NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Dolor RJ, Melloni C, Chatterjee R, et al. Treatment Strategies for Women With Coronary Artery Disease [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2012 Aug. (Comparative Effectiveness Reviews, No. 66.)
This publication is provided for historical reference only and the information may be out of date.
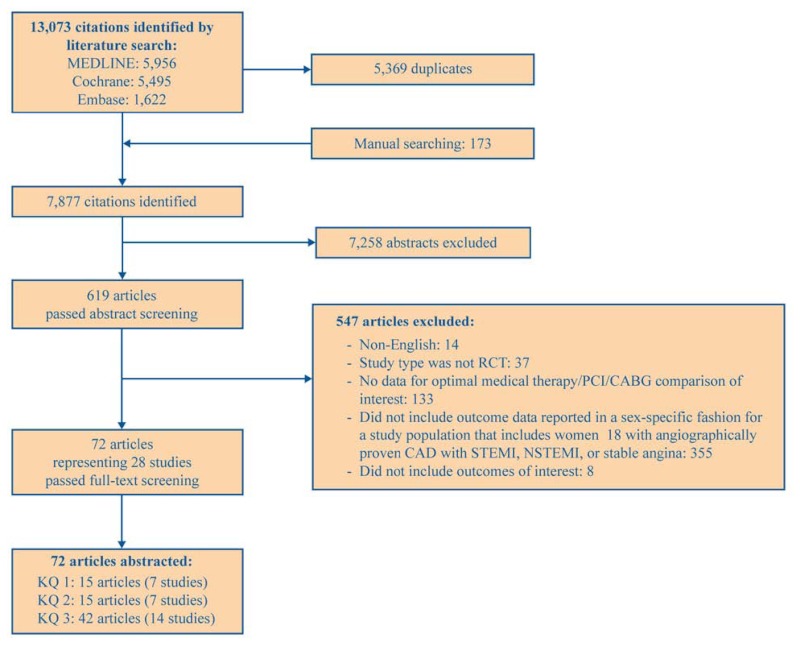
The flow of articles through the literature search and screening process is depicted in Figure 2. Of the 13,073 citations identified by our searches, 5,369 were duplicates. Manual searching identified an additional 173 citations for a total of 7,877 citations. After applying inclusion/exclusion criteria at the title/abstract level, 619 full-text articles were retrieved and screened. Of these, 547 articles were excluded at the full-text screening stage, with 72 articles (representing 28 studies) remaining for data abstraction. Appendix E provides a complete list of articles excluded at the full-text screening stage, with reasons for exclusion.
Key Question 1. Women With STEMI (PCI Vs. Fibrinolysis)
In women presenting with ST elevation myocardial infarction (STEMI):
- What is the effectiveness of percutaneous coronary intervention (PCI) versus fibrinolysis/supportive therapy on clinical outcomes (nonfatal MI, death, stroke, repeat revascularization, recurrent unstable angina, heart failure, repeat hospitalization, length of hospital stay, angina relief, quality of life, or cognitive effects)?
- Is there evidence that the comparative effectiveness of PCI versus fibrinolysis/supportive therapy varies based on characteristics such as:
- Age, race, or other demographic and socioeconomic risk factors?
- Coronary disease risk factors such as diabetes, chronic kidney disease, or other comorbid disease?
- Angiographic-specific factors (number of diseased vessels, vessel territory stenoses, left ventricular function, access site, or prior PCI or coronary artery bypass graft surgery [CABG] revascularization procedure)?
- Hospital characteristics (hospital volume, setting, guideline-based treatment protocols)?
- What are the significant safety concerns associated with each treatment strategy (i.e., adverse drug reactions, radiation exposure, access site complications, renal dysfunction, anaphylaxis, arrhythmias, stent thrombosis, bleeding, infections)?
Overview
STEMI is caused by the complete occlusion of an epicardial artery, leading to possible transmural infarction of the heart muscle. Treatment for patients with STEMI consists of reperfusion therapy (either pharmacological or catheter-based) to restore blood flow promptly in the occluded epicardial infarct-related artery. Pharmacological therapy consists of fibrinolysis or facilitated antithrombotic medications.29 In general, patients with STEMI are not treated with CABG (unless emergent from PCI complications) but do receive optimal medical therapy in addition to treatment directed at removing the clot. Studies assessing the effectiveness of immediate PCI compared with fibrinolytics or immediate PCI compared with conservative/supportive therapy were evaluated for KQ 1.
Key Points
- Description of included studies: Seven studies (6 good quality, 1 fair) evaluated PCI with or without supportive pharmacologic therapy versus fibrinolysis or other routine medical care for women with STEMI and included a total of 4,527 patients, of which 1,174 (26%) were women.
- Effectiveness of interventions: A meta-analysis of five studies (all good quality) reporting 30-day composite outcomes (primarily death/MI/stroke) showed that PCI was better than fibrinolysis in women (OR 0.50; 95% CI, 0.36 to 0.72) and men (OR 0.54; CI, 0.42 to 0.70). Strength of evidence favoring PCI over fibrinolysis was high at 30-day followup. However, there was insufficient evidence for assessing outcomes at 1 year. These findings also are limited in that all the studies were conducted with either balloon angioplasty or bare-metal stents. The current use of drug-eluting stents may lead to different practice patterns and, potentially, increase the effectiveness of PCI. Individual outcomes by sex were rarely reported for heart failure, repeat hospitalization, length of hospital stay, angina relief, quality of life, or cognitive effects.
- Modifiers of effectiveness: Two studies (1 good quality, 1 fair) reported subgroup analyses of demographic or clinical factors in women and included a total of 395 patients, of which 167 (32%) were women. Both studies assessed the influence of age on in-hospital mortality or composite clinical outcomes (death/heart failure/MI/stroke) and showed no age-related differences in PCI compared with optimal medical therapy. Therefore, there was insufficient evidence of the comparative effectiveness of treatment strategies among subgroups of women with STEMI, which precludes any meaningful conclusions.
- Safety concerns: Two good-quality studies reported safety concerns in women with STEMI and included a total of 1,532 patients, of which 367 (24%) were women. One study reported a lower nadir hematocrit in women receiving PCI versus fibrinolysis but no statistically significant differences in the requirement for blood transfusion. Another study reported the proportion of women with intracranial hemorrhage who received PCI versus accelerated tissue plasminogen activator (t-PA) (0% vs. 4.1%). No studies systematically collected radiation exposure, contrast reactions, access site complications, or stent thrombosis in women with STEMI undergoing PCI. Strength of evidence for safety concerns in STEMI studies was insufficient.
Detailed Synthesis
We identified seven studies36–42 that evaluated PCI with or without supportive pharmacologic therapy versus fibrinolysis or other routine medical care for women with STEMI. Of these seven studies, six were good quality, and one was fair quality. Table 3 presents a general description of these seven studies, including the study name, author, year, and related articles (i.e., study design and secondary papers); treatment comparisons evaluated; study population; and overall quality rating. Table 4 summarizes the women-specific outcomes (composite and individual) reported in these studies. Appendix F contains summary tables with sex-specific clinical outcomes for all followup time points.
KQ 1a. Effectiveness of Interventions
A meta-analysis was performed on studies with similar composite outcomes measured at similar time points. This meta-analysis was divided into followup intervals of short term (≤30 days) and long term (≥1 year). The SHOCK study,38 evaluating early revascularization versus medical stabilization, did not report 1-year data by sex, except for noting the lack of a treatment-by-sex interaction, and therefore was not included in the meta-analysis. Similarly, in the Minai study41 evaluating PCI versus no PCI, 3-year data reported no sex effect in a multivariate analysis; however, since the data were not reported by sex, this study also was excluded from the meta-analysis.
Short-Term Followup Studies
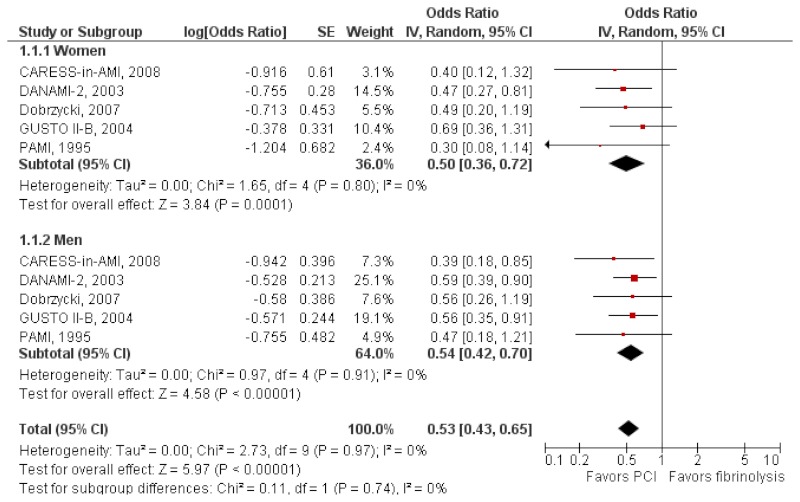
Five studies—CARESS-in-AMI,36 DANAMI-2,37 Dobrzycki,40 GUSTO II-B,39 and PAMI42—were included in the meta-analysis based on comparable composite outcomes (primarily death/MI/stroke) and followup time points of 30 days or in-hospital. The published results from Dobrzycki et al. were inverted to change the reference arm to fibrinolysis. The PAMI study event rates by treatment group and sex were converted into odds ratios. Table 5 presents the outcomes, odds ratios, and confidence intervals for the meta-analysis.
Forest plots for the random-effects model are shown in Figure 3. The summary odds ratio in women was 0.50 (95% CI, 0.36 to 0.72) and in men was 0.54 (CI, 0.42 to 0.70). The test for heterogeneity was nonsignificant. These results show that PCI was better than fibrinolysis in reducing death/MI/stroke in both sexes (p=0.0001 women, p<0.00001 men) at 30 days.
Intermediate-Term Followup Studies
Two studies—DANAMI-244 and Dobrzycki40—reported sex-specific clinical outcomes at 1 year. Table 6 presents the outcomes, odds ratios, and confidence intervals for PCI compared with fibrinolysis by sex. Due to the heterogeneous clinical outcomes, a meta-analysis was not conducted.
PCI Versus Fibrinolysis in High-Risk Groups
We identified two studies that evaluated a PCI or CABG strategy versus conservative/supportive medical therapy in high-risk groups.38,41 These studies were not included in the meta-analysis since the actual results by sex were not reported in the manuscript; instead both papers report the results of a multivariate analysis with sex as a covariate in the model. The SHOCK study38 was considered good quality and evaluated patients with cardiogenic shock and STEMI with a strategy of PCI or CABG within 6 hours versus initial medical stabilization that included fibrinolysis or insertion of an intra-aortic balloon pump (IABP). This study found that the early revascularization strategy was associated with a lower relative risk of death when compared with medical stabilization (risk ratio 0.72; 95% CI, 0.54 to 0.95). Analysis by sex did not identify any significant interaction by treatment arm. The study by Minai et al.41 was considered fair quality and evaluated PCI versus routine medical therapy without reperfusion in patients 80 years of age and older. There was no difference in the number of patients with the composite outcome of death/heart failure/repeat MI/stroke at 3 years between the treatment arms. No analysis by sex was done; however, in a multivariate analysis to evaluate factors associated with the composite outcome, sex was not found to be significantly associated with the outcome in the overall study population. This study was limited by the small sample size of 120 patients enrolled.
KQ 1b. Modifiers of Effectiveness
Two studies41,42 evaluating women with STEMI assessed the characteristics of interest and included a total of 515 patients, of which 167 (32%) were women. The PAMI study42 was considered good quality and evaluated patients randomized to PCI versus fibrinolysis with t-PA. No difference was found in in-hospital mortality among women receiving PCI versus t-PA who were under 65 years of age (0% vs. 4%; p=0.42) nor among women 65 and older (5.9% vs. 21.9%; p=0.58).
The study by Minai et al.41 evaluated PCI versus routine medical therapy without reperfusion in patients 80 years of age and older. The results are noted above. Appendix G contains a summary table with study data related to modifiers of effectiveness (subgroup analyses).
KQ 1c. Safety Concerns
Two good-quality studies reported safety concerns in women with STEMI and included a total of 1,532 patients, of which 367 (24%) were women. In the PAMI study42 evaluating PCI versus t-PA in STEMI patients, the mean nadir hematocrit in women with PCI was 30 ± 5 percent versus 33 ± 5 percent in women with t-PA (p=0.0002). However, there was no statistically significant difference in the requirement for blood transfusion in women with PCI versus t-PA (18% vs. 8.8%; p=0.16). In the GUSTO II-B study39 the proportion of women with intracranial hemorrhage was reported in women who received PCI versus accelerated t-PA (0% vs. 4.1%), but statistical analysis for this comparison was not done. Appendix H contains a summary table with study data related to safety concerns (harms).
Key Question 2. Women With UA/NSTEMI (Early Invasive Vs. Initial Conservative Therapy)
In women presenting with unstable angina or non-ST elevation myocardial infarction (UA/NSTEMI):
- What is the effectiveness of early invasive (PCI or CABG) versus initial conservative therapy on clinical outcomes (nonfatal MI, death, stroke, repeat revascularization, recurrent unstable angina, heart failure, repeat hospitalization, length of hospital stay, graft failure, angina relief, quality of life, or cognitive effects)?
- Is there evidence that the comparative effectiveness of early invasive versus initial conservative therapy varies based on characteristics such as:
- Age, race, or other demographic and socioeconomic risk factors?
- Coronary disease risk factors such as diabetes, chronic kidney disease, or other comorbid disease?
- Angiographic-specific factors (number of diseased vessels, vessel territory stenoses, left ventricular function, access site, or prior PCI or CABG revascularization procedure)?
- Hospital characteristics (hospital volume, setting, guideline-based treatment protocols)?
- What are the significant safety concerns associated with each treatment strategy (i.e., adverse drug reactions, radiation exposure, access site complications, renal dysfunction, anaphylaxis, arrhythmias, stent thrombosis, bleeding, infections)?
Overview
Unstable angina is caused by reversible ischemia of the epicardial arteries, whereas NSTEMI is caused by the partial obstruction of the epicardial arteries and results in myocardial tissue damage. Patients with UA/NSTEMI are not candidates for immediate pharmacological reperfusion (i.e., fibrinolysis). The optimal management of UA/NSTEMI has the twin goals of immediate relief of ischemia and the prevention of serious adverse outcomes (i.e., death or MI). Optimal management is best accomplished with aggressive medical therapy that includes anti-ischemic therapy, antithrombotic therapy, ongoing risk stratification, and in some cases the use of invasive procedures.
Following initiation of aggressive medical therapy, two treatment pathways have emerged for treating patients without ST-segment elevation.28 An “initial conservative strategy” calls for proceeding with an invasive evaluation only for those patients whose medical therapy fails (refractory angina or angina at rest or with minimal activity despite vigorous medical therapy) or in whom objective evidence of ischemia (dynamic electrocardiographic changes, high-risk stress test) is identified. The early invasive strategy triages patients to undergo an invasive diagnostic evaluation without first having a noninvasive stress test or having medical treatment fail. Patients treated with an early invasive strategy generally will undergo coronary angiography within 4 to 24 hours of admission; however, these patients also are treated with the usual UA/NSTEMI medications, including appropriate anti-ischemic, antiplatelet, and anticoagulant therapy. Therefore, studies assessing the effectiveness of early invasive versus initial conservative therapy were evaluated for KQ 2.
Key Points
- Description of included studies: Seven studies (6 good quality, 1 fair) compared early invasive therapy (PCI or CABG) with initial conservative therapy for women with UA/NSTEMI and included a total of 17,930 patients, of which 6,084 (34%) were women.
- Effectiveness of interventions: A meta-analysis of two good-quality studies reporting 6-month composite outcomes (death/MI) suggested a benefit of early invasive compared with initial conservative therapy in women (OR 0.77; 95% CI, 0.28 to 2.12), but early invasive therapy was superior to initial conservative therapy in men (OR 0.65; CI, 0.52 to 0.82; p=0.0002). At 1 year, a meta-analysis of five good-quality studies showed that composite outcomes (primarily death or MI) suggested a benefit for women who received early invasive therapy (OR 0.78; CI, 0.54 to 1.12) as well as for men (OR 0.88; CI, 0.64 to 1.20); however this benefit was not statistically significant. Finally, a meta-analysis of two good-quality studies with 5-year followup comparing early invasive and initial conservative therapy for the composite outcome of death or MI did not reach statistical significance in either sex. The summary odds ratio in women was 1.05 (CI, 0.81 to 1.35) and in men was 0.91 (CI, 0.53 to 1.56). The long-term analysis is limited by the low number of studies. Strength of evidence favoring an early invasive approach was low for women and high for men at 6-month followup; low for women and men at 1-year followup; and insufficient for women and low for men at 5-year followup. Similar to the STEMI studies, individual outcomes by sex were rarely reported for heart failure, repeat hospitalization, length of hospital stay, quality of life, or cognitive effects.
- Modifiers of effectiveness: Two good-quality studies comparing early invasive treatment with PCI with initial conservative treatment reported a subgroup analysis by risk stratification and included a total of 4,030 patients, of which 1,439 (36%) were women. These studies revealed conflicting results—one showed no difference in treatment outcomes in the intermediate- and high-risk groups; the other showed a higher event rate in women in the groups with moderate-to-high risk for thrombolysis in myocardial infarction (TIMI). Strength of evidence for modifiers of effectiveness for early invasive versus initial conservative treatments was insufficient.
- Safety concerns: One good-quality study (2,220 total patients, 757 women, 34% women) reported the harms associated with treatment of UA/NSTEMI by sex group but not the rates of events by treatment group. Bleeding in women undergoing PTCA was higher compared with men (adjusted OR 3.6; 95% CI, 1.6 to 8.3).51 However, bleeding related to CABG was similar in women and men with rates of 12.6 and 15 percent respectively. No studies systematically reported radiation exposure, contrast reactions, access site complications, stent thrombosis or infection, in women with UA/NSTEMI comparing initial conservative with early invasive therapy. Strength of evidence for safety concerns in these populations was insufficient.
Detailed Synthesis
We identified seven studies22,52–57 that evaluated the effect of early invasive therapy compared with initial conservative therapy for UA/NSTEMI and reported results by sex. Of these seven studies, six were good quality, and one was fair. Table 7 presents a general description of these seven studies, including the study name, author, year, and related articles (i.e., study design and secondary papers); treatment comparisons evaluated; study population; and overall quality rating. Table 8 summarizes the women-specific outcomes (composite and individual) reported in these studies. Appendix F contains summary tables with sex-specific clinical outcomes for all followup time points.
KQ 2a. Effectiveness of Interventions
A meta-analysis was performed on studies with similar composite outcomes measured at similar time points. This meta-analysis was divided into followup intervals of short term (6 months), intermediate term (1 year) and long term (5 years).
Short-Term Followup Studies
Two studies reporting 6-month outcomes—FRISC II60 and TACTICS TIMI-1851—were included in the meta-analysis. The TIMI III-B study57 (good quality) reported a shorter followup time point of 6 weeks and therefore was not included in this meta-analysis. In TIMI III-B, the proportion of women with the composite outcome of death/MI at 6 weeks was 6.1 percent in the early invasive arm and 8.9 percent in the initial conservative arm (p=0.24). The proportion of men with the same composite outcome was 7.8 percent and 7.3 percent, respectively (p=0.73). The RITA-2 study54 (fair quality) reported outcomes for angina grade 2+ or exercise time and likewise was not included in the meta-analysis. In RITA-2, the proportion of women with angina graded 2 or higher at 6 months was 22.8 percent for the early invasive arm, and 39.8 percent for the initial conservative arm. In men, the proportion with angina graded 2 or higher was 20.5 percent and 31.4 percent, respectively. For the TACTICS TIMI-18 study, we used the adjusted odds ratio for the composite outcome of death/MI. Table 9 presents the outcomes, odds ratios, and confidence intervals for the meta-analysis.
Forest plots for the random-effects model are shown in Figure 4. The summary odds ratio in women was 0.77 (95% CI, 0.28 to 2.12) and in men was 0.65 (CI, 0.52 to 0.82). The test for heterogeneity was significant in women (p=0.01), but it was nonsignificant in men. These results for short-term outcomes suggested a non–statistically significant benefit of early invasive compared with initial conservative therapy in women but demonstrated that early invasive was superior to initial conservative therapy in men (p=0.0002). The two trials resulted in conflicting conclusions in women versus men, despite having similar results for the overall population.
Intermediate-Term Followup Studies
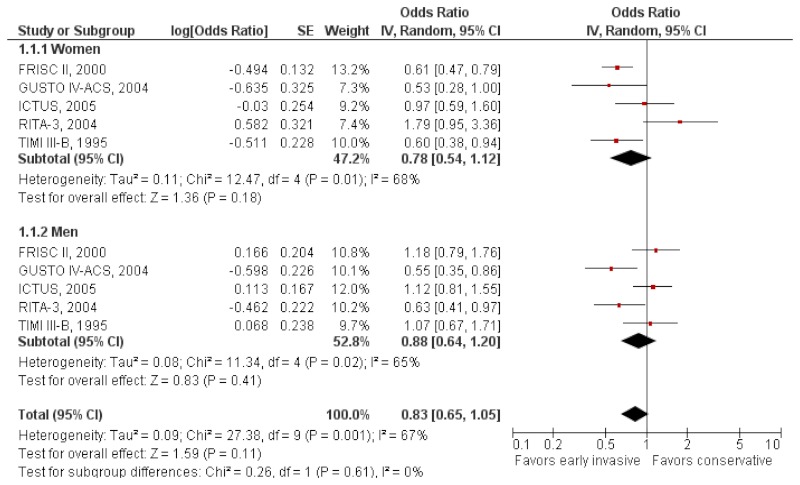
Five studies with 1-year data—FRISC II,59 GUSTO IV-ACS,53 ICTUS,56 RITA-3,22 and TIMI III-B64—were included in the meta-analysis. For the RITA-3 study, the adjusted odds ratio for the composite outcome of death/MI was selected for this analysis. For the ICTUS and TIMI III-B studies, event rates were converted to odds ratios. Table 10 presents the outcomes, odds ratios, and confidence intervals for the meta-analysis.
Forest plots for the random-effects model are shown in Figure 5. The summary odds ratio in women was 0.78 (95% CI, 0.54 to 1.12) and in men was 0.88 (CI, 0.64 to 1.20). The test for heterogeneity was significant in women (p=0.01) and men (p=0.02). These results show trends favoring early invasive therapy in 1-year outcomes although these benefits were not statistically significant in either women or men.
Long-Term Followup Studies
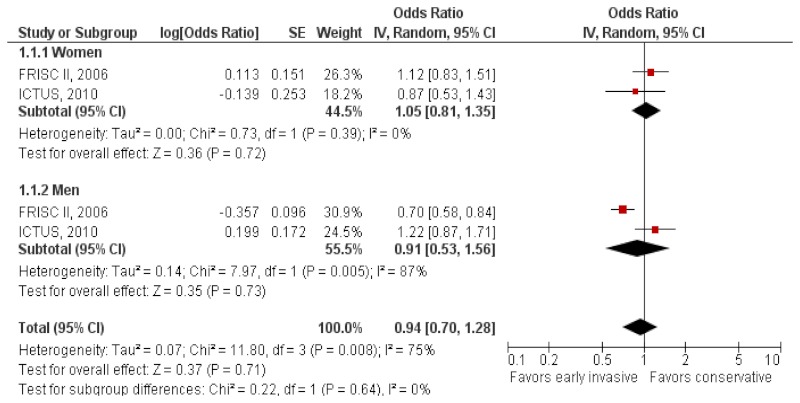
Two studies with 5-year, long-term data were included in the analysis: FRISC II58 and ICTUS.61 Table 11 presents the outcomes, odds ratios, and confidence intervals for the meta-analysis.
Forest plots for the random-effects model are shown in Figure 6. The summary odds ratio in women was 1.05 (95% CI, 0.81 to 1.35) and in men was 0.91 (CI, 0.53 to 1.56). The test for heterogeneity was significant in men (p=0.005) but not in women. Although these results demonstrate a slight trend favoring initial conservative therapy in women, given the small suggested benefit at 5 years, the wide confidence interval crossing 1, and the trend favoring early invasive therapy suggested at earlier time points and across time points in men — we cannot support firm conclusions. There was no evidence of a sex effect. The analysis is limited by the low number of studies.
Some of the analyses above showed heterogeneity in clinical outcomes between the FRISC II and ICTUS studies. The major heterogeneity in these studies arises from the rates and threshold of invasive treatment in the conservative arm. In the FRISC II study, more conservative strategies were used, thus leading to lower rates of invasive treatment in the conservative groups. In the ICTUS study, the selective invasive group was more liberal with the rates of invasive therapy and almost as high as the invasive arms of the other studies, thus explaining some of the potential differences in the results.
KQ 2b. Modifiers of Effectiveness
We identified two good-quality studies22,55 examining the effect of early invasive therapy compared with initial conservative therapy in women by subgroup; these included a total of 4030 patients, of which 1439 (36%) were women. The TACTICS TIMI-18 study55 found that there was no significant benefit to the treatment of women with intermediate-risk (3 to 4) or high-risk (5 to 7) TIMI scores on the primary composite outcome of death/MI/rehospitalization for acute coronary syndrome with early invasive therapy (OR 0.72; 95% CI, 0.45 to 1.16) compared with initial conservative therapy (OR 0.56; CI, 0.23 to 1.32).51 There also was no significant benefit of early invasive therapy on the primary composite outcome for those presenting with ST-segment changes (OR 0.66; CI, 0.38 to 1.15). However, there did seem to be a reduced risk of the primary composite outcome among women who had an elevated troponin level and who underwent early invasive treatment compared with conservative treatment (OR 0.56; CI, 0.32 to 0.97). Men with ST-segment changes and elevated troponin levels also seemed to benefit from early invasive therapy but not those in intermediate- or high-risk groups based on TIMI risk scores.51
The RITA-3 study22 also examined the effect of early invasive therapy compared with initial conservative therapy in women by subgroup based on risk, which was derived from components of the TIMI risk score and a couple other aspects of the participants’ presentation at randomization, including aspirin use and angina severity. This study, unlike the TACTICS TIMI-18 study, found a higher event rate among women in moderate- and high-risk groups who underwent early invasive therapy compared with initial conservative therapy, with event rates of 13.4 percent versus 3.4 percent for those in the moderate-risk group and 11.7 percent versus 8.2 percent for those in the higher risk group. Men with moderate and higher risk had lower event rates if they were in the early invasive arm compared with the initial conservative arm, with 5.4 percent versus 9.4 percent for those in the moderate-risk group and 10.3 percent versus 17.9 percent for those in the higher risk group. This study also examined the effect of intervention group by body mass index group and found no effect of body mass index on treatment effect in either women or men.22 Appendix G contains a summary table with study data related to modifiers of effectiveness (subgroup analyses).
KQ 2c. Safety Concerns
We identified one good-quality study55 (2,220 total patients, 757 women, 34% women) that reported the harms associated with treatment of UA/NSTEMI by sex group but not the rates of events by treatment group. The TACTICS TIMI-18 study, comparing early invasive therapy with initial conservative therapy, found that bleeding in women undergoing PTCA was higher than in men (adjusted OR 3.6; 95% CI, 1.6 to 8.3).51 They found, however, that the bleeding related to CABG was similar in women and men with rates of 12.6 and 15 percent, respectively. Appendix H contains a summary table with study data related to safety concerns (harms).
Key Question 3. Women With Stable or Unstable Angina
In women with stable or unstable angina:
- What is the effectiveness of the following treatment strategies on clinical outcomes (nonfatal MI, death, stroke, repeat revascularization, recurrent unstable angina, heart failure, repeat hospitalization, length of hospital stay, graft failure, angina relief, quality of life, or cognitive effects)?
- Strategy 1. Revascularization (PCI or CABG) versus optimal medical therapy in women with stable angina
- Strategy 2. PCI versus CABG in women with stable or unstable angina
- Is there evidence that the comparative effectiveness of revascularization versus optimal medical therapy varies based on characteristics such as:
- Age, race, or other demographic and socioeconomic risk factors?
- Coronary disease risk factors such as diabetes, chronic kidney disease, or other comorbid disease?
- Angiographic-specific factors (number of diseased vessels, vessel territory stenoses, left ventricular function, access site, or prior PCI or CABG revascularization procedure)?
- CABG-specific factors such as type of surgery performed, cardiopulmonary bypass mode (normothermic versus hypothermic), on-pump versus off-pump, type of cardioplegia used (blood versus crystalloid), or use of saphenous vein grafts, single or bilateral internal mammary artery grafts, or other types of bypass grafts?
- Hospital characteristics (hospital volume, setting, guideline-based treatment protocols)?
- What are the significant safety concerns associated with each treatment strategy (i.e., adverse drug reactions, radiation exposure, access site complications, renal dysfunction, anaphylaxis, arrhythmias, stent thrombosis, bleeding, infections)?
Overview
Angina resulting from progressive narrowing of the coronary arteries is the initial manifestation of ischemic heart disease in approximately 50 percent of patients.30 Most angina is a sign of significant CAD, defined angiographically as a stenosis with ≥70 percent diameter in at least one major epicardial artery segment or with ≥50 percent diameter in the left main coronary artery. However, some angina is caused by stenotic lesions of lesser diameters, which have much less prognostic significance.30
Chronic stable angina is classified as pain that classically occurs with moderate to severe exertion, is milder in nature, and relieved with rest or sublingual nitroglycerin. Unstable angina (UA) is defined as angina with at least one of three features: (1) it occurs at rest or with minimal exertion, (2) it is severe and of recent onset (within the past 4 to 6 weeks), and/or (3) it occurs in a crescendo pattern (i.e., more severe, more prolonged, or more frequent than previously experienced). UA and NSTEMI have a fairly similar pathophysiology, mortality rate, and management strategy when compared with STEMI; therefore they are often grouped together as UA/NSTEMI in clinical guidelines and trial populations.
The treatment of angina has two major purposes. The first is to prevent MI and death and thereby increase the quantity of life. The second is to reduce symptoms of angina and occurrence of ischemia, which should improve the quality of life.30 All patients with stable or unstable angina are candidates for optimal medical therapy and also may be candidates for PCI or CABG based on findings from coronary angiography or if symptoms persist despite optimal medical therapy.
For KQ 3, we evaluated two sets of treatment strategies:
- Revascularization (PCI or CABG) versus optimal medical therapy in women with stable angina
- PCI versus CABG in women with either stable or unstable angina
Strategy 1: Revascularization Versus Optimal Medical Therapy in Stable Angina
Key Points
- Description of included studies: Five studies (all good quality) compared revascularization (PCI or CABG) with optimal medical therapy for women with stable angina and included a total of 6,851 patients, of which 1,285 (19%) were women.
- Effectiveness of interventions: A meta-analysis of three good-quality studies with long-term (4- to 5-year) followup on the composite outcomes (death/MI/revascularization) comparing PCI or CABG with optimal medical therapy showed that revascularization was significantly better than optimal medical therapy in women with stable angina (OR 0.64; 95% CI, 0.47 to 0.89; p=0.008 for PCI strategy trials; OR 0.56 [CI, 0.32 to 0.96; p=0.04] for CABG strategy trials; and OR 0.59 [CI, 0.43 to 0.81; p=0.001] for either PCI or CABG). However, for men with stable angina, the analysis did not show statistically significant findings between revascularization and optimal medical therapy, though it demonstrated a trend favoring optimal medical therapy compared with PCI (OR 1.03; CI, 0.79 to 1.33 for PCI strategy trials). This suggested small benefit however has a wide confidence interval crossing 1 and is not supported by additional time periods or by the evidence in women. Conversely, evidence suggested that CABG or either PCI or CABG reduced outcomes compared with optimal medical therapy in men (OR 0.62; CI, 0.31 to 1.24 for CABG strategy trials; and OR 0.71; CI, 0.49 to 1.02 for either PCI or CABG)—again these findings were not statistically significant. Strength of evidence favoring revascularization for women was moderate in the PCI strategy, low in the CABG strategy, and moderate for both types of revascularization combined. In men, the strength of evidence was low for the PCI, CABG, and combined revascularization strategies.
- Modifiers of effectiveness: No studies were identified that evaluated women presenting with stable angina; therefore data are insufficient.
- Safety concerns: No studies were identified that evaluated women presenting with stable angina; therefore data are insufficient.
Detailed Synthesis
We identified five studies65–69 that reported outcomes for women with stable angina. Of these five studies, all were good quality. Two studies compared PCI with optimal medical therapy,65,66 one compared CABG with optimal medical therapy,67 and one compared medical management with transmyocardial revascularization (TMR).69 Table 12 presents a general description of these five studies, including the study name, author, year, and related articles (i.e., study design and secondary papers); treatment comparisons evaluated; study population; and overall quality rating. Table 13 summarizes the women-specific outcomes (composite and individual) reported in these studies. Appendix F contains summary tables with sex-specific clinical outcomes for all followup time points.
KQ 3a. Effectiveness of Interventions
Long-Term Followup Studies
Three studies were included in a meta-analysis: COURAGE,65 MASS II,68 and STICH.67 These studies had similar followup times (4 to 5 years, except a 10-year followup in the MASS II study) and comparable outcomes (composite, death). No results were available for the short- or intermediate-term outcomes. The TMR study by Allen et al.69 was excluded since the results were reported in a different fashion (i.e., whether sex had an impact on outcome for the TMR patients) and could not be incorporated into the meta-analysis. The OAT study66 was excluded from the meta-analysis since the study subjects were enrolled ≥7 days after an acute MI with revascularization or medical therapy for an occluded artery; the patient population was deemed to be quite different from those enrolled in the other studies. The MASS II study numbers were inverted to place PCI in the comparison group. Table 14 presents the outcomes, odds ratios, and confidence intervals for the meta-analyses.
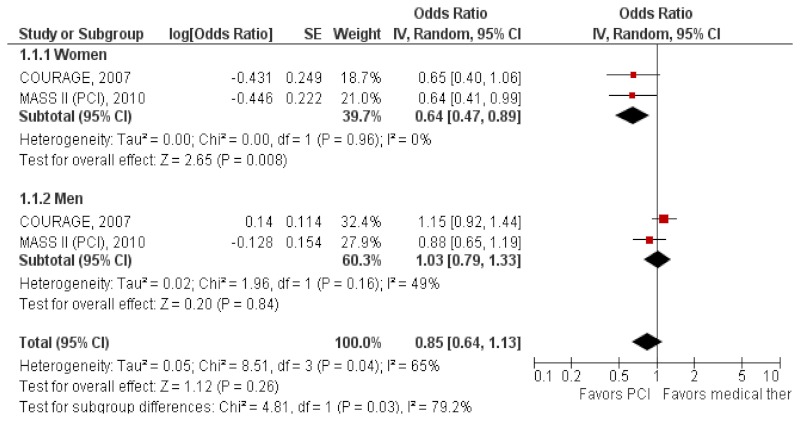
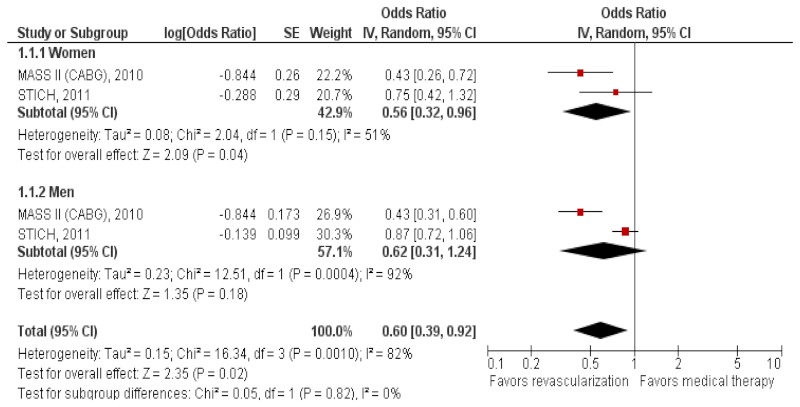
Forest plots for the random-effects model are shown in Figures 7, 8, and 9. Separate analyses were created for (a) primarily PCI strategy, (b) primarily CABG strategy, and (c) either type of revascularization strategy compared with optimal medical therapy for the purposes of creating a sensitivity analysis given the subtle differences in patient populations and revascularization methods used in those studies.
The primarily PCI strategy (Figure 7) studies included COURAGE and MASS II (PCI). The summary odds ratio in women was 0.64 (95% CI, 0.47 to 0.89) and in men was 1.03 (CI, 0.79 to 1.33). The test for heterogeneity was not significant for women and men. The results showed that PCI reduced death/MI in women but not in men.
The primarily CABG strategy (Figure 8) studies included MASS II (CABG) and STICH. The summary odds ratio in women was 0.56 (CI, 0.32 to 0.96) and in men was 0.62 (CI, 0.31 to 1.24). The test for heterogeneity was not significant for women (p=0.15) but was significant for men (p=0.0004). These results show that CABG was significantly better in reducing cardiovascular events than optimal medical therapy was in women (effect size p=0.04) but not in men.
We then combined all studies utilizing both types of revascularization strategies (PCI or CABG)—COURAGE, MASS II, and STICH. Figure 9 shows the forest plot for the random-effects model using the MASS II (CABG) cohort. The summary odds ratio in women was 0.59 (CI, 0.43 to 0.81) and in men was 0.71(CI, 0.49 to 1.02). The test for heterogeneity was not significant in women, but was significant in men. These results showed that revascularization was significantly better in reducing cardiovascular events than optimal medical therapy in women. Similar results were obtained if the model was run with the MASS II (PCI) cohort (figure not shown). For men, revascularization and optimal medical therapy were not statistically different.
KQ 3b. Modifiers of Effectiveness
No studies were identified that evaluated women presenting with stable angina related to modifiers of the effectiveness of revascularization versus optimal medical therapy.
KQ 3c. Safety Concerns
No studies were identified that evaluated women presenting with stable angina related to safety concerns for revascularization versus optimal medical therapy.
Strategy 2: PCI Versus CABG in Stable/Unstable Angina
Key Points
- Description of included studies: 10 studies (8 good quality, 2 fair) compared PCI with CABG in women with stable/unstable angina and included a total of 6,289 patients, of which 1,583 (25%) were women.
- Effectiveness of interventions: A meta-analysis of two good-quality studies reporting 30-day death rates showed no statistically significant difference between PCI and CABG and therefore did not support evidence of a sex effect. The summary odds ratio in women was 0.68 (95% CI, 0.24 to 1.93) and in men was 1.36 (CI, 0.44 to 4.24). These two studies did, however, suggest a potentially greater benefit with PCI in women and with CABG in men. The low number of studies and wide confidence intervals made this a less robust finding and one that should be interpreted with caution. For 1-year outcomes (death/MI/stroke), a meta-analysis of two good-quality studies suggested potentially better outcomes in the CABG group for both sexes however this findings was not statistically significant (CI crosses 1). The summary odds ratio in women was 1.30 (CI, 0.69 to 2.45) and in men was 1.19 (CI, 0.84 to 1.70). For long-term (>2 years) outcomes (death/MI/stroke), a meta-analysis of four good-quality studies although not statistically significant, suggested better outcomes in the CABG group in women (OR 1.17; CI, 0.90 to 1.54); however in men, CABG was significantly better than PCI (OR 1.63; CI, 1.20 to 2.23, p= 0.002). Strength of evidence favoring CABG over PCI was low for women and men at 30-day and 1-year followups, and low for women and high for men at ≥2-year followup.
- Modifiers of effectiveness: One good-quality study (915 total patients, 249 [27%] women) evaluated the comparative effectiveness of PCI versus CABG in diabetic patients with stable/unstable angina. The survival rate at 7 years was similar in diabetic women from both treatment groups. However in diabetic men, those treated with CABG had higher survival than those who underwent PCI. Strength of evidence for modifiers of effectiveness for PCI versus CABG in stable/unstable angina was insufficient.
- Safety concerns: One good-quality study (1205 total patients, 283 [23%] women) reported harms associated with PCI compared with CABG among women with unstable angina or NSTEMI and found that bleeding associated with PCI was higher in women compared with men. Strength of evidence for safety concerns for PCI versus CABG in stable/unstable angina was insufficient.
Detailed Synthesis
We identified 10 studies68,78–86 that evaluated PCI versus CABG for women presenting with unstable angina or NSTEMI. Of these 10 studies, 8 were good quality, and 2 were fair quality. Table 15 presents a general description of these 10 studies, including the study name, author, year, and related articles (i.e., study design and secondary papers); treatment comparisons evaluated; study population; and overall quality rating. Table 16 summarizes the women-specific outcomes (composite and individual) reported in these studies. Appendix F contains summary tables with sex-specific clinical outcomes for all followup time points.
KQ 3a. Effectiveness of Interventions
A meta-analysis of studies was performed on those with similar composite outcomes measured at similar time points. This meta-analysis was divided into followup intervals of short term (≤30 days), intermediate term (1 year), and long term (≥2 years).
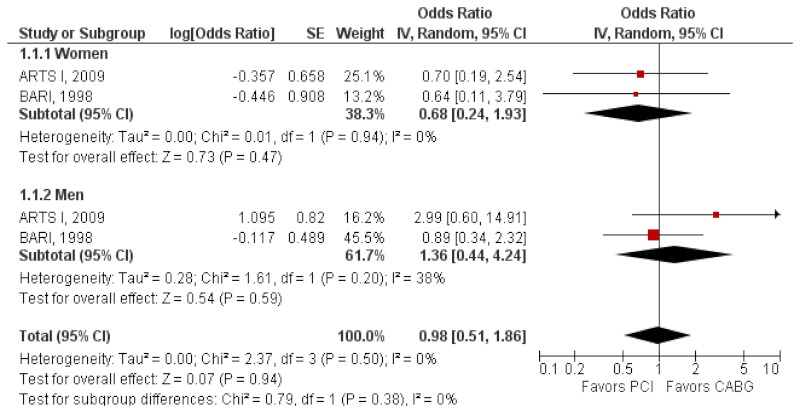
Short-Term Followup Studies
Two studies with short-term (30-day or in-hospital) outcomes—ARTS I78 and BARI79—were included in the meta-analysis. For both studies, the reported event rates/percentages were converted into odds ratios. Table 17 presents the outcomes, odds ratios, and confidence intervals for the meta-analysis.
Forest plots for the random-effects model are shown in Figure 10. The summary odds ratio in women was 0.68 (95% CI, 0.24 to 1.93) and in men was 1.36 (CI, 0.44 to 4.24). The test for heterogeneity was nonsignificant. The findings were not statistically significant for demonstrating a benefit in PCI and CABG, although the odds ratios suggested a possible sex effect, with PCI showing more benefit in women and CABG showing more benefit in men, but the confidence intervals are too wide to support firm conclusions.
Intermediate-Term Followup Studies
Two studies with 1-year outcomes—ARTS I78 and CARDia84—were included in the meta-analysis. In the SYNTAX study, 83 there was no difference in the primary composite outcome (death/MI/stroke, or repeat revascularization) at 1 year between patients undergoing CABG and PCI (13.6% vs. 15.8%). No sex data by treatment in this fair-quality study were provided, but being female was a significant predictor of 1-year major adverse cardiovascular events (OR 0.50; 95% CI, 0.27 to 0.91; p=0.02 [interaction effect not reported]). The SYNTAX study was excluded from the meta-analysis since it did not report subgroup results by sex. The PRECOMBAT study85 did not report sex-specific data at 1 year, so this study was not included in this intermediate-term followup analysis (but data reported at 2 years are included in the long-term followup analysis below). Event data from the ARTS I study were transformed into risk ratios. Table 18 presents the outcomes, odds ratios, and confidence intervals for the meta-analysis.
Forest plots for the random effects model are shown in Figure 11. The summary odds ratio in women was 1.30 (95% CI, 0.69 to 2.45) and in men was 1.19 (CI, 0.84 to 1.70). The test for heterogeneity was nonsignificant. These results show lower events in the CABG group for both sexes, but this benefit was not statistically significant.
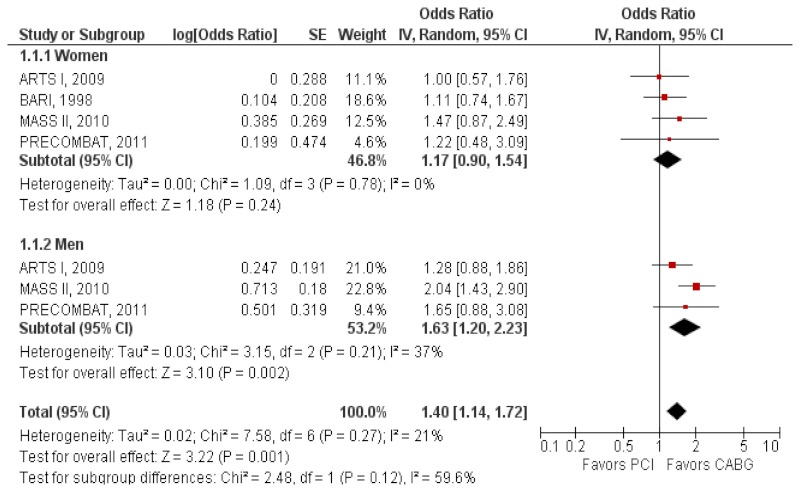
Long-Term Followup Studies
To assess the long-term effect at ≥2 years, four studies were included in the meta-analysis: ARTS I (3-year),78 BARI (5-year),79 MASS II (10-year),68 and PRECOMBAT (2-year).85 Results of the ARTS I and BARI studies were transformed into risk ratios. For the BARI study, the survival rates were converted into death rates. For women, the death rates for CABG and PCI were 24 percent of 240 and 26 percent of 249, respectively. For men, survival rates by treatment group were not reported. The MASS II results were inverted to hazard ratios <1 favoring PCI and hazard ratios >1 favoring CABG. The GABI study86 was excluded from the meta-analysis because it did not present data by sex. The GABI study randomized 359 patients (66 women) with angina CCS class II–IV, under age 75, and coronary multiple-vessel disease requiring revascularization of at least 2 major coronary vessels to either PCI or CABG. The authors report that the hazard ratio for death following PCI or CABG was not different between men and women at the 13-year followup. Table 19 presents the outcomes, odds ratios, and confidence intervals for the meta-analysis.
Forest plots for the random effects model are shown in Figure 12. The summary odds ratio in women was 1.17 (95% CI, 0.90 to 1.54) and in men was 1.63 (CI, 1.20 to 2.23). The test for heterogeneity was nonsignificant. Similar to the intermediate-term outcomes, there was no definitive evidence of a sex effect. In men, CABG was significantly better than PCI (p=0.002); in women, results suggest lower events in the CABG group, but it was not statistically significant (p=0.24).
KQ 3b. Modifiers of Effectiveness
We identified one good-quality study (915 total patients, 249 [27%] women) in which the long-term survival rate (7 years) in diabetic women was addressed. In the BARI study,79 this subgroup analysis was not initially specified but was requested by the safety and monitoring board during the course of the trial on the basis of concurrent reports from another study. Survival rate at 7 years was significantly higher among diabetic patients (n=353) treated with CABG compared with those undergoing PCI (74.6% vs. 55.7%), a difference that remained significant in men (77.9% vs. 51.5%) but not in women (74.3% vs. 61.0%). Appendix G contains a summary table with study data related to modifiers of effectiveness (subgroup analyses).
KQ 3c. Safety Concerns
We identified one good-quality study78 (1,205 total patients, 283 [23%] women) that addressed significant safety concerns and, specifically, risk of major bleeding in women (n=283). The ARTS I study was designed to compare CABG with PCI combined with stent implantation for the treatment of patients with multiple-vessel disease. Major bleeding was higher in women undergoing PCI compared with men (7.2% vs. 0.2%, p<0.001) but not among those assigned to CABG (1.4% vs. 2.8%). After adjusting for baseline characteristics, major bleeding complications remained higher among women in the PCI group (OR 29.4; 95% CI, 5.3 to 500; p=0.001 women vs. men) compared with the CABG group (OR 1.5; CI, 0.4 to 10.1, p=0.58 women vs. men). Appendix H contains a summary table with study data related to safety concerns (harms).
Figures
Tables
Table 3KQ 1: Study characteristics of RCTs evaluating women with STEMI
| Study Author/Year Related Articles | Description of Study | # Subjects | Quality |
|---|---|---|---|
| CARESS-in-AMI Di Mario et al., 200836 and Di Mario et al., 200443 | Title: Immediate angioplasty vs. standard therapy with rescue angioplasty after thrombolysis in the Combined Abciximab Reteplase Stent Study in Acute Myocardial Infarction (CARESS-in-AMI): an open, prospective, randomized, multicentre trial Comparator: Immediate PCI with fibrinolysis (reteplase) vs. fibrinolysis (reteplase) with rescue PCI Components of medical therapy: Clopidogrel (300 mg bolus on arrival, then 75 mg once daily 1 to 12 months after stent implantation). Beta blockers, angiotensin-converting enzyme inhibitors, and statins were administered to all patients unless contraindicated. | Total: 600 Women: 128 (21%) | Good |
| DANAMI-2 Andersen et al., 200337 and Mortensen et al., 200744 Nielsen et al., 201045 Busk et al., 200946 Busk et al., 200847 | Title: A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction Comparator: PCI vs. fibrinolysis (accelerated t-PA) Components of medical therapy: Aspirin 300 mg, IV beta-blocker (20 mg of metoprolol), IV unfractionated heparin (5000 U bolus, then 1000 U/hr). | Total: 1,572 Women: 417 (27%) | Good |
| Dobrzycki et al., 200740 | Title: Transfer with GP IIb/IIIa inhibitor tirofiban for primary percutaneous coronary intervention vs. on-site thrombolysis in patients with ST elevation myocardial infarction (STEMI): a randomized open-label study for patients admitted to community hospitals Comparator: Transfer with tirofiban for primary PCI vs. onsite fibrinolysis (streptokinase) Components of medical therapy: Aspirin 325 mg daily. Additional treatment was administered at the discretion of the physician. | Total: 401 Women: 105 (26%) | Good |
| GUSTO II-B Tamis-Holland et al., 200439 | Title: Benefits of direct angioplasty for women and men with acute myocardial infarction: results of the Global Use of Strategies to Open Occluded Arteries in Acute Coronary Syndromes Angioplasty (GUSTO II-B) Angioplasty Substudy Comparator: PCI vs. fibrinolysis (accelerated t-PA) Components of medical therapy: Not reported. | Total: 1,137 Women: 260 (23%) | Good |
| Minai et al., 200241 | Title: Long-term outcome of primary percutaneous transluminal coronary angioplasty for low-risk acute myocardial infarction in patients older than 80 years: a single-center, open, randomized trial Comparator: PCI vs. optimal medical therapy (without fibrinolysis) Components of medical therapy: IV heparin; IV nitroglycerin (0.5 mg/min/kg) for 24 hours after admission. Aspirin, other cardiovascular medications (calcium channel blockers, beta-blockers, and angiotensin-converting enzyme inhibitors administered at the discretion of the physician. | Total: 120 Women: 60 (50%) | Fair |
| PAMI Stone et al., 199542 | Title: Comparison of in-hospital outcome in men with outcome in women treated by either thrombolytic therapy or primary coronary angioplasty for acute myocardial infarction Comparator: PCI vs. fibrinolysis (t-PA) Components of optimal medical therapy: IV unfractionated heparin for 3–5 days, Nitroglycerin for at least 24 hours, followed by topic or oral nitrates. Aspirin 325 mg/daily, diltiazem 30 to 60 mg x 4 times a day; use of beta-blockers and IV lidocaine was left to investigator discretion. | Total: 395 Women: 107 (27%) | Good |
| SHOCK Hochman et al., 200138 and Hochman et al., 200648 Hochman et al., 199949 Hochman et al., 199950 | Title: One-year survival following early revascularization for cardiogenic shock Comparator: Early invasive revascularization (PCI or CABG within 6 hours) vs. initial medical stabilization (thrombolysis, IABP) Components of optimal medical therapy: Aspirin, IV unfractionated heparin, as recommended by AHA/ACC guidelines and at discretion of local investigator. | Total: 302 Women: 97 (32%) | Good |
CABG = coronary artery bypass graft; IABP = intra-aortic balloon pump; IV = intravenous; PCI = percutaneous coronary intervention; RCT = randomized controlled trial; STEMI = ST elevation myocardial infarction; t-PA = tissue plasminogen activator
Table 4KQ 1: Outcomes reported in RCTs evaluating women with STEMI
| Study | Composite Outcomea (Timing) Anticipated Effect Size | Deatha (Timing) | MI (Timing) | Stroke (Timing) | Revascularization (Timing) | Other (Timing) |
|---|---|---|---|---|---|---|
| CARESS-in-AMI36,43 | Total mortality/reinfarction/refractory MI (30 days) Powered to detect >50% RRR | |||||
| DANAMI-237,44–47 | Total mortality/nonfatal MI/stroke (30 days, 3 years; median 7.8 years) Powered to detect 40% RRR | Yes (30 days, 3 years) | Angina (30 days, 1 year) SF-36 (30 days, 1 year) | |||
| Dobrzycki et al.40 | Total mortality/nonfatal MI/stroke (30 days, 1 year) Powered to detect 50% RRR | Yes (30 days, 1 year) | ||||
| GUSTO II-B39 | Total mortality/nonfatal MI/nonfatal disabling stroke (30 days) Powered to detect 40% RRR | Yes (30 days) | Yes (30 days) | Yes (30 days) | Intracranial hemorrhage (30 days) | |
| Minai et al.41 | Total mortality/heart failure/repeat MI/stroke (3 years) Primary outcome & effect size not specified | |||||
| PAMI42 | Death/reinfarction (in hospital) Powered to detect 50% RRR | Yes (in hospital) | Yes (in hospital) | Yes (in hospital) | Recurrent ischemia (in hospital) Length of stay (in hospital) | |
| SHOCK38,48–50 | Powered to detect 25% RRR | Yes (1 year) |
MI = myocardial infarction; RRR = relative risk reduction; STEMI = ST elevation myocardial infarction
- a
Primary outcome in italics.
Table 5Sex results for STEMI on composite outcomes (short-term)
| Study (Comparison) | Outcome | Women (95% CI) | Men (95% CI) | Overall (95% CI) |
|---|---|---|---|---|
| CARESS-in-AMI (immediate PCI with reteplase vs. reteplase with rescue PCI) | Death/MI/refractory ischemia (30 days) | 0.40 (0.12 to 1.31) | 0.39 (0.18 to 0.85) | 0.40 (0.21 to 0.76) |
| DANAMI-2 (immediate PCI vs. accelerated t-PA ) | Death/MI/stroke (30 days) | 0.47 (0.27 to 0.81) | 0.59 (0.39 to 0.90) | 0.55 (0.38 to 0.76) |
| Dobrzycki (transfer for primary PCI vs. onsite streptokinase ) | Death/MI/stroke (30 days) | 0.49 (0.20 to 1.18) | 0.56 (0.26 to 1.18) | 0.51 0.29 to 0.91) |
| GUSTO II-B (PCI vs. accelerated t-PA) | Death/MI/stroke (30 days) | 0.69 (0.36 to 1.32) | 0.56 (0.35 to 0.91) | 0.67 (0.47 to 0.97) |
| PAMI (PCI vs.t-PA ) | Death/MI (in-hospital) | 0.30 (0.08 to 1.16) | 0.47 (0.18 to 1.19) | 0.40 (0.18 to 0.85) |
CI = confidence interval; MI = myocardial infarction; PCI = percutaneous coronary intervention; t-PA = tissue plasminogen activator
Table 6Sex results for STEMI on clinical outcomes (intermediate-term)
| Study (Comparison) | Outcome | Women (95% CI) | Men (95% CI) | Overall (95% CI) |
|---|---|---|---|---|
| DANAMI-2 (immediate PCI vs. accelerated t-PA) | Angina | 0.86 (0.50 to 1.49) | 0.86 (0.61 to 1.20) | NR |
| Dobrzycki (transfer for primary PCI vs. onsite streptokinase ) | Death/MI/stroke | 0.40 (0.17 to 0.94) | 0.62 (0.35 to 1.09) | 0.53 (0.33 to 0.84) |
CI = confidence interval; NR = not reported; PCI = percutaneous coronary intervention; t-PA = tissue plasminogen activator
Table 7KQ 2: Study characteristics of RCTs evaluating women with UA/NSTEMI
| Study Author/Year Related Articles | Description of Study | # of Subjects | Quality |
|---|---|---|---|
| FRISC II Lagerqvist et al., 200152 and Lagerqvist et al., 200658 Wallentin et al., 200059 Anonymous, 199960 | Title: Is early invasive treatment of unstable coronary artery disease equally effective for both women and men? FRISC II Study Group Investigators Comparator: Early invasive treatment with revascularization (PCI, type not specified, for 1- or 2-vessel CAD; CABG for 3-vessel CAD or left main disease) vs. initial conservative strategy Components of optimal medical therapy: Aspirin 300 to 600 mg (initial), then 75 to 320 mg daily. Beta blockade (unless contraindicated). Organic nitrates and calcium antagonists as needed. Lowering of cholesterol with statins, angiotensin converting-enzyme inhibitors for left-ventricular dysfunction, and aggressive antidiabetic treatment were recommended according to modern treatment guidelines. | Total: 2,457 Women: 749 (30%) | Good |
| GUSTO IV-ACS Ottervanger et al., 200453 | Title: Association of revascularisation with low mortality in non-ST elevation acute coronary syndrome, a report from GUSTO IV-ACS Comparator: Early invasive management vs. initial conservative treatment within 30 days. A total of 2265 (30%) patients underwent revascularization: 789 patients CABG, 1450 patients PCI, and 26 both CABG and PCI. Type of PCI was not specified. Components of optimal medical therapy: Aspirin for 30 days if not contraindicated. IV unfractionated heparin as bolus and infusion for 48 hours or low molecular weight heparin (dalteparin) subcutaneously every 12 hours for 5 to 7 days or until a revascularisation procedure or discharge. Continuation of antithrombin therapy with unfractionated or low molecular weight heparin was left at the discretion of the investigator. | Total: 7,800 Women: 2,896 (37%) | Good |
| ICTUS de Winter et al., 200556 and Damman et al., 201061 | Title: Early invasive vs. selectively invasive management for acute coronary syndromes Comparator: Early invasive therapy with revascularization vs. selective invasive strategy (initial conservative) Components of optimal medical therapy: Aspirin (300 mg at randomization then 75 mg daily); enoxaparin (1 mg/kg twice daily subcutaneously for 48 hours), Clopidogrel (300 mg immediately, followed by 75 mg daily) in combination with aspirin was recommended after the drug was approved in 2002 for the indication of acute coronary syndromes; intensive lipid-lowering therapy, preferably 80 mg of atorvastatin daily or the equivalent. | Total: 1,200 Women: 320 (27%) | Good |
| RITA-2 Anonymous, 199754 | Title: Coronary angioplasty vs. medical therapy for angina: the second Randomised Intervention Treatment of Angina (RITA-2) trial. RITA-2 trial participants Comparator: Early invasive therapy with PCI (primarily PTCA, but stent could be used if PTCA failed) vs. initial conservative Components of optimal medical therapy: Aspirin, unless contraindicated. Antianginal medication for symptom relief. Beta-adrenoceptor blocker with a calcium antagonist and/or long-acting nitrate in maximally tolerated doses. Lipid-lowering drugs prescribed at the discretion of the supervising clinician. | Total: 1,018 Women: 183 (8%) | Fair |
| RITA-3 Clayton et al., 200422 and Fox et al., 200262 | Title: Do men benefit more than women from an interventional strategy in patients with unstable angina or non-ST elevation myocardial infarction? The impact of gender in the RITA-3 trial Comparator: Early invasive with PCI (type at discretion of investigator) vs. initial conservative Components of optimal medical therapy: Aspirin; enoxaparin 1 mg/kg twice daily subcutaneously for 2 to 8 days. Antianginal treatment chosen by the supervising clinician, including a beta-blocker unless contraindicated. | Total: 1,810 Women: 682 (38%) | Good |
| TACTICS TIMI-18 Cannon et al., 200155 and Glaser et al., 200251 Cannon et al., 199863 | Title: Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban Comparator: Early invasive with PCI (type not specified) vs. initial conservative Components of optimal medical therapy: Aspirin 325 mg daily (unless contraindicated); IV unfractionated heparin (5000 U bolus, then 1000 U/hour for 48 hours); tirofiban (loading dose 0.4 μg/kg per minute for a period of 30 minutes, then 0.1 μg/kg/min for 48 hours or until revascularization, and for at least 12 hours after PCI; beta blockers (82%), nitrates (94%), and lipid-lowering agents (52%). | Total: 2,220 Women: 757 (34%) | Good |
| TIMI III-B Anonymous, 199457 and Anderson et al., 199564 | Title: Effects of tissue plasminogen activator and a comparison of early invasive and conservative strategies in unstable angina and non-Q-wave myocardial infarction. Results of the TIMI IIIB Trial Comparator: Early invasive with PCI (type not specified) vs. initial conservative Components of optimal medical therapy: Anti-ischemic therapy consisting of a beta-blocker (metoprolol 50 mg p.o. q 12 hours), a calcium antagonist (diltiazem 30 mg p.o. q 6 hours), and a long-acting nitrate (isosorbide dinitrate 10 mg p.o. q 8 hours) or larger doses and supplemented by sublingual nitroglycerin pm. IV heparin. Aspirin 325 mg daily was given on the second day and continued for 1 year. | Total: 1,425 Women: 497 (35%) | Good |
CABG = coronary artery bypass graft; PCI = percutaneous coronary intervention; NSTEMI = non-ST elevation myocardial infarction; PTCA: percutaneous transluminal coronary angioplasty; RCT = randomized controlled trial; UA = unstable angina
Table 8Outcomes reported in RCTs evaluating women with UA/NSTEMI
| Study | Composite Outcomea (Timing) Anticipated Effect Size | Death (Timing) | MI (Timing) | Stroke (Timing) | Revascularization (Timing) | Other (Timing) |
|---|---|---|---|---|---|---|
| FRISC II52,58–60 | Death/MI or both (6 months, 1 year, 5 years) Powered to detect 32% difference | |||||
| GUSTO IV-ACS53 | Not reported by sex Powered to detect 25% reduction in primary endpoint of death/MI | Yes (1 year) | ||||
| ICTUS56,61 | Death/MI/rehospitalization for angina (1 year) Death/spontaneous MI (5 years) Powered to detect 25% RRR | |||||
| RITA-254 | Death/MI (median followup of 2.7 years) Powered to detect 15% difference | Angina grade 2+ (6 months) Exercise time (6 months) | ||||
| RITA-322,62 | Death/MI (1 year) Death/MI/refractory angina (4 months, 1 year) Powered to detect 33% RRR | Yes (1 year) | ||||
| TACTICS TIMI-1851,55,63 | Death/MI/rehospitalization for acute coronary syndrome (6 months) Death/MI (6 months) Powered to detect 25% difference | Yes (6 months) | ||||
| TIMI III-B57,64 | Death/MI/failed symptom-limited exercise treadmill test (6 weeks) Death/MI (6 weeks, 1 year) Powered to detect 30% RRR |
MI = myocardial infarction; RRR = relative risk reduction; NSTEMI = non-ST elevation myocardial infarction; UA = unstable angina
- a
Primary outcome in italics.
Table 9Sex results for UA/NSTEMI on composite outcomes (short-term)
| Study (Comparison) | Outcome | Women (95% CI) | Men (95% CI) | Overall (95% CI) |
|---|---|---|---|---|
| FRISC II (early invasive vs. initial conservative) | Death/MI | 1.26 (0.80 to 1.97) | 0.64 (0.49 to 0.84) | 0.78 (0.62 to 0.98) |
| TACTICS TIMI-18 (early invasive vs. initial conservative) | Death/MI | 0.45 (0.24 to 0.88) | 0.68 (0.0.43 to 1.05) | 0.74 (0.54 to 1.00) |
CI = confidence interval; MI = myocardial infarction; PCI = percutaneous coronary intervention
Table 10Sex results for UA/NSTEMI on composite outcomes (intermediate-term)
| Study (Comparison) | Outcome | Women (95% CI) | Men (95% CI) | Overall (95% CI) |
|---|---|---|---|---|
| FRISC II (early invasive vs. initial conservative) | Death/MI | 0.61 (0.47 to 0.79) | 1.18 (0.79 to 1.76) | 0.74 (0.60 to 0.92) |
| GUSTO IV-ACS (revascularization in 30 days vs. initial conservative) | Death | 0.53 (0.28 to 1.00) | 0.55 (0.35 to 0.85) | 0.53 (0.37 to 0.77) |
| ICTUS (early invasive vs. selective invasive) | Death/MI/rehospitalization for angina | 0.97 (0.59 to 1.60) | 1.12 (0.81 to 1.56) | 1.07 (0.87 to 1.33) |
| RITA-3 (early invasive vs. initial conservative) | Death/MI | 1.79 (0.95 to 3.35) | 0.63 (0.41 to 0.98) | 0.91 (0.67 to 1.25) |
| TIMI III-B (early invasive vs. initial conservative) | Death/MI | 0.60 (0.38 to 0.93) | 1.07 (0.67 to 1.70) | 0.88 (0.64 to 1.21) |
CI = confidence interval; MI = myocardial infarction
Table 11Sex results for UA/NSTEMI on composite outcomes (long-term)
| Study (Comparison) | Outcome | Women (95% CI) | Men (95% CI) | Overall (95% CI) |
|---|---|---|---|---|
| FRISC II (early invasive vs. initial conservative) | Death/MI | 1.12 (0.83 to 1.50) | 0.70 (0.59 to 0.86) | 0.81 (0.69 to 0.95) |
| ICTUS (early invasive vs. selective invasive) | Death/MI | 0.87 (0.53 to 1.43) | 1.22 (0.87 to 1.71) | 1.29 (1.00 to 1.66) |
CI = confidence interval; MI = myocardial infarction
Table 12KQ 3 Strategy 1: Study characteristics of RCTs evaluating women with stable angina (PCI/CABG vs. optimal medical therapy)
| Study Author/Year Related Articles | Description of Study | # of Subjects | Quality |
|---|---|---|---|
| Allen et al., 200469 and Allen et al., 199970 | Title: Transmyocardial revascularization: 5-year follow-up of a prospective randomized multicenter trial Comparator: Surgical revascularization (CABG with transmyocardial revascularization) vs. optimal medical therapy Components of optimal medical therapy: Not reported. | Total: 222 Women: 61 (27%) | Good |
| COURAGE Boden et al., 200765 and Mancini et al., 200971 Boden et al., 200672 | Title: Optimal medical therapy with or without PCI for stable coronary disease Comparator: PCI (type not specified) or CABG if PCI failed vs. optimal medical therapy Components of optimal medical therapy: Aspirin (81 to 325 mg per day) or 75 mg of clopidogrel per day, if aspirin intolerance was present. Metoprolol, amlodipine, and isosorbide mononitrate, alone or in combination, along with either lisinopril or losartan; aggressive therapy to lower low-density lipoprotein cholesterol levels (simvastatin alone or in combination with ezetimibe) with a target level of 60 to 85 mg per deciliter (1.55 to 2.20 mmol per liter). | Total: 2,287 Women: 338 (15%) | Good |
| MASS II Hueb et al., 201068 and Hueb et al., 200473 Hueb et al., 200774 | Title: Ten-year follow-up survival of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease Comparator: PCI vs. optimal medical therapy; CABG vs. optimal medical therapy Components of optimal medical therapy: Nitrates, aspirin, beta blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, or a combination of these drugs unless contraindicated. Lipid-lowering agents, particularly statins, were also prescribed, along with a low-fat diet, on an individual basis. | Total: 611 Women: 196 (32%) | Good |
| OAT Hochman et al., 200666 and Hochman et al., 200575,76 | Title: Coronary intervention for persistent occlusion after myocardial infarction Comparator: PCI (or CABG if PCI failed) vs. optimal medical therapy Components of optimal medical therapy: Aspirin, anticoagulation if indicated, angiotensin-converting enzyme inhibition, beta blockade, and lipid-lowering therapy, unless contraindicated. Thienopyridine therapy was initiated before PCI and continued for 2 to 4 weeks after stenting. After reports of the efficacy of prolonged treatment with a thienopyridine after MI, the recommendation was changed to 1 year in both study groups. | Total: 2,166 Women: 476 (22%) | Good |
| STICH Velazquez et al., 201167 and Velazquez et al., 200777 | Title: Coronary-artery bypass surgery in patients with left ventricular dysfunction Comparator: CABG vs. optimal medical therapy Components of optimal medical therapy: Unless contraindicated, optimal medical therapy included angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or both; beta blocker; aldosterone antagonist; and antiplatelet agents adjusted to optimal doses within 30 days after randomization. Statin, diuretic, and digitalis use was individualized to patient-specific indications. The use of implantable defibrillators was encouraged as part of medical therapy and was used in compliance with standard guidelines. | Total: 1,212 Women: 148 (12%) | Good |
CABG = coronary artery bypass graft; CAD = coronary artery disease; MI = myocardial infarction; PCI = percutaneous coronary intervention; PTCA = percutaneous transluminal coronary angioplasty
Table 13KQ 3 Strategy 1: Outcomes reported in RCTs evaluating women with stable angina (PCI/CABG vs. optimal medical therapy)
| Study | Composite Outcomea (Timing) Anticipated Effect Size | Deatha (Timing) | MI (Timing) | CVA (Timing) | Revascularization (Timing) | Othera (Timing) |
|---|---|---|---|---|---|---|
| Allen et al.69,70 | Effect size not reported | Yes (5.7 years) | Angina relief (5.7 years) | |||
| COURAGE65,71,72 | Death/MI (median 4.6 years) Powered to detect 22% RRR | |||||
| MASS II68,73,74 | Death/MI/angina requiring revascularization (10 years) Powered to detect 2-fold difference | |||||
| OAT66,75,76 | Death/MI/heart failure (4 years, 7 years) Powered to detect 25% reduction | |||||
| STICH67,77 | Powered to detect 25% reduction in mortality | Yes (5 years) |
CABG = coronary artery bypass grafting; CVA = cerebrovascular accident; MI = myocardial infarction; PCI = percutaneous coronary intervention; RRR = relative risk reduction
- a
Primary outcome in italics.
Table 14Sex results for stable angina on composite outcomes (long-term)
| Study (Comparison) | Outcome | Women (95% CI) | Men (95% CI) | Overall (95% CI) |
|---|---|---|---|---|
| COURAGE (PCI [or CABG if PCI failed] vs. optimal medical therapy) | Death/MI | 0.65 (0.40 to 1.06) | 1.15 (0.91 to 1.42) | 1.05 (0.87 to 1.27) |
| MASS II (PCI vs. optimal medical therapy) | Death/MI/revascularization | 0.64 (0.41 to 0.98) | 0.88 (0.65 to 1.19) | 0.79 (0.62 to 1.01) |
| MASS II (CABG vs. optimal medical therapy) | Death/MI/revascularization | 0.43 (0.26 to 0.72) | 0.43 (0.31 to 0.61) | 0.43 (0.32 to 0.56) |
| STICH (CABG vs. optimal medical therapy) | Death | 0.75 (0.42 to 1.31) | 0.87 (0.72 to 1.06) | 0.86 (0.72 to 1.04) |
CI = confidence interval; CABG = coronary artery bypass graft; MI = myocardial infarction; PCI = percutaneous coronary intervention
Table 15KQ 3 Strategy 2: Study characteristics of RCTs evaluating women with stable or unstable angina (PCI vs. CABG)
| Study Author/Year Related Articles | Description of Study | # of Subjects | Quality |
|---|---|---|---|
| ARTS I Vaina et al., 200978 and van den Brand, et al., 200287 Serruys et al., 199988 Voudris et al., 200689 Anonymous, 199990 | Title: Effect of gender differences on early and mid-term clinical outcome after percutaneous or surgical coronary revascularisation in patients with multivessel coronary artery disease: insights from ARTS I and ARTS II Comparator: PCI (BMS) vs. CABG Components of medical therapy: Not reported. | Total: 1,205 Women: 283 (23%) | Good |
| BARI Jacobs et al., 199879 and Gibbons et al., 200191 Anonymous, 200792 Lombardero et al., 200293 Anonymous, 200094 Hlatky et al., 199595 Rogers et al., 199596 Sutton-Tyrrell et al., 199897 Mullany et al., 199998 Anonymous, 199699 | Title: Better outcome for women compared with men undergoing coronary revascularization: a report from the bypass angioplasty revascularization investigation (BARI) Comparator: PCI (type not specified) vs. CABG Components of medical therapy: Not reported. | Total: 915 Women: 249 (27%) | Good |
| CABRI Anonymous, 199580 | Title: First-year results of CABRI (Coronary Angioplasty vs. Bypass Revascularisation Investigation) Comparator: PCI (PTCA) vs. CABG Components of medical therapy: Aspirin; fish oils and lipid-lowering agent were allowed; individual patient management followed the established practice at each participating center. | Total: 1,054 Women: 234 (22%) | Good |
| CARDia Kapur et al., 201084 and Kapur et al., 2005100 | Title: Randomized comparison of percutaneous coronary intervention with coronary artery bypass grafting in diabetic patients. 1-year results of the CARDia (Coronary Artery Revascularization in Diabetes) trial Comparator: PCI (BMS or DES) vs. CABG Components of medical therapy: Glycoprotein IIb/IIIa, clopidogrel, and aspirin. | Total: 510 Women: 132 (26%) | Good |
| EAST King et al., 200081 and King et al., 1995101 King et al., 1994102 Zhao et al., 1996103 | Title: Eight-year mortality in the Emory Angioplasty vs. Surgery Trial (EAST) Comparator: PCI (type not specified) vs. CABG Components of medical therapy: Not reported. | Total: 392 Women: 103 (26%) | Good |
| GABI Kaehler et al., 200586 and Hamm et al., 1994104 | Title: 13-year follow-up of the German angioplasty bypass surgery investigation Comparator: PCI (type not specified) vs. CABG Components of medical therapy: Not reported (discretion of treating provider). | Total: 359 Women: 66 (18%) | Good |
| MASS II Hueb et al., 201068 and Hueb et al., 200473 Hueb et al., 200774 | Title: Ten-year followup survival of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease Comparator: PCI (type not specified) vs. CABG Components of medical therapy: Nitrates, aspirin, beta blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, or a combination of these drugs unless contraindicated. Lipid-lowering agents, particularly statins, were also prescribed, along with a low-fat diet, on an individual basis. | Total: 611 Women: 196 (32%) | Good |
| PRECOMBAT Park et al., 201185 | Title: Randomized Trial of Stents versus Bypass Surgery for Left Main Coronary Artery Disease Comparator: PCI (DES) vs. CABG Components of medical therapy: Before or during PCI: aspirin plus clopidogrel (loading dose, 300 mg) or ticlopidine (loading dose, 500 mg). After PCI: 100 mg/day aspirin indefinitely and 75 mg/day clopidogrel or 250 mg/day ticlopidine for at least 6 months. Medications after CABG were selected according to the policy of the institution or physician. | Total: 600 Women: 141 (24%) | Good |
| SOS Zhang et al., 200482 and Zhang et al., 2003105 Stables et al., 1999106 | Title: Relative benefit of coronary artery bypass grafting vs. stent-assisted percutaneous coronary intervention for angina pectoris and multivessel coronary disease in women vs. men (one-year results from the Stent or Surgery trial) Comparator: PCI (BMS) vs. CABG Components of medical therapy: Not reported. | Total: 908 Women: 206 (23%) | Fair |
| SYNTAX Morice et al., 201083 | Title: Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial Comparator: PCI (type not specified) vs. CABG Components of medical therapy: In the PCI arm, clopidogrel for 6 months, with aspirin therapy indefinitely. | Total: 705 Women: 185 (26%) | Fair |
BMS= bare-metal stent; CABG = coronary artery bypass graft; CAD = coronary artery disease; DES = drug-eluting stent; PCI = percutaneous coronary intervention; PTCA = percutaneous transluminal coronary angioplasty; RCT = randomized controlled trial
Table 16KQ 3 Strategy 2: Outcomes reported in RCTs evaluating women with stable or unstable angina (PCI vs. CABG)
| Study | Composite Outcomea (Timing) Anticipated Effect Size | Deatha (Timing) | MI (Timing) | CVA (Timing) | Revascularization (Timing) | Other (Timing) |
|---|---|---|---|---|---|---|
| ARTS I78,87–90 | Death/CVA/MI/CABG/repeat PCI (30 days, 1 year, 3 years, 5 years) Death/CVA (30 days, 1 year, 3 years) Death/MI/CVA (30 days, 1 year, 3 years, 5 years) MI/CVA/PTCA (5 years) Powered to detect 7% difference in favor of CABG | Yes (30 days, 1 year, 3 years, 5 years) MACE-free survival (30 days, 1 year, 3 years) | Yes (30 days, 1 year, 3 years, 5 years) | Yes (5 years) (30 days, 1 year, 3 years, 5 years) | Yes (30 days, 1 year, 3 years, 5 years) | Quality of life (3 years) Bleeding (in hospital) |
| BARI79,91–99 | Effect size not reported | Cumulative survival rate (5 year, 7 years, 10 years) | Yes (in hospital) | Yes (10 years) | Angina status (4 years, 10 years) Congestive heart failure (in hospital) | |
| CABRI80 | Powered to detect 60% reduction in mortality in PCI group | Yes (1 year) | Angina (1 year) | |||
| CARDia84,100 | Death/MI/stroke repeat revascularization (1 year) Death/MI/CVA (1 year) Powered for OR of 0.69 in favor of PCI (upper CI 1.3) | |||||
| EAST81,101–103 | Powered for 25% reduction | Survival (3 years, 8 years) | ||||
| GABI86,104 | Powered for 15% difference in success rates as therapeutically equivalent | Yes (13 years) | Primary outcome was freedom from angina (not reported by sex) | |||
| MASS II68,73,74 | Death/MI/angina requiring revascularization (10 years) Powered to detect 2-fold difference | |||||
| PRECOMBAT85 | Death/MI/stroke/ischemia-driven target-vessel revascularization (1 year, 2 years) Powered to detect 7% difference | |||||
| SOS82,105,106 | Powered for event rate of 5% in CABG arm and 10% in PCI arm | Primary outcome not reported by sex | Quality of life (6 months, 1 year) Angina frequency (6 months, 1 year) Physical limitation (6 months, 1 year) | |||
| SYNTAX83 | Death/MI/CVA/repeat revascularization (1 year) Powered for clinically relevant difference of 5% |
CABG = coronary artery bypass grafting; CVA = cerebrovascular accident; MACE = major adverse cardiovascular event; MI = myocardial infarction; OR = odds ratio; PCI = percutaneous coronary intervention; RRR = relative risk reduction
- a
Primary outcome in italics.
Table 17Sex results for stable/unstable angina on composite outcomes (short-term)
| Study (comparison) | Outcome | Women (95% CI) | Men (95% CI) | Overall (95% CI) |
|---|---|---|---|---|
| ARTS I (PCI vs. CABG) | Death (30 days) | 0.70 (0.19 to 2.51) | 2.99 (0.60 to 14.91) | NR |
| BARI (PCI vs. CABG) | Death (in-hospital) | 0.64 (0.11 to 3.86) | 0.89 (0.34 to 2.31) | 0.83 (0.36 to 1.93) |
CI = confidence interval; CABG = coronary artery bypass graft; NR = not reported; PCI = percutaneous coronary intervention
Table 18Sex results for stable/unstable angina on composite outcomes (intermediate-term)
| Study (Comparison) | Outcome | Women (95% CI) | Men (95% CI) | Overall (95% CI) |
|---|---|---|---|---|
| ARTS I (PCI vs. CABG) | Death/MI/stroke | 1.05 (0.51 to 2.21) | 1.27 (0.81 to 1.98) | NR |
| CARDia (PCI vs. CABG) | Death/MI/stroke | 2.13 (0.68 to 6.68) | 1.07 (0.59 to 1.93) | 1.25 (0.75 to 2.09) |
CI = confidence interval; CABG = coronary artery bypass graft; NR = not reported; PCI = percutaneous coronary intervention
Table 19Sex results for stable/unstable angina on composite outcomes (long-term)
| Study (Comparison) | Outcome | Women (95% CI) | Men (95% CI) | Overall (95% CI) |
|---|---|---|---|---|
| ARTS I (PCI vs. CABG) | Death/MI/CVA/revascularization | 1.00 (0.57 to 1.76) | 1.28 (0.88 to 1.86) | NR |
| BARI (PCI vs. CABG) | Death | 1.11 (0.74 to 1.67) | NR | 1,20 (0.92 to 1.59) |
| MASS II (PCI vs. CABG) | Death/MI/revascularization | 1.47 (0.87 to 2.50) | 2.04 (1.45 to 2.94) | 1.89 (1.38 to 2.56) |
| PRECOMBAT (PCI vs. CABG) | Death/MI/CVA/revascularization | 1.22 (0.48 to 3.08) | 1.65 (0.88 to 3.07) | 1.50 (0.90 to 2.52) |
CI = confidence interval; CABG = coronary artery bypass graft; NR = not reported; PCI = percutaneous coronary intervention