., only patients already diagnosed with CFS are included. Patients must have medically determinable condition (clinical signs and symptoms, lab results, or other), which leads to physical or mental impairment, which then leads to disability, as defined by the SSA.
V. Definition of disability and CFS (C. Levine)
It was agreed that 4 definitions for CFS will be used in the scope of this project. These include: CDC 1988, CDC 1994, Oxford, and Australian. See Attachment B for descriptions of these definitions.
Discussion of the definition of disability. Per SSA definitions, disability is based upon inability to work. The disabled person cannot do work that was done before and cannot adjust to other work, and the disability must be expected to last for at least a year.
In the current literature, impairment and loss of function are not well linked to disability. Objective disability outcome measurements should be used (functional limitations, capacity, functional impairment, dysfunction).
VI. Refinement of key questions (C. Levine)
Original Key Question 1
What is the evidence that individuals with CFS have a discrete physical impairment? What is the evidence that individuals with CFS have a coexisting mental impairment? For example, what is the evidence that comorbid psychiatric/neurologic conditions frequently reported in CFS are present and, if present, are a result of CFS or are an integral part of the CFS disease process?
Revised Key Question 1
What is the evidence that some individuals with CFS have discrete impairments that are associated with disability?
Impairment includes both physical and mental impairments.
Original Key Question 2
What is the evidence that there are specific clinical tests that can be used to reliably diagnose CFS, for example, are there specific anatomical, psychological, physiological, or medical imaging indices that are diagnostic for CFS?
Revised Key Question 2
It was agreed that this question does not pertain to disability and should be deleted.
Original Key Question 3
When cognitive deficits are alleged, what is the evidence that individuals with CFS have such deficits and what is the evidence that these potential deficits contribute to functional limitations or inability to do work activity?
Revised Key Question 3
Same as Revised Key Question 1.
Original Key Question 4
Do current neuropsychological tests reliably detect cognitive or mental impairments in the CFS population? Are there certain tests that are preferred in terms of reliability and validity? Are there certain tests or diagnostic tools that contain reliable correlations between test result(s) and either ability or inability to perform designated work-related functions (e.g., ability to relate to coworkers and supervision appropriately, ability to maintain concentration or pace, suitable memory capacity for work activities, etc.).
Revised Key Question 4
What is the evidence that in the CFS population, current neuropsychological tests detect cognitive or affective impairments associated with decreased ability to work?
Original Key Question 5
What treatments have been shown to be most effective for CFS in terms of restoring an individual's ability to do work activity?
Revised Key Question 5
What is the evidence that in some individuals with CFS, treatments are effective in restoring the ability to work?
Original Key Question 6
What are the patient characteristics that best define improvement or positive outcomes in the CFS population such that they experience improvement in functioning? Where it occurs, how is this improvement in functioning related to the ability to engage in work activity?
Revised Key Question 6
No change, but it was agreed that it was unlikely that the literature would allow us to address the last part of this question.
Original Key Question 7
What evidence is available from related fields (e.g., sleep medicine, autonomic nervous system abnormalities, endocrinology, gastrointestinal illness, neurocognitive therapy) that would be applicable to the assessment, functional evaluation, and treatment for CFS?
Revised Key Question 7
No change, although complete searches and reviews of the literature in other fields is beyond the scope of this project. SSA will discuss and propose a modified question.
It was agreed that this question will apply only to literature that pertains to CFS.
VII. Preliminary literature assessment (C. Levine)
It was agreed that the search needs to be expanded to 1988, to match the first operational definition of CFS, which was published by CDC in 1988. Many important studies about CFS were published immediately after 1988, and need to be included in this project. Number of citations identified will increase; however, the overall number of eligible studies may not change too much, given requirements that studies contain information regarding impairment or disability.
Pubmed, PsychINFO, Current Contents, and Cochrane Database will be the only electronic sources searched for this literature review. Also Journal of Chronic Fatigue Syndrome (JCFS), which is not indexed by Medline, will be searched.
Any study with > than 1 patient with CFS will be included, but individual case reports will not. Fibromyalgia, Gulf War Syndrome, or other related disorders without CFS will not be included within the scope of this project. Studies pertaining to multiple disorders will only be accepted if information regarding patients with CFS is separately extractable.
VIII. Conclusions/Next Steps (S. Ross)
- Definitional issues must be recognized regarding disability and impairment.
- MetaWorks will be "monists," not mind-body dualists.
- The words "mental" and "physical" will be removed from the key questions, and the general term impairment will be used instead.
- Four operational definitions of CFS will be used.
- Key questions will be revised as discussed.
- Literature search will be expanded as discussed.
IX. Action Items
MetaWorks to:
- Distribute meeting minutes.
- Contact members of the expert panel regarding serving on the Technical Experts Panel (TEP).
- Adopt questions and literature search recommendations as discussed in the panel.
SSA to:
- Review Key Question 7 and propose modifications.
Attachment A: Causal Pathway
References used:
1. Fukuda K, Straus SE, Hickie I, et al. The chronic fatigue syndrome: A comprehensive approach to its definition and study. Ann Intern Med 1994; 121: 953-9.
2. SSR 99-2p: Policy interpretation ruling Titles II and XVI: Evaluating cases involving chronic fatigure syndrome (CFS).
Attachment B: CFS Diagnostic Criteria
CDC 1988 CFS definition
- Major criteria:
- new onset of persistent or relapsing, debilitating fatigue in a person without a previous history of such symptoms that does not resolve with bedrest and that is severe enough to reduce or impair average daily activity to less than 50% of the patient's premorbid activity level for at least 6 months
- fatigue that is not explained by the presence of other evident medical or psychiatric illnesses
- Minor criteria:
- at least six symptoms plus at least two signs, or at least eight symptoms from the list below
- Symptoms:
- mild fever or chills
- sore throat
- painful adenopathy (posterior or anterior, cervical or axillary)
- generalized muscle weakness
- myalgias
- prolonged generalized fatigue after previously tolerated levels of physical activity
- generalized headaches
- migratory arthralgia without swelling or redness
- neuropsychologic complaints
- sleep disturbance
- main symptom complex developing over a few hours to a few days
- Physical Signs:
- low-grade fever
- nonexudative pharyngitis
- palpable or tender anterior or posterior, cervidal or axillary lymph nodes
From: Holmes GP, Kaplan JE, Gantz NM, et al. Chronic fatigue syndrome: A working case definition. Ann Intern Med 1988; 108: 387-9.
CDC 1994 CFS definition
- Clinically evaluated, unexplained, persistent or relapsing chronic fatigue lasting > 6 months
- of new or definite onset
- not the result of ongoing exertion
- not substantially alleviated by rest
- substantial reduction in previous levels of occupational, educational, social, or personal activities
- Clinical evaluation:
- History and Physical, Mental Status examination
- Laboratory screening including CBC, ESR, LFTs, TP, albumin, globulin, CA, PO4, glucose, BUN, CRE, electrolytes, TSH, urinalysis
- 4 symptoms concurrently present for > 6 months
- Sore throat
- Tender cervical or axillary lymph nodes
- Muscle pain
- Multijoint pain
- New headaches
- Unrefreshing sleep
- Postexertion malaise
- Exclusion criteria
- Active, unresolved, or suspected disease likely to cause fatigue
- Psychotic, melancholic or bipolar depression-(but not uncomplicated major depression)
- Psychotic disorders
- Dementia
- Anorexia or bulimia nervosa
- Alcohol or other substance misuse
- Severe obesity
From: Fukuda K, Straus SE, Hickie I, et al. The chronic fatigue syndrome: A comprehensive approach to its definition and study. Ann Intern Med 1994; 121: 953-9.
Oxford CFS definition
- Severe, disabling fatigue lasting > 6 months that:
- affects both physical and mental functioning
- is present for > 50% of the time
- Other symptoms may be present:
- myalgia
- sleep disturbances
- mood disturbance
- Exclusion criteria:
- Active, unresolved, or suspected disease likely to cause fatigue
- Psychotic, melancholic or bipolar depression-(but not uncomplicated major depression)
- Psychotic disorders
- Dementia
- Anorexia or bulimia nervosa
From: Sharpe MK, Archard LC, Banatvala JE, et al. A report - chronic fatigue syndrome: Guidelines for research. J R Soc Med 1991; 84: 118-21.
Australian CFS definition
- Disabling and prolonged feelings of physical tiredness or fatigue, exacerbated by physical activity.
- Present for at least 6 months.
- Unexplained by an alternative diagnosis reached by history, laboratory, or physical examinations.
- Accompanied by new onset of neuropsychological symptoms including impaired short-term memory and concentration, decreased libido, and depressed mood. These symptoms usually have their onset at the same time as the physical fatigue, but are typically less severe and less persistent than those seen in classic depressive illness.
- Exclusion criteria:
- Chronic medical condition that may result in fatigue
- History of schizophrenia, other psychotic illnesses, or bipolar affective disorder
- Drug or alcohol dependence makes CFS very unlikely.
From: Lloyd AR, Hickie I, Boughton CR, et al. Prevalence of chronic fatigue syndrome in an Australian population. Med J Aust 1990; 153: 522-8.
Publication Details
Copyright
Publisher
Agency for Healthcare Research and Quality (US), Rockville (MD)
NLM Citation
Levine C, Ganz N, Estok R, et al. Systematic Review of the Current Literature Related to Disability and Chronic Fatigue Syndrome. Rockville (MD): Agency for Healthcare Research and Quality (US); 2002 Dec. (Evidence Reports/Technology Assessments, No. 66.) Appendix B. Expert Meeting Information.